Medical expert of the article
New publications
Dysgenesis of the brain
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Common neurological problems for children are pathologies, the appearance of which is based on improper intrauterine development of the brain. Such disorders are called "brain dysgenesis"; we are talking about multifactorial conditions that often do not have a pronounced clinical picture. In most cases, parents seek help from a doctor with complaints of learning difficulties, seizures, motor absent-mindedness, behavioral deviations in the child. Brain dysgenesis is recognized only during CT or nuclear magnetic resonance imaging. In general, the mechanisms of development of the disorder have not been sufficiently studied.
Epidemiology
Defects in brain development account for about 20% of all developmental defects. According to experts, the incidence of congenital disorders of the central nervous system ranges from 1 to 2 cases per 1,000 newborns. [ 1 ], [ 2 ]
Among congenital anomalies of brain development, one of the first places is occupied by cortical dysgenesis, which becomes the main cause of the emergence of childhood epileptic syndrome. In general, congenital anomalies of the brain are detected in approximately 30% of cases of all dysgenesis diagnosed in childhood.
Cortical dysgenesis is observed in 25-40% of patients with brain developmental defects and is often accompanied by epileptic syndrome or other types of symptomatic epilepsy.
Among congenital anomalies of the brain, cortical dysgenesis is observed quite often, which is due to the wide practical use of neuroimaging diagnostics - in particular, neurosonography, magnetic resonance imaging, computed tomography.
Causes brain dysgenesis
The most obvious causes of brain dysgenesis are considered to be:
- impaired intrauterine development of the nervous system (at the stage of development);
- damage to the nervous system at the stage of early embryogenesis as a result of gene mutations, infectious diseases of the mother during pregnancy, exposure to radiation, traumatic injuries, exposure of the fetus to chemical agents and toxins.
Among the infections that have a damaging effect on the nervous system of the fetus, rubella, toxoplasmosis, viral hepatitis, and cytomegalovirus infection should be especially noted.
Most often, abnormal intrauterine development is caused by the negative impact of unfavorable factors on the mother and baby's body that have a teratogenic effect. Exogenous causes of dysgenesis may include:
- radioactive radiation;
- influence of chemical agents;
- elevated temperature;
- exposure to high frequency currents;
- unsatisfactory environmental conditions, which lead to toxic products entering the woman’s body.
In addition, some medications and hormonal agents that the expectant mother may take without knowing about the pregnancy may also have a teratogenic effect. There is evidence that many medications easily penetrate the placenta and end up in the baby's circulatory system. Not only potent substances, but also common medications in large doses, and even multivitamin complexes can be dangerous. [ 3 ]
Metabolic disorders, viral and other infections, including those with a latent asymptomatic course, can also provoke intrauterine developmental disorders such as dysgenesis. The following are considered especially dangerous:
- hyperthyroidism;
- metabolic disorders;
- diabetes mellitus;
- syphilis;
- cytomegalovirus infection;
- rubella;
- listeriosis;
- toxoplasmosis.
The life of a pregnant woman has an extremely negative impact on the course of pregnancy and the health of the future child. Teratogenic effects are caused by:
- alcohol consumption;
- smoking;
- addiction.
Risk factors
The following are considered predisposing factors for the development of brain dysgenesis:
- hereditary predisposition (related cases of the occurrence of pathology, by autosomal type of inheritance, or linked to the X-chromosome);
- spontaneous mutation;
- chromosomal rearrangement;
- intrauterine infection (mainly of viral origin) or traumatic injuries;
- the influence of intoxications, medications, chemicals during the intrauterine development stage;
- fatal alcohol syndrome caused by maternal alcoholism during pregnancy;
- acute deficiency of nutrients in the fetus;
- severe metabolic disorders in the expectant mother.
Currently, scientists cannot identify any one main cause of brain dysgenesis, so it is necessary to weigh the existing risk factors. [ 4 ]
Pathogenesis
The development of the human brain begins at the intrauterine stage, actively continuing after birth. According to experts, the right cerebral hemisphere is responsible for figurative and creative thinking, motor coordination, balance, spatial visual and kinesthetic receptivity. The left cerebral hemisphere determines mathematical, symbolic, logical, speech, analytical abilities, ensures the receptivity of information by ear, target settings and schematic settings. A single brain is the work of two hemispheres, tightly interconnected with each other by the neurofibrous system (corpus callosum).
The corpus callosum is located between the cerebral hemispheres in the occipital-parietal region. It includes 200 million nerve fibers and ensures the coordinated work of the brain and the transfer of information between the hemispheres. With such a disorder as brain dysgenesis, a person's cognitive function suffers. With improper conduction through the corpus callosum, the dominant hemisphere takes on an increased load, with the other practically inactive. The connection between the two brain "halves" is lost. As a result, spatial orientation suffers, an imbalance occurs, the patient cannot correctly perceive his own body, adequately react emotionally. The function of perception of the leading limbs is impaired. [ 5 ]
Children with brain dysgenesis often do not crawl, and have difficulties with walking, reading, and writing. Information is perceived mainly through hearing and vision. In the absence of treatment and medical rehabilitation, such patients subsequently develop many problems related to general development and learning. [ 6 ]
Symptoms brain dysgenesis
Clinical symptoms manifest differently in all patients, so diagnostics are performed at different times. For example, severe forms of brain dysgenesis are detected in early childhood, while in adults the disorder may be latent and diagnosed by chance.
Children with brain dysgenesis in the neonatal period may have a normal and quite healthy appearance, and development indicators coincide with normal ones up to the age of three months. Starting from 3 months, the first pathological signs may appear in the form of epileptic seizures, infantile spasms, etc.
The clinical picture may be represented by the following signs:
- disturbance of the formation and subsequent development of the corpus callosum;
- cystic dilatation of the cerebral ventricular cavity, anomaly of the cerebral mantle;
- hydrocephalus;
- atrophy of the optic and auditory nerves;
- microencephaly;
- tumor processes (including cysts) in the area of the cerebral hemispheres;
- incomplete formation of convolutions;
- early sexual development;
- malformation of the spinal column (spina bifida, non-fusion of the vertebral arch);
- Aicardi syndrome (early myoclonic encephalopathy);
- lipomas;
- various types of pathologies of the digestive system;
- retarded psychomotor development;
- intellectual and physical retardation;
- coordination disorders;
- defects of other organs, including the musculoskeletal system;
- decreased muscle tone.
In relatively mild cases of dysgenesis, with normal mental and motor development, signs of impaired information exchange between the cerebral hemispheres may be observed. [ 7 ]
First signs
Brain dysgenesis in infants is most often detected after three months of life, although it is possible to diagnose the pathology even at the stage of intrauterine development. The first signs of a malfunction in babies are usually as follows:
- the appearance of convulsions, infantile spasms;
- convulsions;
- weakening of screaming;
- problems with vision, smell and/or touch;
- communication disorders; [ 8 ]
- signs of muscle hypotonia (decreased reflex activity, profuse salivation, inhibition of physical development, weak motor activity, impaired grasping function).
In older people, dysgenesis is characterized by deterioration of auditory and visual memory, impaired motor coordination and thermoregulation (hypothermia).
Infantile spasms are sudden convulsive flexion-extension of the limbs. Muscle hypotonia is characterized by decreased muscle tone (may be combined with loss of muscle strength).
More common are non-syndromic types of dysgenesis, which remain asymptomatic for a long time and are detected almost by chance - for example, during the diagnosis of mental retardation, seizures or large head size. Macrocephaly is partly due to the presence of giant cystic formations located posterior to the third ventricle. Less often, endocrinological disorders may be observed.
Syndromic forms of brain dysgenesis are as follows:
- Aicardi syndrome - occurs predominantly in girls and is characterized by infantile spasms, specific choroidal lacunae, and vertebral-costal defects. The outcome of the pathology is often unfavorable: patients continue to have seizures and experience profound mental retardation.
- A familial syndrome with genital pathology that may manifest as microcephaly and other defects of the central nervous system.
- Andermann syndrome is characterized by damage to the peripheral nervous system in combination with brain dysgenesis (or hypotrophy).
- Syndrome of periodic hyperhidrosis and hypothermia (reverse Shapiro syndrome).
Dysgenesis of the corpus callosum
Dysgenesis is a congenital pathology of the brain, as it begins to develop in the prenatal stage under the influence of various factors. Secondary dysgenesis of the corpus callosum is considered as a secondary destruction of the septum pellucidum: such a defect can be visualized in the coronal projection during neurosonography. Many pathologies are associated with dysgenesis of the septum pellucidum, including stenosis of the aqueduct against the background of secondary hydrocephalus, agenesis of the corpus callosum, Chiari II anomaly, migration defect and septo-optic dysplasia. In septo-optic dysplasia, dysgenesis of the septum pellucidum and hypoplasia of the optic canals, nerve fibers and chiasm are observed. Most patients with such pathology additionally suffer from disorders of the pituitary-hypothalamic system. [ 9 ]
Dysgenesis of the corpus callosum in a child affects the nerve plexuses that connect the two cerebral hemispheres, namely the corpus callosum, which has a flattened shape and is located under the cerebral cortex. The disease can have varying degrees of severity:
- A mild degree of dysgenesis is observed with the preservation of intellectual abilities and motor activity. There are only disturbances in the transmission of impulse signals between the hemispheres.
- The complex degree is accompanied not only by general signs of dysgenesis, but also by other anomalies of brain development. There are pronounced failures in neural connections, seizures, and obvious inhibition of mental development.
Complications and consequences
The outcomes of congenital brain anomalies can be divided into three options:
- Almost complete recovery, with no visible impairments and the patient’s return to normal life activity.
- Residual effects that do not threaten the patient’s life, but to a certain extent limit his everyday and social activities.
- Severe disorders, significant intellectual disabilities.
The severity of the consequences of dysgenesis depends on the volume of pathological changes in the brain, as well as on the cause that provoked this pathology. Timely diagnosis and adequacy of treatment are of great importance. [ 10 ]
In general, many patients with brain dysgenesis experience moderate or severe intellectual disabilities and physical retardation.
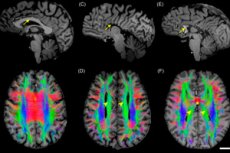
Diagnostics brain dysgenesis
In severe cases of brain dysgenesis, diagnostics can be performed already during a visual examination of a newborn baby. Additional examinations can be prescribed for muscular hypotonia in the neonatal period, for the appearance of convulsions, for mental retardation.
Common diagnostic methods include:
- screening and obstetric ultrasound examination during pregnancy;
- neurosonography through the fontanelle area in the first 12-18 months of the baby’s life;
- electroencephalography with possible video monitoring;
- magnetic resonance imaging. [ 11 ]
To identify disorders associated with dysgenesis and somatic pathologies, ultrasound examination of the kidneys, heart, and abdominal organs is performed. Genetic counseling may also be required. Laboratory tests are performed as part of a general assessment of the body's condition: general blood and urine tests are performed, and less frequently, cerebrospinal fluid is examined.
Instrumental diagnostics in childhood, during the period of open fontanelles, is most often represented by neurosonography – an accessible, mobile, safe and informative procedure. Neurosonography can be used for both congenital and infectious, neuroplastic or traumatic brain lesions. [ 12 ]
Differential diagnosis
When diagnosing brain dysgenesis in the neonatal period, differentiation should be made with the following pathological conditions:
- closure defects, cephalocele, meningocele, myelomeningocele;
- Chiari malformation;
- cerebellar anomalies, ventral induction disorders;
- Dandy-Walker malformation;
- cerebellar dysplasia and hypoplasia; [ 13 ]
- hypoplasia and aplasia of the corpus callosum; [ 14 ]
- holoprosencephaly;
- migration defects, heterotopia, lissencephaly, polymicrogyria, schizencephaly;
- proliferation and neuronal differentiation;
- aqueduct stenosis;
- phakomatoses (Sturge-Weber syndrome);
- vascular malformations.
Who to contact?
Treatment brain dysgenesis
Medicine is unable to completely cure brain dysgenesis. Doctors prescribe treatment to correct the functioning of the central nervous system, to eliminate pathological symptoms, to normalize the intellectual activity of patients. The therapeutic regimen is selected individually for each patient, taking into account the severity of the pathology.
To alleviate the condition, the following medications are prescribed:
- Phenobarbital helps reduce the frequency of infantile spasms. Most often, it is prescribed to children in a dosage of 50 mg per day, and to adults – 200 mg per day.
- Benzodiazepines slow down psychomotor reactions and reduce the frequency of seizures. Diazepam in an initial dose of 5-10 mg corrects behavioral disorders, has a muscle-relaxing effect.
- Corticosteroids eliminate even complex epileptic seizures, but require careful selection of dosage and gradual withdrawal of the drug. Side effects occur mainly against the background of long-term use of such drugs and can be expressed in the appearance of electrolyte disturbances, hyperglycemia, impaired glucose tolerance, osteoporosis, hypertension, etc.
- Neuroleptic drugs are used to prevent mental disorders, but treatment with such drugs should be done with caution, since in some cases neuroleptics can contribute to an increase in the frequency of seizures.
- Nootropics normalize brain functions. The nootropic drug of hopantenic acid Pantogam is especially widespread: its use as part of a neurometabolic corrective treatment regimen helps improve psychosomatic health and optimize the quality of life of children with brain dysgenesis. Neuropeptides optimize neural connections and are widely used in neuropediatrics as effective and safe means of improving mental and motor functions in patients.
In addition to drug treatment, surgical intervention may be prescribed.
Surgical treatment
Surgeon's assistance is required to stimulate the vagus nerve in cases of brain dysgenesis. A special vagus stimulator is used for this purpose, consisting of a pulse generator and battery, as well as a connecting cable with platinum electrodes. The generator is implanted in the left subclavian zone, the electrodes are fixed in the neck area near the left vagus (X cranial nerve).
The implantation is performed under general anesthesia, and the procedure itself lasts about 60-90 minutes. During the operation, two incisions are made in the left armpit and neck area for the correct placement of the pulse generator and electrodes. The functionality of the implant is checked directly during the procedure. After the operation, the patient remains in hospital for several more days.
What does this type of treatment for dysgenesis provide? The occurrence of seizures is blocked, concentration and mood are improved, and the quality of life is increased. These effects are especially evident in patients who have already taken medication therapy, and in particular, antiepileptic drugs.
Surgical intervention is used in cases where other therapeutic methods do not bring the necessary result, and the pathology of brain dysgenesis itself threatens complications in vital organs. [ 15 ]
Prevention
Preventive measures should be used at the stage of preparation for pregnancy and the expected conception. The primary type of dysgenesis prevention includes the following points:
- Optimization of a woman's nutrition throughout the entire reproductive period, regular use of vitamin and mineral components in the form of special pharmacy food supplements or by expanding and enriching the diet.
- Elimination of consumption of unhealthy foods and alcohol.
- Prevention of diabetes mellitus during the preparation for pregnancy and during gestation, preventing the development of obesity.
- Prevention of intoxication and harmful effects (heavy metals, pesticides, certain medications, X-rays). The intake of any medications by a woman should be as justified as possible.
- Prevention of the development of infections, early vaccination against rubella (if the woman was not vaccinated or did not have rubella as a child).
Forecast
If brain dysgenesis is not combined with other developmental disorders, the prognosis can be described as favorable. More than 80% of pediatric patients have virtually no serious consequences of the disease, or acquire borderline neurological disorders.
It is important to understand that the main danger of dysgenesis is that the child is deprived of the opportunity to consolidate acquired skills and abilities, often having to learn a lot anew. The patient needs to constantly return to maintenance courses of treatment, which is especially important against the background of increasing brain load with age. The need for regular therapy remains at least until the age of 14, until the final formation of interhemispheric connections. Moreover, it is not possible to speed up this process, since the consequences of such "acceleration" can be unpredictable.
It is not possible to provide a more accurate prognosis for the disease: brain dysgenesis occurs relatively infrequently and has not yet been studied fully enough.

