Medical expert of the article
New publications
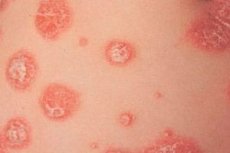
Plaque psoriasis: widespread, chronic, pustular psoriasis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Causes plaque psoriasis
Experts still cannot clearly name the cause of the disease. It is assumed that a hereditary factor is involved, but there are a huge number of cases when plaque psoriasis is diagnosed in people whose heredity is not burdened with the disease. Therefore, scientists have identified a number of theoretical factors that, to one degree or another, can influence the onset of plaque psoriasis in the body.
Risk factors
Risk factors may include the following:
- severe or chronic stress;
- frequent or chronic infectious pathologies, frequent acute respiratory viral infections, acute respiratory infections, tonsillitis;
- poor nutrition with predominant consumption of so-called “unhealthy”, harmful food;
- alcohol abuse;
- diseases of the digestive system, associated primarily with bad habits or poor nutrition;
- work in hazardous industries, chronic intoxication, frequent mechanical damage to the skin;
- chronically weak immunity, vitamin deficiency.
Pathogenesis
To date, experts have proposed two theories of the pathogenesis of plaque psoriasis:
- Immune-dependent theory. Cellular structures responsible for immunity change their protective function: they are directed to the superficial layers of the skin, where a large number of cytokines are released. As a result, the growth of keratocytes is provoked, inflammatory reactions in the skin begin. This theory is justified by the fact that the treatment of psoriatic plaques with immunosuppressant drugs leads to a stable positive effect.
- Theory of functional intracellular disorders. Disrupted intradermal processes lead to a failure of cellular differentiation: uncontrolled cell division begins in the affected cellular structures. As a result, the immune system reacts to this disorder and seeks to suppress it. Evidence is provided to support this version: drugs that have a detrimental effect on the growth and development of keratocytes are successfully used in plaque psoriasis.
It can be noted that both versions listed are absolutely contradictory to each other. That is why the search for the exact cause and the correct solution regarding the pathogenesis of plaque psoriasis is still ongoing.
Symptoms plaque psoriasis
Reddish, flaking and symmetrical localization, spots are most often found on the extensor side of the arms or legs, on the scalp, in the lumbar region, in the gluteal region, on the external genitals. Multiple scales and plaques are regularly formed. Small, separately located spots can merge, spread to the periphery, take various forms.
Depending on the clinical manifestations, there are different types of plaque psoriasis:
- geographic plaque psoriasis - characterized by the fusion of plaques, the outlines of which are similar in appearance to a geographic map;
- plaque psoriasis gyrata - manifested by the peripheral spread of plaques, which, when merging, form the shape of a spiral or garland;
- annular plaque psoriasis - characterized by partial resolution in the central part of the lesions, which gives the plaques the appearance of a ring;
- plaque rupoid psoriasis - it is characterized by the appearance of cone-shaped or saucer-shaped lesions;
- plaque oyster psoriasis - manifests itself in the presence of lesions with a concave central part, which in appearance resembles an oyster shell;
- elephant psoriasis is an atypical type of plaque psoriasis, in which the formation of large plaques with dense thickened scales can be observed (usually on the legs).
The first signs of plaque psoriasis can appear in a person at any age. However, according to statistics, the pathology most often reveals itself in teenagers aged 14-17, or in older people - about 60 years.
Stages
- I – stage of progress: spots appear on certain areas of the skin and gradually grow in size.
- II – stationary stage: the spots merge with each other, forming flaky plaques of a light silver color.
- III – stage of regression: plaques gradually become pale, peeling is minimized. If there was itching or other unpleasant sensations, they remain.
Plaque psoriasis has a chronic course, so the stages are periodically repeated: the period of exacerbation is replaced by a period of remission, the duration of which is different for each patient.
Forms
Plaque psoriasis can occur on its own or in combination with other diseases, such as those of the nervous or digestive systems.
At first, reddish spots appear on certain areas of the skin, on which light scales gradually form. At first, such spots are not very large, but as the disease progresses, they increase in size and merge with each other, forming plaques.
The spots may itch, but this does not always happen: sometimes the patient does not experience any unpleasant sensation in the affected areas.
Widespread plaque psoriasis
If the skin surface covered with psoriatic plaques exceeds 10% of the entire body surface, then we speak of widespread plaque psoriasis - this is a severe form of the disease that requires immediate medical intervention.
The widespread form can affect large areas of the skin, including the scalp. Such patients have an increased risk of developing a microbial or fungal infection. Complications are especially common in patients with lower limbs affected by psoriasis, since fungal diseases most often occur on the legs, abrasions and injuries occur, varicose veins and trophic ulcers are present, which creates a favorable background for plaque infection.
 [ 33 ]
[ 33 ]
What is vulgar plaque psoriasis?
The term "vulgar psoriasis" is a synonym for other names of this disease: plaque, plaque-like, plaque, common, ordinary, scaly psoriasis. All these terms are applied to the same form of psoriasis, so they should be perceived identically.
The name comes from the Latin word "vulgaris" meaning ordinary, common.
Chronic plaque psoriasis
If timely measures are not taken to treat plaque psoriasis, the disease will begin to progress and become chronic. As a rule, in most cases, plaque psoriasis worsens in a wave-like manner, with periodic relief of the patient's condition.
In severe cases, there may be no periods of remission at all: the disease spreads, psoriatic arthritis develops, nails and even internal organs are affected.
 [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ]
[ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ]
Papular plaque psoriasis
Papular plaque psoriasis is a disease in which, along with reddish plaques (flaky spots), papules appear on the skin. What is a papule? It is a cavity-less, superficial, slightly convex formation, prone to transient regression. Otherwise, a papule is also called a nodule.
In psoriasis, papules can grow to the periphery, "melt" in their central part, forming a characteristic ring-like element. In this case, they often talk about annular plaque psoriasis - in fact, these are different names for the same disease.
Complications and consequences
The consequences of plaque psoriasis depend on how severe the disease is. For example, patients with severe forms of the disease have an increased risk of developing lymphoma.
Plaque psoriasis causes patients to experience significant psychological discomfort due to constant worries about their appearance. This manifests itself in low self-esteem, in minimizing social connections, which necessarily affects the patient's ability to work and personal life. Long-term psychological stress leads to the development of depressive states and neuroses, up to suicidal thoughts. It can be said that plaque psoriasis itself does not pose a threat to life, but can significantly affect its quality.
As a result of constant stress, patients often develop secondary complications such as hypertension, cardiovascular pathologies, and diabetes.
Diagnostics plaque psoriasis
Plaque psoriasis is easily determined by external pathological signs. However, if necessary, the doctor can prescribe additional confirmatory diagnostic methods - based on the results of the studies, a more accurate treatment plan for the disease will be drawn up.
The following tests are included in the standard set of studies for psoriasis:
- Blood test (general and biochemical) – attention is paid to the level of leukocytes, hemoglobin, uric acid (rheumatoid factor).
- Stool for the presence of helminths.
- Urine to assess water and electrolyte balance.
Instrumental diagnostics are used to clarify the diagnosis:
- A biopsy is a microscopic examination of affected tissue.
- Radiography is a study to detect damage to joint tissues caused by psoriasis.
- Tests and scrapings to exclude fungal and syphilitic skin lesions.
- Bacterial culture is a study of psoriatic lesions of mucous tissues.
What do need to examine?
How to examine?
Differential diagnosis
Differential diagnosis of plaque psoriasis is carried out mainly with the following diseases:
- with discoid eczema;
- with cutaneous lymphoma;
- with smooth skin dermatophytosis;
- with squamous cell carcinoma;
- with Paget's disease.
In addition, it is advisable to simultaneously exclude such diseases as red hair lichen, simple lichen, epidermal nevus, seborrheic dermatitis, subacute lupus erythematosus, erythrokeratoderma, candidiasis, Hailey-Heli disease, etc.
Who to contact?
Treatment plaque psoriasis
Treatment regimens for plaque psoriasis are developed taking into account a wide range of external and systemic medications. The main focus of treatment is immunomodulation - restoration of damaged immune links, cell functions and ensuring the completeness of ongoing reactions.
When choosing medications for a specific patient, the doctor compares the severity of the disease and the patient's condition as a whole. Since plaque psoriasis is a chronic pathology, it is also important to consider the safety of the selected drugs for long-term use.
Many medications, such as Calcipotriol or Methotrexate, are best suited for long-term use. This cannot be said about topical corticosteroids or cyclosporine, which are prescribed in short courses or as part of complex rotational therapy.
Medicines recommended for plaque psoriasis
Method of administration and dosage |
Side effects |
Special instructions |
|
Calcipotriol |
The ointment is applied to areas with psoriatic plaques twice a day. The course of treatment lasts 1.5-2 months. |
Rarely – skin irritation, hypercalcemia. |
The drug is not used on the skin of the face and is not combined with ointments based on salicylic acid. |
Methotrexate |
Taken orally from 10 to 25 mg per week, with a gradual increase in dosage. |
Anemia, nausea, digestive disorders, dizziness, conjunctivitis, and convulsions may occur. |
Treatment with the drug occurs under constant supervision of a physician, with monitoring of the blood picture and function of the cardiovascular system. |
Efalizumab |
The drug is administered subcutaneously, at an initial dosage of 700 mcg per kg of weight, once a week. The total duration of the course is 3 months. |
Flu-like syndrome, lymphocytosis, allergy, ecchymosis are possible. |
The drug is administered with great care and under the supervision of a physician. |
Lorinden A |
The ointment is applied to the affected skin 2-3 times a day, but not more than 3 weeks in a row. |
Treatment may be accompanied by burning, dry skin, atrophy, hyperpigmentation. |
Lorinden is not applied to the face. The drug cannot be used for a long time, as it can cause addiction and withdrawal syndrome. |
Tacrolimus |
The drug is prescribed in individual dosages, one hour before meals or 2-3 hours after them. |
Treatment may be accompanied by increased blood pressure, tachycardia, dyspepsia, digestive disorders, and renal dysfunction. |
Tacrolimus should not be taken with St. John's wort or other herbal preparations. |
An additional important condition for the onset of remission of plaque psoriasis is considered to be careful adherence to dietary principles of nutrition. First of all, it is necessary to limit the consumption of simple sugars, animal fat and provoking food (chocolate, coffee, hot spices, marinades, alcohol).
Nutrition for plaque psoriasis should focus on fermented milk products, plant products and oils, and cereals.
Regular psychotherapy can also improve the patient's condition, helping to smooth out stressful situations and increase self-esteem. In some situations, the use of antidepressant drugs may be required.
Vitamins
It is very important for patients with plaque psoriasis to receive sufficient amounts of vitamin D 3. This vitamin acts by binding to a specific hormonal receptor - it normalizes the development, differentiation and protective properties of cells, stabilizes calcium and phosphorus metabolism. Vitamin D blocks the processes of keratinocyte proliferation and regulates the differentiation of epidermal cells.
In addition, the vitamin inhibits the production of cytokines by psoriatic cells.
Vitamin D3 analogues recommended for use in plaque psoriasis include Calcipotriol, Maxacalcitol, and Tacalcitol. The listed drugs are often included in complex regimens, along with external hormonal agents. This combination helps enhance the therapeutic effect of corticosteroids and reduces the risk of developing steroid skin atrophy.
Physiotherapy treatment
Physiotherapy is an important component of a comprehensive approach to the treatment of plaque psoriasis. Most often, specialists recommend the following procedures:
- magnetotherapy – exposure to low-frequency constant or pulsed magnetic fields;
- PUVA therapy is a physiotherapeutic method using a photoactive substance, simultaneously with exposure of the skin to long-wave ultraviolet rays;
- electrosleep – the effect of weak electric discharges on the brain;
- Magnetic laser treatment is a method used to treat psoriatic joint lesions;
- UFO – a method of ultraviolet irradiation of the skin;
- X-ray therapy – treatment with X-rays;
- Diadynamic therapy is one of the types of impulse therapy using electric current with a frequency of 50-100 Hz.
Folk remedies
Traditional medicine has a huge number of different recipes that are supposed to rid a person of plaque psoriasis, a chronic, persistent disease. It is difficult to say how effective these remedies are: if a recipe helps some patients, it may not have any effect on others. Most likely, this is because no one yet knows the true cause of the disease – and there may be many of these causes, and they are different for each patient.
However, for plaque psoriasis, the most common folk methods are:
- Every day, you need to treat the affected skin with cabbage brine. There is no need to wash off the brine: it is constantly applied to the same place. After 6-8 days, the plaques will begin to peel off, revealing clean healthy skin.
- You can prepare an antipsoriatic ointment: take 150 g of birch tar, 150 g of medical alcohol, 3 raw egg yolks, 1 tsp of camphor oil, mix everything. Use to lubricate the affected skin. After treatment, do not wash in the bath or take a shower for 24 hours. Use the product 3 times a week until the skin condition improves.
- Prepare a mixture of 1 part aloe juice, 1 part real honey, 3 parts eucalyptus juice. Keep the mixture in a dark place for three days and use to treat skin areas 2-3 times a day.
- An external remedy is prepared from 200 ml of vinegar, 200 g of quality butter, 1 raw egg. The mass is mixed and kept for 7-8 days in a dark, cool place. The finished product is applied to the affected areas several times a day. This ointment has drying and cleansing properties.
Herbal treatment
- Prepare a mixture of equal parts of dry celandine powder, sorrel rhizome, and succession grass. The dry powder of the collection is poured with birch tar and kept for 4 weeks. Apply to the affected areas daily at night. The effect of the remedy will be enhanced if it is alternated with Vishnevsky ointment.
- Prepare a herbal mixture: 1 teaspoon of succession, the same amount of celandine, horsetail, calamus roots, milkweed grass, elderberry flowers. Pour a liter of boiling water over the dried herbs, leave for 2 hours, filter. Take 75 ml orally before main meals. Duration of treatment is up to 1 month.
- A tincture is prepared from the flowers of the Crimean Sophora: 2 teaspoons of flowers are poured into 100 g of vodka and left in the dark for 4 weeks. Take 1 teaspoon before each meal. Duration of therapy is 2 months.
In addition, it is recommended to take medicinal baths and foot baths, to which infusions of thyme, sage, walnut leaves, and celandine are added. Take such baths for 15-20 minutes. After such treatment, the plaques gradually become pale and decrease in size until plaque psoriasis disappears completely.
Homeopathy
By turning to homeopathic treatment, a sick person seeks to stabilize the protective function of his body and direct it to fight the disease - plaque psoriasis.
Before you start selecting a drug, you need to make sure that there is a certificate of conformity and quality, and also be sure to consult with a doctor.
The most popular homeopathic remedies for plaque psoriasis are:
- Sulfur - used in patients with hypersensitive skin;
- Sepia – used to treat patients with skin prone to hyperpigmentation;
- Silicea – suitable for sensitive, irritation-prone skin;
- Arsenicum album - especially recommended for widespread plaque psoriasis affecting the scalp;
- Arsenicum iodatum is recommended for the treatment of patients with large plaques and dense scales.
Homeopathic remedies are prescribed according to individual schemes, depending on the stage of the disease, on the general condition of the patient. The selection of drugs and dosage is carried out by a specially trained homeopathic doctor.
Surgical treatment
Surgery is not the main method of treating plaque psoriasis. Surgical intervention may be relevant in the development of psoriatic arthritis - in this case, it is necessary to remove the affected joint tissue to restore joint function, or to insert implants.
Prevention
The main purpose of prevention for plaque psoriasis is to reduce the frequency of exacerbations and reduce the severity of disease symptoms.
Patients with plaque psoriasis should listen to the following advice from specialists:
- If you take a shower or bath, use only a soft washcloth and towel to avoid damaging the damaged skin.
- After water procedures, be sure to apply any suitable moisturizer to the skin - this will protect the skin from damaging and drying external influences.
- In everyday life, it is necessary to beware of various skin injuries. To ensure protection during cleaning, it is recommended to wear protective gloves, and it is better to choose clothes made of natural fabric (to prevent the development of allergies).
- The room you spend most of your time in should be sufficiently ventilated and humidified. An air conditioner is not recommended, as it dries out the air excessively.
- You need to take care of your health and avoid contact with people who have colds and viral diseases.
- If possible, take care of your nervous system – do not react to stressful situations, do not allow mental and physical exhaustion.
- Avoid overcooling and overheating.
- Forget about the existence of alcohol and cigarettes.
- Pay attention to your diet - is it correct? If in doubt, read the rules of nutrition for psoriasis.
Forecast
For life, plaque psoriasis has a favorable prognosis. A sick person can live a normal life if periodically undergo treatment to prevent exacerbations of the disease. But it should be noted that plaque psoriasis tends to persist and spread throughout the body, so the disease should not be ignored under any circumstances. Therapeutic courses must be repeated regularly, depending on the periods of exacerbation of the pathology. Sanatorium and resort treatment in specialized institutions is also welcomed.
Sometimes – although only in 15-16% of cases – a so-called spontaneous healing is observed, when plaque psoriasis disappears in the same way it appeared. The reasons for this phenomenon remain a mystery.
 [ 58 ]
[ 58 ]

