Medical expert of the article
New publications
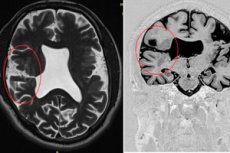
Schizencephaly of the brain
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The formation of abnormal clefts in the thickness of the cerebral hemispheres – schizencephaly of the brain (from the Greek schizo – to split, to divide and enkephalos – brain) – is one of the congenital cerebral defects. [ 1 ]
Epidemiology
Clinical statistics estimate the incidence of schizencephaly at one case per 65-70 thousand births. The estimated prevalence is 1.48 per 100,000 births. The open type of anomaly is detected 2.5 times more often. Closed schizencephaly is bilateral in 40-43% of cases, and open - in almost 80%.
In almost all patients with unilateral open cleft cerebral hemispheres, the head is asymmetrical; in bilateral schizencephaly, asymmetry is observed in approximately 60% of cases.
According to some data, this defect is most often detected in childhood, on average, at the age of 5-6 years.
Causes schizencephaly
Although the exact etiology of schizencephaly, as one of the malformations of the brain, is unknown, its connection with a number of factors is obvious - both non-genetic and genetic. The main reasons for which there may be schizencephaly of the brain in a newborn are associated with disturbances in its prenatal formation - migration of neuroblasts during the period of embryogenesis and early morphogenesis.
Schizencephaly can be caused by intrauterine infection of the fetus with cytomegalovirus (herpes virus type 5), which is asymptomatically present in the mother and, reactivating in the body of the unborn child, can affect the brain, as well as the spinal cord, eyes, lungs and gastrointestinal tract. Read more - Cytomegalovirus during pregnancy
Deviations in brain development can be caused by hypoxia – oxygen starvation of the fetus or intracranial hemorrhage – antenatal stroke, which, as studies have shown, is most often caused by mutations in the COL4A1 gene on chromosome 13, encoding type IV collagen – the main protein of the basal membranes of body tissues, including the endothelium of blood vessels. Mutations identified in this gene cause pathology of small cerebral vessels and stroke in the fetus. In addition, disruption of the type IV collagen network during intrauterine development negatively affects cell migration, proliferation and differentiation. [ 2 ]
A link has also been established between schizencephaly and germline mutations in the EMX2 homeobox gene (on chromosome 10), [ 3 ] which regulates morphogenesis and is expressed in dividing neuroblasts of the developing cerebral cortex; the SIX3 gene (on chromosome 2), encoding the protein transcription factor SIX3, which plays an important role in the development of the embryonic forebrain (prosencephalon); and the SHH gene (on chromosome 7), [ 4 ] which encodes a ligand for a protein signaling pathway involved in the morphogenesis of the cerebral hemispheres.
Risk factors
In addition to sporadic gene mutations or possible inheritance of a defective gene, experts consider the teratogenic effects of alcohol and drugs, as well as antiepileptic drugs (anticonvulsants) used during pregnancy, some anticoagulants, and retinoic acid (synthetic vitamin A) preparations to be risk factors for schizencephaly. [ 5 ], [ 6 ]
In addition to cytomegalovirus, the threat of developing congenital brain defects is posed by HSV 1 - herpes simplex virus type 1, herpes virus type 3 - Varicella zoster virus (chickenpox virus) and the virus of the genus Rubivirus (causing measles rubella). More details in the publication - Viral infections as a cause of embryo- and fetopathy
Pathogenesis
Prenatal formation of the brain and its cortex from the neuroectoderm of the prechordal region begins in the fifth to sixth week of gestation. And it is during this period – as a result of abnormal proliferation and migration of neuroblastic cells along the neural tube – that a cleft in the brain substance occurs, which subsequently leads to disruption of its development. And the pathogenesis of which lies in cortical dysplasia and destructive changes in the cerebral hemispheres. [ 7 ], [ 8 ]
This genetically determined cortical malformation may affect one or both hemispheres of the brain and consists of the formation of a cleft that connects the internal soft membrane (pia mater) of the cerebral hemisphere with one or both lateral ventricles of the brain (ventriculi laterales), which are lined with ependyma, consisting of neuroglial cells similar to the epithelial cells of the mucous membranes. The lining of the cleft is gray matter, but it is heterotopic: due to a delay in the migration of neurons into the cerebral cortex, they are arranged incorrectly - in the form of a continuous layer (columns) of gray matter, which is adjacent directly to the junction of the pia mater and ependyma. [ 9 ], [ 10 ]
Most clefts are located in the posterior frontal or parietal lobes, but can occur in the occipital and temporal lobes.
Schizencephaly can be of two types - open and closed. In open type, a cerebrospinal fluid-filled cleft runs through the hemispheres from the ependyma in the center to the pia mater without a connecting band of gray matter.
Closed schizencephaly, on the other hand, is characterized by gray-matter-covered bands (called "lips" by imaging experts) that touch and fuse together. In the former, the cerebrospinal fluid between the ventricular cavity and the subarachnoid space circulates freely; in the latter, the cleft prevents its circulation.
Often, there is an absence of part of the hemispheres with their replacement by cerebrospinal fluid. Microcephaly, absence of the transparent septum (septum pellucidum) in the brain and hypoplasia of the optic nerve (septo-optic dysplasia), as well as aplasia of the corpus callosum are common.
Symptoms schizencephaly
The clinical symptoms of schizencephaly vary depending on which part of the brain is affected, whether the anomaly is open, closed, unilateral or bilateral, and their severity is determined by the degree of clefting and the presence of other cerebral anomalies.
The closed type of defect may be asymptomatic or may be detected in adults with average intelligence when seeking help for epileptic seizures and minor neurological problems (limited movement).
The first signs of open schizencephaly, which has a more severe course when bilateral, are manifested by seizures, muscle weakness and motor disorders. Severe cognitive impairment (with lack of speech) is observed. Patients may have paresis and paralysis of varying degrees (upper and lower limbs) with impaired motor functions (up to the inability to walk).
Bilateral schizencephaly of the brain in a newborn leads to delayed development of both physical and mental development. With bilateral clefts, infants experience spastic diplegia and tetraplegia (paralysis of all limbs), with unilateral clefts, spastic hemiplegia (one-sided paralysis).
Complications and consequences
With schizencephaly, consequences and complications include:
- epilepsy, often refractory (resistant to drugs), which manifests itself in children under three years of age;
- muscle hypotonia, partial or complete paralysis;
- accumulation of cerebrospinal fluid in the brain - hydrocephalus with increased intracranial pressure.
Diagnostics schizencephaly
Instrumental diagnostics can detect schizencephaly of the brain, and this is MRI - magnetic resonance imaging (MRI) of the brain, which makes it possible to obtain images in different planes, visualize the size of the defect, determine its exact location and predict the neurological outcome. [ 11 ], [ 12 ]
The presence of a cleft can be determined by ultrasound of the fetus at 20-22 weeks of pregnancy, but this congenital defect is considered a neonatal diagnosis.
Differential diagnosis
Based on tomographic visualization of cerebral structures, differential diagnostics with focal cortical dysplasia and other brain dysgenesis are carried out.
Who to contact?
Treatment schizencephaly
In all cases of the presence of abnormal clefts in the thickness of the cerebral hemispheres, treatment is symptomatic, aimed at stopping seizures, increasing muscle tone and developing motor skills.
Antiepileptic drugs are used for seizures.
Physiotherapy is carried out. For example, in Europe, the dynamic neuromuscular treatment method of Vaclav Vojta (a Czech pediatric neurologist who worked in Germany for over 35 years) is used. This method is based on the principles of reflex locomotion, and, as studies have shown, promotes cortical and subcortical activation of the brain and central nervous system.
Occupational therapy is aimed at developing fine motor skills, work therapy is aimed at developing basic skills, and speech therapy is aimed at developing speech.
If this defect is complicated by hydrocephalus, surgical treatment involves the installation of a ventriculoperitoneal shunt to drain cerebrospinal fluid.
Prevention
Preventive measures include proper obstetric management of pregnancy and timely prenatal diagnosis of congenital diseases, as well as seeking genetic counseling (when planning a pregnancy).
Forecast
For patients with schizencephaly, the prognosis can vary depending on the size of the clefts and the extent of neurological impairment.

