Medical expert of the article
New publications
Testicular torsion
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
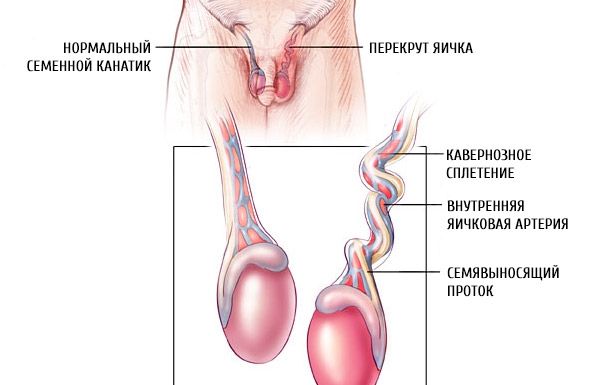
Testicular torsion is an abnormal twisting of the spermatic cord caused by rotation of the mesorchium (the fold between the testicle and its appendage), which leads to strangulation or necrosis of the testicular tissue.
Epidemiology
Testicular torsion occurs with a frequency of 1 in 500 patients in urological clinics.
In the first 10 years of life, testicular torsion is observed in 20% of cases, and after 10 years and before puberty - in 50%. Thus, the main place in the etiopathogenesis of acute testicular diseases in children is occupied by mechanical factors, such as testicular torsion.
Causes testicular torsion
The provoking factor of testicular torsion can be trauma and bruises of the scrotum, sudden movements, abdominal tension, which leads to a reflex contraction of the muscle that lifts the testicle. The absence of normal attachment of the testicle to the bottom of the scrotum - an anomaly that occurs during the period of attachment of the epididymis to the testicle - leads to a violation of mutual fixation, which entails the separation of these two formations. The testicle is subject to torsion in case of developmental defects associated with a violation of its migration into the scrotum (cryptorchidism).
Pathogenesis
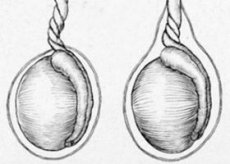
The testicle rotates around the vertical axis. If the rotation of the testicle together with the spermatic cord exceeds 180°, blood circulation in the testicle is disrupted, numerous hemorrhages form, thrombosis of the veins of the spermatic cord occurs, serous-hemorrhagic transudate occurs in the cavity of the proper membrane of the testicle; the skin of the scrotum becomes edematous.
Extra-vaginal or supra-testicular torsion of the testicle occurs together with its membranes. The testicle is located mesoperitoneally in relation to the vaginal process of the peritoneum and its fixation is not impaired. The decisive role in the development of this form of testicular torsion is played not by its developmental defect, but by the morphological immaturity of the spermatic cord and surrounding tissues - hypertonicity of the muscle that lifts the testicle, loose adhesion of the membranes to each other, a short wide inguinal canal that has an almost straight direction.
Intravaginal, or intratunical, testicular torsion (intravaginal form) occurs in the cavity of the vaginal membrane. It is observed in children over 3 years of age, especially at the age of 10-16 years. In this case, testicular torsion occurs as follows. When the muscle that lifts the testicle contracts, it, together with the surrounding membranes, is pulled upward and makes a rotational movement. The rigidity and density of the adhesion of the membranes, as well as the inguinal canal, which intimately embraces the spermatic cord in the form of a tube (in older children), do not allow the testicle to make a full rotation around the axis, so at some point the rotation stops.
The testicle, which has a long mesentery and therefore has high mobility inside the cavity of the vaginal process of the peritoneum, continues to rotate by inertia. Then the muscle fibers relax. The testicle, raised to the upper part of the scrotal cavity, is fixed and held by its convex parts in a horizontal position. With further contraction of the muscle that lifts the testicle, the torsion continues. The longer the mesentery and the greater the force of contraction of the muscle that lifts the testicle, and the greater the mass of the testicle, the more pronounced the degree of torsion.
The authors explain the increase in the frequency of intravaginal torsions in the prepubertal and pubertal periods by the disproportionate increase in testicular mass at this age. This indicates that in the mechanism of intravaginal testicular torsion, along with other factors, a certain role is played by the disproportion in the growth of the reproductive system.
Symptoms testicular torsion
Testicular torsion has acute symptoms. They manifest themselves as sharp pains in the testicle, in the corresponding half of the scrotum, radiating to the groin area; sometimes accompanied by nausea, vomiting and a collapsed state.
Symptoms of testicular torsion depend on the duration of the disease and the age of the child. In newborns, testicular torsion is most often detected during the initial physical examination as a painless enlargement of half of the scrotum. Hyperemia or blanching of the skin of the scrotum, as well as hydrocele, are often noted. Infants are restless, cry, and refuse to breastfeed. Older children complain of such symptoms of testicular torsion as: pain in the lower abdomen and in the groin area. A painful tumor-like formation appears at the external inguinal ring or upper third of the scrotum. Later, the twisted testicle appears elevated and when trying to raise it even higher, the pain intensifies (Prehn's symptom).
Complications of testicular torsion and its hydatid
The problem of prevention, timely diagnosis and treatment of acute diseases of the scrotum organs is of great importance. Firstly, 77-87.3% of patients are people of working age from 20 to 40 years; secondly, 40-80% of patients who have suffered acute diseases of the scrotum organs experience atrophy of the spermatogenic epithelium and, as a consequence, infertility. Conservative treatment of testicular torsion ends with testicular atrophy, and later surgical treatment either removes the testicle or appendage, or also its atrophy.
Causes of testicular atrophy after orchiepididymitis:
- direct damaging effect of the etiological factor on the parenchyma;
- violation of the hematotesticular barrier with the development of autoimmune aggression;
- development of ischemic necrosis.
Clinical and morphological studies have revealed that in all forms of acute diseases of the scrotum organs, largely identical processes occur. manifested by a characteristic clinical picture and neurodystrophic changes in the tissue. Acute diseases of the scrotum organs cause mainly identical disorders of spermatogenesis, expressed in pathospermia, a violation of the content of trace elements in the ejaculate, a decrease in the area of the nucleus and head of spermatozoa, and a decrease in the content of DNA in them.
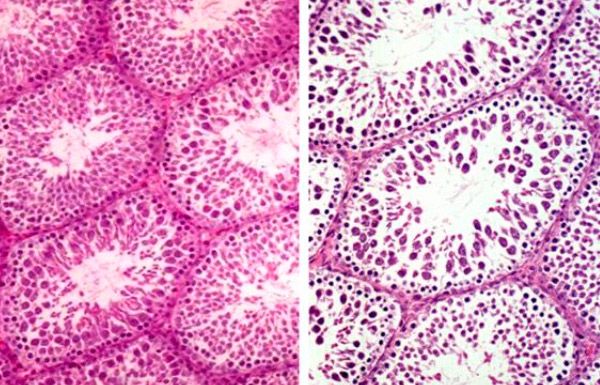
Ischemic necrosis is a consequence of parenchyma edema, its protein coat. All this justifies the tendency that has emerged in recent years for early surgical treatment of acute diseases of the scrotum organs, as it allows for rapid elimination of ischemia, timely detection of the disease, thereby preserving the functional capacity of the testicle. Early surgical treatment is indicated for severe pain, development of reactive hydrocele of the testicle, purulent inflammation and suspected rupture of the scrotum organs, torsion of the testicles, hydatid and its appendage.
Where does it hurt?
Forms
There are two forms of testicular torsion.
- Extravaginal testicular torsion (above the attachment of the parietal layer of the vaginal process of the peritoneum) is observed in children under 1 year of age;
- Intravaginal testicular torsion - occurs more often in children than in adults.
Diagnostics testicular torsion
A thorough medical history should be obtained. Recent scrotal trauma, dysuria, hematuria, urethral discharge, sexual activity, and time since onset of clinical manifestations should be noted.
 [ 22 ], [ 23 ], [ 24 ], [ 25 ]
[ 22 ], [ 23 ], [ 24 ], [ 25 ]
Clinical diagnosis of testicular torsion
It is necessary to examine the abdominal cavity, genitals and perform a rectal examination. Particular attention should be paid to the presence or absence of discharge from the urethra, the position of the affected testicle and its axis, the presence or absence of a hydrocele on the opposite side, the presence of induration or excess tissue in the testicle or its appendage, and changes in the color of the scrotum.
The testicle is usually palpated at the upper edge of the scrotum, which is associated with shortening of the spermatic cord. The scrotum is slightly painful upon palpation. Sometimes, with torsion, the appendage is located in front of the testicle. The spermatic cord is thickened due to torsion. Subsequently, swelling and hyperemia of the scrotum are observed. Due to impaired lymph drainage, there is secondary hydrocele.
 [ 26 ]
[ 26 ]
Laboratory diagnostics of testicular torsion
To rule out infection, a urine test must be done.
Instrumental diagnostics of testicular torsion
With Doppler ultrasound, the architecture of the testicle and its appendage is clearly visible; an experienced physician can obtain evidence of the presence or absence of blood flow in the testicle.
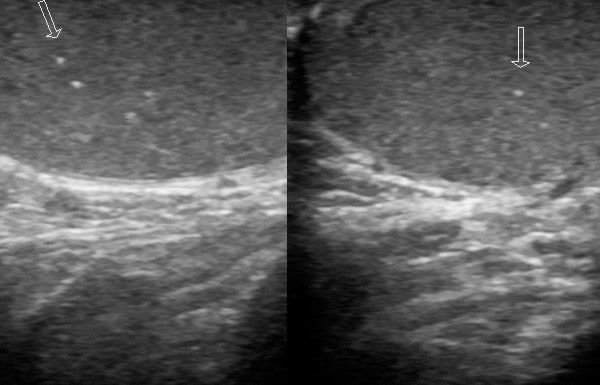
Echographically, testicular torsion is characterized by non-homogeneity of the parenchyma image with random alternation of hyper- and hypoechogenic areas, thickening of the scrotal integumentary tissues, edematous hyperechogenic appendage, and a small volume of hydrocele. At an early stage, changes may not be detected echographically when scanning in gray scale mode, or they may be non-specific (change in echo density). Later, a change in structure is recorded (infarction and bleeding). Comparative studies have shown that a testicle with unchanged echo density during surgery is viable, while hypoechogenic or heterogeneous in echogenicity testicles are non-viable.
All other echographic signs (size, blood supply and thickness of the scrotal skin, presence of reactive hydrocele) are prognostically insignificant. It is necessary to use tissue (energy) Doppler mapping. The study must be carried out symmetrically to identify minimal changes, such as in incomplete torsion or spontaneous resolution. In the affected organ, the blood flow is depleted and is not even completely determined (with inflammation, the blood flow increases). Spontaneous elimination of torsion leads to a reactive increase in blood flow, clearly visible in comparison with previous studies.
In order to determine the nature of the contents of the membranes (blood, exudate), diaphanoscopy and diagnostic puncture are performed.
 [ 30 ]
[ 30 ]
What do need to examine?
Differential diagnosis
Differential diagnostics of testicular torsion is performed with orchitis (testicular inflammation), which complicates infectious mumps, and allergic Quincke's edema. With the latter, as a rule, the entire scrotum is enlarged, the fluid soaks all its layers, forming a water bubble under the thinned skin.
Who to contact?
Treatment testicular torsion
Non-drug treatment for testicular torsion
In 2-3% of patients, torsion can be eliminated in the first hours of the disease by performing external manual detorsion.
External manual testicular detorsion
The patient is placed on his back; detorsion is performed in the direction opposite to the testicular inversion. It should be remembered that the right testicle rotates clockwise, the left counterclockwise. A convenient reference point when choosing the direction of testicular untwisting is the median suture of the scrotum. The testicle with the scrotal tissues is grasped and rotated 180° in the direction opposite to the median suture of the scrotal skin. At the same time, a slight downward traction of the testicle is performed. After this, it is lowered and the manipulation is repeated several times.
If detorsion is successful, the pain in the testicle disappears or is significantly reduced. It becomes more mobile and takes its normal position in the scrotum. If conservative detorsion is ineffective within 1-2 minutes, the manipulation is stopped and the patient is operated on. The earlier the detorsion is performed and the older the child, the better the result of the operation.
 [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ]
[ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ]
Surgical treatment of testicular torsion
If ultrasound cannot be performed or the results are unclear, then surgical intervention is indicated.
In case of swollen scrotum syndrome, urgent surgery is necessary, since the testicle is very sensitive to ischemia and can quickly die (irreversible changes occur within 6 hours).
The choice of access depends on the form of torsion and the age of the child. In newborns and infants, inguinal access is used, since they have a predominantly extravaginal form of torsion. In older children and adults, the intravaginal form predominates, so access through the scrotum is more convenient.
Technique of surgery for testicular torsion
In all cases, the testicle is exposed to the tunica albuginea, which allows for a wide resection, and the form of the torsion is determined. The testicle is dislocated into the wound, detorsion is performed, and its viability is assessed. To improve microcirculation and determine the safety of the testicle, it is recommended to inject 10-20 ml of 0.25-0.5% procaine (novocaine) solution with sodium heparin into the spermatic cord. If blood circulation does not improve within 15 minutes, orchiectomy is indicated. To improve blood circulation, heat compresses with isotonic sodium chloride solution are used for 20-30 minutes. When blood circulation is restored, the testicle acquires its normal color.
The testicle is removed only in case of its complete necrosis. If it is difficult to decide on the viability of the affected testicle. Ya.B. Yudin. A.F. Sakhovsky recommend using transillumination examination of the testicle on the operating table. Transillumination of the testicle indicates its viability. In the absence of the transillumination symptom, the authors recommend making an incision in the protein coat of the testicle at the lower pole; bleeding from the vessels of this coat indicates the viability of the organ.
The necrotic testicle, despite measures to improve its vascularization, does not change color. There is no pulsation of the vessels below the site of strangulation, the vessels of the protein coat do not bleed. The preserved testicle is sutured to the scrotal septum with two or three sutures behind the lower ligament of the appendage without tensioning the elements of the spermatic cord.
A drainage tube is inserted into the wound as in acute orchiepilidimitis and constant irrigation with antibiotics is established for 2-3 days, depending on the severity of destructive changes and the inflammatory process.
In case of testicular torsion in cryptorchidism, the above-described measures are carried out after detorsion. The atrophied testicle is removed, the viable testicle is lowered into the scrotum and fixed.
Further management
In the postoperative period, patients are prescribed sensitizing agents, physiotherapy, drugs that normalize microcirculation in the damaged organ (daily novocaine blockade of the spermatic cord, intramuscular administration of sodium heparin, rheopolyglucin, etc.). To reduce the permeability of the hemotesticular barrier in the postoperative period, patients are prescribed acetylsalicylic acid (0.3-1.5 g per day) for 6-7 days.
If necessary, preventive orchidopexy from the opposite side can be used in future practice to prevent testicular torsion.
It has been proven that if a dead testicle is preserved in the late stage of the disease, sperm antibodies appear in the patient’s body, testicular torsion spreads to the contralateral testicle, which ultimately leads to infertility.

