Medical expert of the article
New publications
Tracheitis in a baby
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
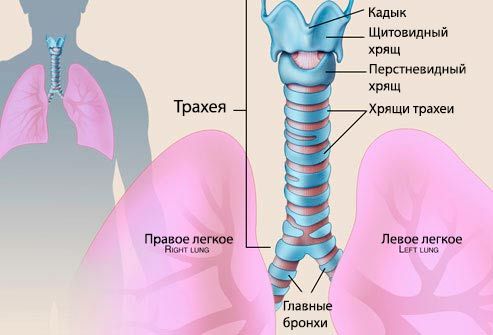
Inflammation of the mucous membrane of one of the important parts of the respiratory tract – the trachea – is called tracheitis.
The inflammatory process can be provoked by banal hypothermia, but most often tracheitis in a child develops against the background of a viral infection (flu), measles or whooping cough, since the child's body is extremely vulnerable and susceptible to all kinds of viruses and infections.
Causes tracheitis in a child
Acute tracheitis in children develops as a result of the aggressive impact of a virus or bacterial infection on the epithelium of the tracheal mucosa. Most often in pediatric clinical practice, inflammation of the trachea is caused by the influenza virus or pneumococci, less often by staphylococci. Acute tracheitis in children can also be provoked by the following reasons:
- Insufficient humidity in the room where the child is constantly located.
- Too cold air that the child breathes for a long time.
- Severe hypothermia.
- Allergic reaction.
- Some types of cardiac pathologies.
- General unfavorable environment surrounding the child – parents smoking indoors, poor ecology, and so on.
Chronic tracheitis in children most often develops against the background of an undetected and untreated respiratory infection, or when acute tracheitis is combined with an inflammatory process in the bronchi (tracheobronchitis). Chronic tracheitis in children can also be provoked by the following factors:
- diseased teeth in which a bacterial infection develops;
- chronic bacterial infection in the nasopharynx;
- chronic tonsillitis;
- adenoids;
- allergy;
- the child's constant presence in a room with smoking adults (passive smoking).
Allergic tracheitis can be triggered by an allergic reaction. Most often, the factor activating allergic tracheitis in children is an aggressive response of the immune system to antigens of household dust, pet hair. Much less often, the cause of allergic tracheitis can be food allergens or drug allergies.
Tracheitis in infants can be associated with many factors, but the main cause is the vulnerability of the unformed mucous epithelium and a viral infection. Much less often, tracheitis in infants is associated with dry air in the room, that is, with insufficient humidity.
Just like tracheitis, laryngitis is an inflammatory process, only one that occurs in the larynx. The causes that provoke tracheitis and laryngitis are almost identical:
- Hypothermia.
- Dry or smoky air in a room where a child is constantly located.
- Acute respiratory infection.
- Allergy.
- Physiological irritation of the ligaments, and then the mucous membrane of the larynx and trachea due to vocal strain. In adults, these are typical diseases of teachers, actors or lecturers. In children, the cause may be prolonged screaming or crying.
The inflammation spreads to the mucous epithelium of the epiglottis, then the larynx, the oral cavity and ligaments become inflamed. Also, tracheitis and laryngitis in children can develop against the background of a chronic infectious process in the nasopharynx or in the oral cavity. Inflammation of the tonsils, adenoids, chronic sinusitis and even bad teeth are a potential source of constant infection of the mucous membranes of the larynx and trachea.
Symptoms tracheitis in a child
Signs of tracheitis in children are manifested by pronounced symptoms that are impossible not to notice. First of all, it is a dry, debilitating cough. Coughing attacks are most active at night, when the child takes a horizontal position and relaxes. Coughing shocks can be so frequent that they sometimes cause vomiting. The child does not get enough sleep, becomes lethargic, irritable. During the day, the cough is a little less frequent, it is more like a cough. Unlike adults, children react to tracheitis with an elevated body temperature. Hyperthermia can reach high values, up to 39 degrees, which, combined with a constant cough, poses a real threat to babies, especially infants. Signs of tracheitis in children, as a rule, immediately alert attentive parents and encourage them to consult a doctor. If timely treatment is not started, tracheitis can develop into tracheobronchitis and even bronchopneumonia.
The main specific symptom of tracheitis is a persistent dry and frequent cough. Coughing most often occurs at night, less often during the day. Other symptoms of tracheitis in children may be as follows:
- Subfebrile body temperature in chronic tracheitis.
- High body temperature (up to 38-39 degrees) in the acute form of the disease.
- General weakness of the body up to exhaustion.
- Rapid breathing, respiratory failure.
- Stridor is noise when breathing.
- During coughing attacks, typical intercostal retractions are observed – compression of the ribs.
- Hoarseness of the voice, even to the point of loss of voice (dysphonia).
- Lowering of the voice timbre.
- Reflexive urge to vomit.
- Headache.
- Decreased appetite.
- Complaints of a burning sensation in the chest area.
Symptoms of tracheitis in children, as well as adults, are quite specific, they are difficult to confuse with signs of another disease. In addition, when listening, the doctor never detects noises or other changes in the lungs, with the exception of tracheobronchitis, when dry wheezing can be heard in the bronchi.
Cough with tracheitis in a child
Cough is a reflex defense mechanism of the body, which is triggered by the slightest irritation of the receptors of the larynx or trachea. Cough with tracheitis in a child is a unique way to remove sputum accumulated there from the tracheal branches. Characteristic features of cough with tracheitis are frequency (sometimes up to 20 coughing fits in a row), dryness - without sputum secretion, pain in the retrosternal space. Quite often, the inflammatory process in the trachea spreads to the bronchi, the throat also becomes inflamed, so cough with tracheitis in a child can be quite strong, persistent. A typical cough, characteristic of tracheitis, is night attacks, sometimes so long that they literally do not allow either the child or the parents to sleep. Since the secretion of sputum is difficult, a dry cough can cause a gag reflex. A simple sigh, throwing back the head, laughing or even crying can provoke a cough in a child with tracheitis.
Acute tracheitis in children is manifested by severe swelling of the mucous epithelium of the trachea, which leads to an increase in temperature, the release of viscous secretory fluid and almost immediately - to a characteristic dry cough. Cough with tracheitis is the leading clinical sign, most often it is activated at night or early in the morning.
Acute tracheitis is quite often combined with catarrhal laryngitis – inflammation of the larynx, as well as rhinitis.
Symptoms of chronic tracheitis are less intense than in the acute form of the disease, but a typical sign is a dry cough. A child's cough looks like a constant coughing, which over time becomes more intense, the voice may change (low timbre, hoarseness). If treatment is not started, the cough develops into night attacks, into obsessive coughing series, which most often occur at night. Chronic tracheitis in children is almost always accompanied by pronounced symptoms, so it is impossible not to notice it. Attentive parents at the first alarming signs similar to the manifestations of tracheitis should immediately show the child to a doctor.
Allergic tracheitis in children is manifested by pronounced edema and hyperemia of the mucous epithelium of the trachea, itching, and a sore throat. Just like with other types of tracheitis, the main symptom is a characteristic dry, persistent cough. A child's cough can be provoked by a simple sigh, sobbing while crying, or laughter. Unlike other types, allergic tracheitis in children is manifested by both night and daytime chronic cough. The child's condition gradually worsens, subfebrile temperature and general weakness appear, since breathing is shallow and frequent: with tracheitis, a child makes up to 25 respiratory movements per minute, with a norm of 14-17. Constantly accumulating sputum is not released, but only provokes another coughing attack.
A feature of tracheitis in infants is the fact that the baby is not able to complain about his poor condition, the main criterion for the success of treating tracheitis in newborns is the attentive attitude of parents and timely diagnosis of the disease. Any attacks of night coughing in a baby should alert the mother. Tracheitis in an infant manifests itself in the form of rapid breathing, in addition to coughing, a sign of the disease can be a hoarse voice of the baby when he cries. If mucus accumulates in the tracheal branches, the child tries to "cough it up", but due to the underdevelopment of the cough reflex, sputum can return to the baby's body again. Tracheitis can also be accompanied by an inflammatory process in the bronchi, which only complicates the child's condition. The main danger of tracheitis in newborns is the risk of respiratory failure up to asphyxia.
The symptoms of tracheitis in small children under one year are almost identical to the signs of the disease in adults. There is only one difference - tracheitis in children under one year is usually much more severe and most often in an acute form. In addition, a small child is not yet able to complain and specify his condition, he becomes irritable, capricious. The main symptom of tracheitis in babies is a characteristic night cough, which manifests itself in attacks accompanied by holding the breath. The cough is frequent, shallow, long-lasting, there is usually no sputum. Coughing attacks can be so long that they cause vomiting. Quite often, tracheitis in children under one year is provoked by a viral infection, so inflammation of the trachea is combined with a runny nose and laryngitis. The baby's throat becomes inflamed, there may be a fairly high temperature.
Tracheitis and laryngitis in children in combination with each other are most often accompanied by a fairly high body temperature, sometimes reaching 39 degrees. The child loses appetite, weakens, his breathing becomes shallow and rapid. Respiratory failure is manifested in pale skin, a bluish tint of the lips. Sometimes such a pathological "union" of laryngitis and tracheitis is considered grounds for hospitalizing the baby.
Where does it hurt?
What's bothering you?
Forms
Types of tracheitis can be as follows:
- Acute - with pronounced symptoms in the form of a characteristic cough, most often acute tracheitis is accompanied by laryngitis, rhinitis and pharyngitis. Quite often the acute form of the disease is combined with an inflammatory process in the bronchi (tracheobronchitis).
- Chronic – develops from the acute form, less often it is a primary disease. Chronic tracheitis in a child also has subtypes:
- Hypertrophic form – dilation of the vessels of the tracheal branch.
- Atrophic form – thinning of the mucous membrane of the upper respiratory tract.
What do need to examine?
How to examine?
What tests are needed?
Who to contact?
Treatment tracheitis in a child
Treatment of tracheitis in children is usually carried out without the use of antibiotics, if the disease is not associated with a bacterial infection. Since tracheitis significantly depletes many functions of the body, treatment should be as comprehensive as possible, and at the same time gentle. Acute tracheitis diagnosed in a timely manner is treated much faster than chronic tracheitis, which is more difficult to treat with therapeutic measures.
Treatment of tracheitis in a child goes through the following stages:
- The factor or cause that provokes the inflammatory process in the tracheal mucosa is eliminated – a respiratory disease, virus, bacterial infection, allergy, and so on.
- Threatening symptoms are relieved: antipyretics are used at high temperatures, expectorants to activate sputum secretion. Warm wraps, rubbing, mustard plasters (in the absence of fever) are indicated.
- Inhalations and physiotherapy procedures are effective.
- Measures are being taken to strengthen the immune system.
Treatment of tracheitis in a child can be quite lengthy, in which case the doctor makes a plan of therapeutic measures, which parents must strictly follow. This is especially true for tracheitis in newborn babies.
The room where the sick child is located must have a certain humidity level and be cleaned daily. It is also necessary to eliminate all irritants - smoke, including cigarette smoke, the use of all kinds of chemicals and fragrances. A sick child needs much more attention in the sense that any vocal strain - crying, talking can aggravate irritation of the tracheal mucosa, so the baby needs to be constantly distracted and calmed down.
Treatment of tracheitis in a child also involves the use of herbal remedies, which can successfully replace drug therapy. Decoctions of coltsfoot, chamomile, linden, and licorice root are extremely effective if prepared according to the recommended recipe.
What can be done at home?
- If the child is over two years old, you can put mustard plasters on the area between the shoulder blades or the sternum. Mustard plasters cannot be used if the child has a fever, and the procedure should be warming, not burning, so mustard plasters are applied to cotton or linen fabric, not to the bare body.
- You can use warming wraps, compresses with hot boiled potatoes or rubbing. Rubbing is especially effective for infants. The procedure is best done half an hour before bedtime.
- The child needs to drink a lot. It is better if these are herbal infusions, for example, chamomile or calendula. Cranberry juice or rosehip infusion will strengthen the immune system and help to remove intoxication from the child's body faster.
Medicines for tracheitis for children
Medicines for tracheitis for children are, as a rule, all sorts of syrups and herbal decoctions. Pediatricians try to prescribe antibiotics and antiviral drugs with extreme caution, especially when it comes to very young infants.
Expectorant tablets are also effective, such as Ambroxol or Lazolvan, which is prescribed as a mucolytic even to newborns. All kinds of breast elixirs, herbal expectorant infusions and teas are also an excellent medicine for tracheitis in children. In addition, antipyretic drugs based on paracetamol can be prescribed as symptomatic therapy. If tracheitis is viral in nature, antiviral drugs are prescribed. Immunal, Anaferon help not only with flu, but also as a medicine for tracheitis in children. The following drugs are prescribed as mucolytic syrups - "Doctor Mom", Flavamed, Gedelix, for children over three years old, Bromhexine, ACC relieves cough.
Antibiotics for tracheitis in children
Antibiotics for tracheitis in children are usually not prescribed. An exception may be a combination of tracheitis with bronchitis or if the disease has a bacterial cause. If tracheitis is caused by a bacterial infection, a local antibiotic may be prescribed - Bioparox, which is used by inhalation through the mouth, less often through the nose. Bioparox cannot be prescribed to children under three years of age, in addition, the drug has some other contraindications. Also, antibiotics for tracheitis in children can be prescribed in the case of a protracted nature of the disease, when chronic tonsillitis worsens, or the disease is accompanied by otitis, sinusitis. The drug of choice may be the latest generation antibiotic Azithromycin, which can be used even for infants in the form of a suspension. Like many other macrolides, Azithromycin has a broad spectrum of action and is used once a day.
 [ 12 ]
[ 12 ]
Inhalations for tracheitis in children
The most effective way to help relieve cough symptoms is inhalation. Inhalations for tracheitis in children should be used no earlier than the second, and preferably the third day after the onset of the disease. Decoctions or syrups of licorice root, chest pharmacy fees are suitable for inhalation. It is best to inhale with a herbal remedy containing essential oils, these include eucalyptus, sage, mint and all coniferous trees. Of course, many children actively resist this procedure, so inhalations for tracheitis in children can be carried out in the following ways:
- A baby can be bathed in water with a decoction of essential herbs. In warm water, the healing ethers begin to evaporate and your baby will inevitably inhale these vapors. You can also put a container with the decoction on the fire, close the windows and doors in the room and stay with the baby next to the gradually evaporating liquid. Another option is to put a saucepan with a hot decoction near the baby's crib so that the air is saturated with healing vapors.
- For an older child, you can prepare a hot decoction of the indicated herbs in a small container and ask him to breathe in the steam for a few minutes.
- Children over three years of age are quite capable of breathing over a regular steam or ultrasonic inhaler.
Inhalations for tracheitis in children should not exceed 5-10 minutes, and they do not replace other treatments prescribed by the attending physician.
How to cure tracheitis in a child?
How to cure tracheitis in a child if the symptoms do not disappear and the disease becomes protracted and chronic? The fact is that many parents, carried away by self-medication, uncontrollably give their child expectorants bought at a pharmacy, which are sometimes completely ineffective in treating tracheitis. The first thing to do if signs of the disease are noticed is to contact a pediatrician to rule out other, more serious diseases - bronchitis, pneumonia or whooping cough.
In addition, the question of how to cure tracheitis in a child can really only be answered by the attending physician, who will prescribe the necessary cough syrup or other medication that is adequate to the symptoms.
More information of the treatment
Drugs

