Medical expert of the article
New publications
Gallbladder
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
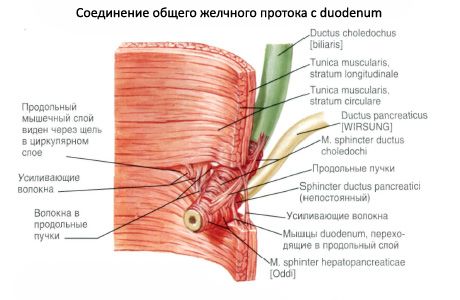
The gallbladder (vesica biliaris, s.vesica fellea) is pear-shaped, it accumulates and concentrates bile. The gallbladder is located in the right hypochondrium. Its upper surface is adjacent to the gallbladder fossa on the visceral surface of the liver. The free lower surface faces the peritoneal cavity, is covered with peritoneum and is adjacent to the anterior wall of the upper part of the duodenum. On the right, the lower surface of the gallbladder is adjacent to the right flexure of the colon. The gallbladder is shaped like a pear. The length of the gallbladder is 8-12 cm, the width is 4-5 cm, the capacity is about 40 cm 3. The gallbladder has 3 sections: the fundus, the body and the neck.
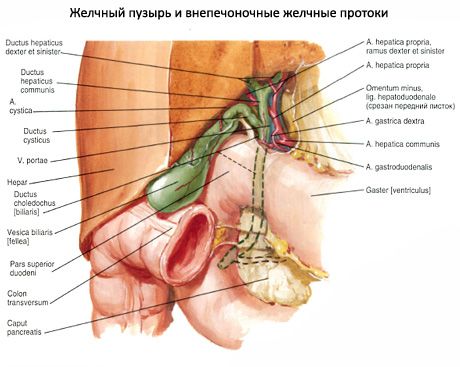
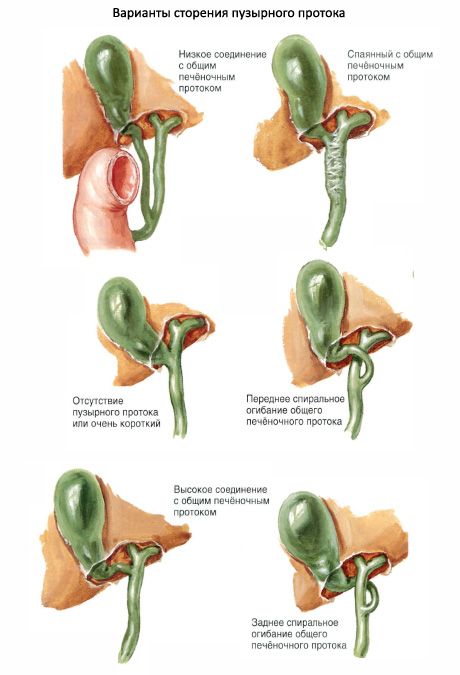
The fundus of the gallbladder (fundus vesicae biliaris) is expanded. It slightly emerges from under the lower edge of the liver at the level of the junction of the VIII and IX costal cartilages, which corresponds to the intersection of the costal arch with the right edge of the rectus abdominis muscle. The fundus of the gallbladder passes into the body (corpus vesicae biliaris), and the body passes into the neck (collum vesicae biliaris). The cystic duct (ductus cysticus) begins from the neck. The neck of the bladder is directed toward the porta hepatis and, together with the cystic duct, is located in the thickness of the hepatoduodenal ligament. At the point where the body of the gallbladder passes into its neck, a bend usually forms. Therefore, the neck is at an angle to the body of the gallbladder.
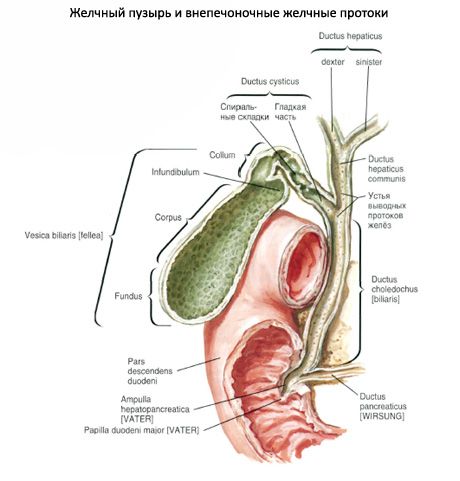
The wall of the gallbladder is formed by four layers: the mucous, muscular and serous membranes and the submucous base. The mucous membrane is thin and forms numerous small folds. A spiral fold (plica spiralis) is formed in the neck area.
The mucous membrane of the gallbladder is lined with a single-row columnar epithelium. The well-developed lamina propria of the mucous membrane contains lymphocytes and their small clusters, mucous glands, vessels and nerves. The submucosa is thin. The muscular membrane of the gallbladder is formed by one circular layer of smooth myocytes, among which there are muscle bundles of oblique and longitudinal orientation. The muscular layer is less developed in the area of the fundus, and more developed in the neck area, where it directly continues into the muscular layer of the cystic duct. Outside of the muscular membrane there is a subserous base (tela subserosa) and a serous membrane (peritoneum). The peritoneum covers the gallbladder from below and from the sides. The surface of the gallbladder facing the liver is covered with adventitia.
Innervation of the gallbladder: branches of the vagus nerves and hepatic plexus (sympathetic).
Blood supply to the gallbladder: bile duct artery (from the proper hepatic artery).
Venous outflow: bile duct vein (tributary of the portal vein).
Lymphatic drainage: hepatic and gallbladder lymph nodes.
Functions of the gallbladder
The gallbladder is an organ that performs important functions in the digestion process. Its main function is to store and concentrate bile, which is produced by the liver. Here are the main functions of the gallbladder:
- Bile Storage: The liver continually produces bile, but it is only needed for digestion after a meal. The gallbladder serves as a temporary storage reservoir for bile so that it can be released into the stomach and intestines when needed.
- Concentrating Bile: In the gallbladder, bile is concentrated, meaning that water and some other components of the bile are removed, making it more concentrated and effective for digesting fats. When fat-containing foods enter the intestines, bile is released to help digest them.
- Bile Release: When fat-rich food reaches the duodenum, the gallbladder contracts and releases concentrated bile into the intestines through the bile ducts. This helps break down fats into tiny droplets and makes them easier for enzymes to digest.
- Helps in the absorption of fats and fat-soluble vitamins: Bile helps the body absorb fats and fat-soluble vitamins (A, D, E, K) from food, as these substances cannot dissolve in water and require bile to break them down and be absorbed.
The gallbladder plays an important role in processing and digesting fats in food, which is an important step in the digestion process. The absence or dysfunction of this organ can lead to problems with digestion and absorption of nutrients.
Contractile function of the gallbladder
It involves contraction and release of bile that has been accumulated and concentrated in it. This occurs with certain signals related to the digestive process and plays a key role in the digestion of fats.
When fat-rich food enters the stomach and duodenum, receptors in the intestinal wall detect this fact and transmit signals to the gallbladder. In response to these signals, the gallbladder begins to contract, squeezing and squeezing bile through the bile ducts into the intestine. This process is called cholekinesis.
The contractile function of the gallbladder allows for precise dosing and release of concentrated bile into the intestines, where it mixes with food and helps digest fats. Bile is important for emulsifying fats, that is, breaking them down into tiny droplets so that digestive enzymes can more easily break down and absorb the fats. This process helps the absorption of nutrients, including fat-soluble vitamins (A, D, E, K), from food.
The contractile function of the gallbladder is an important link in the digestion process and allows the body to effectively absorb fats from food.
Evacuation function of the gallbladder
Associated with its ability to release concentrated bile into the duodenum when needed for fat digestion. This function plays an important role in the digestive process and is controlled by nervous and hormonal regulation.
The main aspects of the evacuation function of the gallbladder include:
- Gallbladder contraction: When food containing fat enters the stomach and duodenum, receptors in the intestinal wall detect this fact. In response to these signals, the gallbladder begins to contract (bilekinesis) and releases stored bile into the bile ducts.
- Regulation: Gallbladder contraction is regulated by the nervous and hormonal systems. The hormone cholecystokinin, released by the intestines when fat enters, stimulates gallbladder contraction. Vagus nerves and other neural mechanisms also play an important role.
- Release of Bile: Contraction of the gallbladder causes bile to be released into the duodenum, where it mixes with food and helps digest fats. Bile is important for emulsifying fats, which means breaking them down into tiny droplets so that digestive enzymes can more easily break down and absorb the fats.
The gallbladder's evacuation function allows for precise dosing and release of bile to aid in the digestion of fats. This process effectively facilitates the breakdown and absorption of fat-soluble vitamins and other nutrients from food.
Study of gallbladder functions
Various methods and procedures are used to examine the function of the gallbladder and its ability to contract and release bile. Some of these include:
- Gallbladder ultrasound: An ultrasound of the gallbladder can help evaluate its structure and size, as well as detect the presence of stones in the gallbladder or bile ducts.
- Hepatobiliary scintigraphy: This is a nuclear medicine procedure that evaluates the motor function of the gallbladder. The patient is injected with a radioactive substance, which is then collected in the gallbladder. A special scanner is then used to study the movement of the radioactive substance and evaluate how the gallbladder contracts and releases bile.
- Esophagogastroduodenoscopy (EGD): This procedure allows your doctor to evaluate your duodenum and bile ducts and look for stones or other problems.
- Functional tests: There are various functional tests that can be used to evaluate gallbladder function. For example, a gallbladder contraction test can be performed using cholecystography, magnetic resonance cholecystography, or duodenal manometry.
These tests help doctors evaluate the motor function of the gallbladder and identify any abnormalities or problems that may be affecting its function. If you have symptoms or suspect a gallbladder problem, you should see a doctor who can conduct appropriate tests and determine the best treatment or management for your condition.
Evaluation of gallbladder function
Hypomotor gallbladder function (hypokinetic function): This is a condition in which the gallbladder has a reduced ability to contract and release bile. This can lead to bile retention and problems with fat digestion. Hypomotor gallbladder function can occur due to various factors, such as insufficient fat intake in the diet, long-term adherence to low-fat diets, or slow motor activity of the gallbladder itself.
Hypermotor gallbladder function (hyperkinetic function): This is a condition in which the gallbladder contracts and releases bile excessively often or forcefully. This can lead to improper evacuation of bile and can cause symptoms such as pain or diarrhea. Hypermotor gallbladder function can be associated with various factors, including stress, strong emotional arousal, certain diets and eating habits.
Both of these conditions can cause symptoms and require evaluation and treatment by a physician or gastroenterologist. Treatment may include dietary changes, medications, or other medical procedures, depending on the specific situation.
Age-related features of the gallbladder
The gallbladder of a newborn is elongated (3-4 cm), but its bottom does not protrude from under the lower edge of the liver. By the age of 10-12 years, the length of the gallbladder increases approximately 2 times. The gallbladder is projected onto the anterior abdominal wall below the costal arch, 2 cm to the right of the anterior midline. Below the gallbladder are the duodenum, loops of the mesenteric part of the small intestine and the transverse colon. The gallbladder acquires its final dimensions by the age of 20-25 years. In old age, local thinning of the gallbladder walls appears, bay-like protrusions of its walls are formed (especially above the area of its neck).


 [
[