Medical expert of the article
New publications
Trachea
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
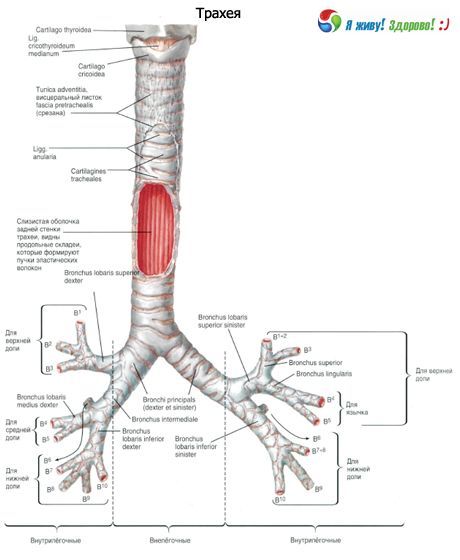
The trachea is a hollow tubular organ that serves to pass air into and out of the lungs. In an adult, the trachea begins at the level of the lower edge of the sixth cervical vertebra, where it joins the larynx (at the level of the cricoid cartilage), and ends at the level of the upper edge of the fifth thoracic vertebra. The average length of the trachea in an adult is 12 cm (from 8.5 to 15 cm), the number of tracheal rings varies from 15 to 20 (the maximum number is 26). The width of the trachea varies from 17 to 19 mm.
In a child, the beginning of the trachea corresponds to the IV-V cervical vertebra, and the bifurcation of the trachea is at the level of the III-IV thoracic vertebra.
The minimum size of the trachea corresponds to the exhalation phase, the maximum - to the inhalation phase. During a cough push, the lumen of the trachea decreases by 3-10 times depending on the age of the person (the younger, the more the lumen of the trachea narrows).
The trachea is located in the anterior region of the neck (cervical region, pars cervicalis) and in the mediastinum of the thoracic cavity (thoracic region, pars thoracica)), the border between which runs along a transverse line drawn through the upper aperture of the chest. The cervical region accounts for 1/3, and the thoracic region for 2/3 of the total length of the trachea.
Topographically, the trachea is closely related to the organs of the anterior neck. In front of the cervical part of the trachea are the lower part of the thyroid gland, the pretracheal plate of the cervical fascia, the sternohyoid and sternothyroid muscles of the neck. The esophagus is adjacent to the trachea behind. On the sides are a paired vascular-nerve bundle, which includes the common carotid artery, the internal jugular vein and the vagus nerve.
The bifurcation of the trachea is adjacent to the aortic arch, the brachiocephalic trunk and the brachiocephalic vein, as well as to the initial part of the left common carotid artery. The posterior wall of the trachea is adjacent to the esophagus along its entire length, from which it is separated by a layer of cellular tissue. On the right and left between the trachea and the esophagus, the esophageal-tracheal grooves are formed, in which the recurrent nerves and inferior laryngeal arteries pass.
Along the trachea in front are the suprasternal, interaponeurotic, pretracheal and paratracheal spaces. In the pretracheal cellular space is located the unpaired venous plexus of the thyroid gland and in 10-20% of cases - an additional branch from the aorta, directed to the thyroid gland (inferior thyroid artery - a. thyroidea ima). In the paratracheal cellular space on the right are the lymph nodes, vagus nerve, cardiac branches of the border sympathetic trunk, on the left - branches of the border trunk, thoracic duct.
At the level of the 5th thoracic vertebra, the trachea divides into the right and left main bronchi. At the site of division of the trachea, a fork is formed - bifurcation (bifurcatio trachea). At the junction of the medial walls of the main bronchi, a small protrusion is revealed, called a spur, keel or carina (carina tracheae). The angle of bifurcation of the trachea is on average 70°. During inhalation, the bifurcation of the trachea shifts downward and forward by 2-3 cm.
The wall of the trachea consists of the mucous membrane, submucosa, fibrocartilaginous and adventitial membranes.
The mucous membrane of the trachea is lined with pseudo-stratified multi-row columnar (cylindrical) epithelium lying on the basal membrane. The epithelial cover is dominated by ciliated epithelial cells, which have an average of 250 cilia. The movements of the cilia are directed upward, towards the larynx. In the covering epithelium of the trachea there is a significant number of goblet cells that secrete mucus. There are also basal (stem) cells, endocrinocytes (secrete norepinephrine, serotonin, dopamine) and some other types of epithelial cells. The proper plate of the mucous membrane is rich in longitudinally located elastic fibers, lymphoid tissue. In the thickness of the proper plate there are individual smooth myocytes, located mainly circularly. The excretory ducts of numerous tracheal glands (gll.tracheales) pass through the proper plate of the mucous membrane, the secretory sections of which are located in the thickness of the submucosa.
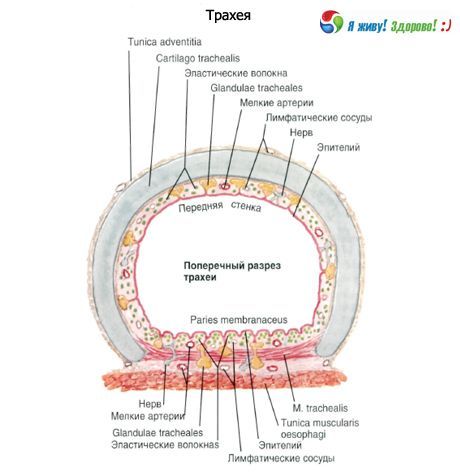
The submucosa of the trachea, represented by loose fibrous connective tissue, contains vessels, nerves, clusters of lymphoid cells and individual lymphocytes.
The fibrocartilaginous membrane of the trachea is represented by 16-20 hyaline cartilages (cartilagines tracheales). Each cartilage has the form of an arc occupying 2/3 of the circumference of the trachea and not closed at the back. The cartilages are connected to each other by narrow annular ligaments (ligg.annularia), passing into the perichondrium covering the cartilages of the trachea. The posterior membranous wall (paries membranaceus) of the trachea is formed by dense fibrous connective tissue, contains bundles of myocytes. The trachea is covered from the outside by the adventitia.
Age-related features of the trachea and main bronchi
In a newborn, the trachea is 3.2-4.5 cm long. The lumen width in the middle part is about 0.8 cm. The membranous wall of the trachea is relatively wide, the tracheal cartilages are poorly developed, thin, soft. In old age (after 60-70 years), the tracheal cartilages become dense, fragile, and easily break when compressed.
After birth, the trachea grows rapidly during the first 6 months, then its growth slows down and accelerates again during puberty and adolescence (12 years-22 years). By 3-4 years of age, the width of the tracheal lumen increases by 2 times. The trachea of a child aged 10-12 is twice as long as that of a newborn, and by 20-25 years its length triples.
The mucous membrane of the trachea wall in a newborn is thin and delicate; the glands are poorly developed. In a newborn, the trachea is located high. Its beginning is at the level of the II-IV cervical vertebrae, and the bifurcation of the trachea corresponds to the II-III thoracic vertebrae. In a child of 1-2 years, the upper edge of the trachea is located at the level of the IV-V cervical vertebrae, at 5-6 years - in front of the V-VI vertebrae, and in adolescence - at the level of the VI cervical vertebra. By the age of 7, the bifurcation of the trachea is in front of the IV-V thoracic vertebrae, and after 7 years it gradually settles at the level of the V thoracic vertebra, as in an adult.
The right main bronchus in a newborn departs from the trachea at a smaller angle (26°) than the left (49°), and in its direction is like a continuation of the trachea. The main bronchi grow especially quickly in the first year of a child's life and during puberty.


 [
[