Medical expert of the article
New publications
Pituitary microadenoma: causes, symptoms, what is dangerous, prognosis
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Benign neoplasms that arise in the endocrine glands are called adenomas, and a microadenoma of the pituitary gland is a small tumor of its anterior lobe, which produces a number of important hormones.
Epidemiology
The incidence of pituitary tumors is estimated to be 10-23%, and pituitary adenomas, which can have various shapes and sizes, are the most common (16%).[ 1 ]
Up to 20-25% of people may have small pituitary tumors, microadenomas, without even knowing it, and such tumors are discovered by chance during brain imaging in about half of the cases.
Prolactin-secreting microadenomas account for 45-75% of such tumors; ACTH-producing formations account for no more than 14% of cases, and the frequency of STH-producing microadenomas does not exceed 2%.
Microadenoma of the pituitary gland in children and adolescents is detected in 10.7-28% of cases, and at least half of them are hormonally inactive. [ 2 ]
Causes pituitary microadenomas
Experts do not know the exact reasons for the appearance of microadenoma in the pituitary gland, an endocrine gland in the brain whose cells produce:
- corticotropin or ACTH – adrenocorticotropic hormone, which causes the secretion of steroid hormones by the adrenal cortex;
- growth hormone STH – somatotropic hormone;
- gonadotropins FSH – follicle-stimulating hormone and LH – luteinizing hormone, which determine the production of female sex hormones in the ovaries and male sex hormones in the testes;
- lactogenic hormone prolactin (PRL);
- thyrotropin or thyroid-stimulating hormone (TSH), which stimulates the synthesis of hormones by the thyroid gland.
It is believed that the development of these neoplasms may be caused by traumatic brain injury; insufficient blood supply to the pituitary gland; cerebral infections or exposure to toxins (causing edema and intracranial hypertension).
Risk factors
It is known that pituitary adenomas and microadenomas occur more often in the presence of a family history of MEN 1 syndrome - multiple endocrine adenomatosis type 1, which is hereditary. Thus, there are genetically determined risk factors associated with certain changes in DNA. [ 3 ]
Multiple endocrine neoplasia type 4 (MEN4): MEN 4 has a mutation in the cyclin-dependent kinase inhibitor 1 B (CDKN1B) gene, which is characterized by pituitary tumors, hyperparathyroidism, neuroendocrine tumors of the testes and cervix.[ 4 ]
Carney complex (CNC): In Carney complex, there is a germline mutation in the tumor suppressor gene PRKAR1A leading to primary pigmented nodular adrenocortical disease (PPNAD), testicular tumors, thyroid nodules, patchy hyperpigmentation of the skin, and acromegaly.[ 5 ]
The clinical form of familial isolated pituitary adenomas (FIPA) is characterized by genetic defects in the aryl hydrocarbon receptor interacting protein (AIP) gene, in approximately 15% of all related and 50% of homogeneous somatotropin families.[ 6 ]
Familial isolated pituitary adenomas (FIPA): A mutation in the aryl hydrocarbon receptor interacting protein (AIP) is detected in adolescence or early adulthood in approximately 15% of all FIPA cases. These tumors are typically aggressive and most often secrete growth hormone, causing acromegaly.[ 7 ]
The possibility of this type of tumor arising as a result of functional disorders on the part of other endocrine glands and cerebral structures, in particular, changes in the vascular system of the hypothalamus, which within the neuroendocrine hypothalamic-pituitary system regulates the functioning of the pituitary gland and its anterior lobe, the adenohypophysis, with its releasing hormones, is not excluded.
Pathogenesis
According to its histology, pituitary adenoma is a benign tumor; depending on the size, these neoplasms are divided into microadenomas (up to 10 mm in size at the widest point), macroadenomas (10-40 mm) and giant adenomas (40 mm or more).
While studying the pathogenesis of tumor formation in the pituitary gland, it has not yet been possible to determine the mechanisms of hyperplastic transformation of cells of its anterior lobe into a tumor.
Experts believe that one of the most convincing versions is a connection with the deregulation of the metabolism of the neurotransmitter and hormone dopamine (which is the main inhibitor of prolactin secretion) and/or a disruption of the functions of transmembrane dopamine receptors of pituitary cells that secrete PRL (lactotrophs).
Most pituitary microadenomas are sporadic, but some occur as part of genetically determined neuroendocrine syndromes such as MEN 1, McCune-Albright syndrome, Werner syndrome, and Carney syndrome (or Carney complex). The latter is associated with an increased risk of developing benign tumors in hormonal (endocrine) glands, including the pituitary, adrenal, thyroid, ovaries, and testicles.
Symptoms pituitary microadenomas
A pituitary microadenoma may not show any symptoms for a very long time. Symptoms vary depending on the location and usually arise as a result of endocrine dysfunction. This is the most common finding in cases of hormonal imbalance associated with excessive production of one or more hormones. In most cases, by location, this is a microadenoma of the anterior pituitary gland.
There are different types of pituitary microadenoma based on their hormonal activity. Thus, the most common type is considered to be a non-functioning adenoma – a hormonally inactive pituitary microadenoma, which – until it reaches a certain size – does not give any symptoms. But a growing hormonally inactive pituitary microadenoma can compress nearby brain structures or cranial nerves, so a pituitary microadenoma and headaches in the frontal and temporal regions can be combined, [ 8 ] and vision problems are also possible. [ 9 ] However, as researchers claim, non-functioning (hormonally inactive) pituitary tumors in 96.5% of cases are macroadenomas. [ 10 ]
Hormonally active microadenoma of the pituitary gland (its anterior lobe) with increased secretion of the hormone prolactin may also occur - prolactinoma of the pituitary gland. Increased production of PRL by lactotropic cells of the adenohypophysis is defined as hyperprolactinemia in pituitary microadenoma.
How does such a pituitary microadenoma manifest itself in women? Pathologically high levels of this hormone inhibit the production of estrogens, and the first signs are manifested by menstrual cycle disorders - with the absence of menstruation (amenorrhea) and / or their ovulatory phase. As a result, persistent galactorrhea-amenorrhea syndrome develops and the ability to conceive and become pregnant is lost.
Prolactin-secreting pituitary microadenoma in men can lead to hyperprolactinemic hypogonadism with decreased libido, erectile dysfunction, enlarged breasts (gynecomastia), and decreased facial and body hair.
Active microadema secreting corticotropin (ACTH) leads to an excess of steroid hormones (glucocorticoids) produced by the adrenal cortex, which can cause Itsenko-Cushing's disease of pituitary etiology.
In children, such a microadenoma can manifest itself with symptoms of hypercorticism (Cushing's syndrome), including headaches, general weakness, excess deposition of adipose tissue on the trunk, decreased bone mineral density and muscle strength, strip-like atrophy of the skin (in the form of purple striae), etc.
With an active somatotropin-producing microadenoma, the level of STH in the body increases. In childhood, its excessive anabolic effect stimulates the growth of almost all bones in the body and can lead to gigantism; in adults, acromegaly can develop with increased growth of the facial bones (causing distortion of appearance) and cartilage in the joints of the extremities (which leads to a violation of their proportions and thickening of the fingers), with joint pain, excessive sweating and sebum secretion, and impaired glucose tolerance.
Very rarely (in 1-1.5% of cases) there is a microadenoma of the pituitary gland that produces thyrotropin, and since this hormone has a stimulating effect on the thyroid gland, patients have clinical signs of pituitary hyperthyroidism in the form of sinus tachycardia and atrial fibrillation of the heart, increased blood pressure, decreased body weight (with increased appetite), as well as increased nervous excitability and irritability.
The so-called intrasellar microadenoma of the pituitary gland, synonym - endosellar microadenoma of the pituitary gland, like the entire pituitary gland, is localized within the sella turcica - inside the anatomical saddle-shaped depression in the sphenoid bone of the base of the skull. At the same time, the pituitary gland is located at the bottom of this depression - in the pituitary fossa (intrasellar region). And the whole difference in terms is that "inside" in Latin is intra, and in Greek - endom.
But a pituitary microadenoma with suprasellar growth means that the neoplasm grows upward from the bottom of the pituitary fossa.
Cystic microadenoma of the pituitary gland has a closed sac-like structure and is an asymptomatic formation.
Microadenoma of the pituitary gland with hemorrhage may be the result of apoplexy or hemorrhagic infarction associated with enlargement of the gland and damage to the sinusoidal capillaries of the parenchyma of its anterior lobe, neurohemal synapses and/or portal vessels.
Microadenoma of the pituitary gland and pregnancy
As already noted, women with prolactin-producing pituitary microadenoma are usually infertile due to estrogen deficiency and suppression of pulsatile secretion of GnRH (gonadotropin-releasing hormone). In order to become pregnant, prolactin levels must be normalized, otherwise conception does not occur, or the pregnancy is terminated at the very beginning.
- Is it possible to give birth with a pituitary microadenoma?
In women with clinically functioning microadenomas who are treated with dopamine agonists (Cabergoline or Dostinex), prolactin levels may normalize and menstrual cycles and fertility may be restored.
Is breastfeeding possible with pituitary microadenoma?
In the postpartum period, breastfeeding is allowed if there are no symptoms of the tumor, but it is necessary to monitor its size (using magnetic resonance imaging of the brain). And if the tumor grows, breastfeeding is stopped.
- Microadenoma of the pituitary gland and IVF
Treatment of hyperprolactinemia is required for IVF, and the procedure can be initiated if normal prolactin levels have been stable for 12 months and there are no abnormalities in serum levels of other pituitary hormones.
Complications and consequences
What is dangerous about pituitary microadenoma? Although this tumor is benign, its presence can cause complications and have consequences, in particular:
- lead to dysfunction of the hypothalamic-pituitary-adrenal system with the development of Itsenko-Cushing's disease;
- disrupt hormonal regulation of the menstrual cycle in women and lead to erectile dysfunction in men;
- cause growth retardation and pituitary dwarfism (hypopituitarism) in children;
- provoke the development of osteoporosis.
When a growing tumor compresses the optic nerve fibers in the area of their crossing (which in 80% of people is located directly above the pituitary gland), there is a disturbance in eye mobility (ophthalmoplegia) and a gradual deterioration in peripheral vision. Although microadenomas are usually too small to exert such pressure.
Can a pituitary microadenoma resolve? It cannot resolve, but over time, a hormonally inactive tumor in children can significantly decrease. But in about 10% of patients, microadenomas can increase in size.
Diagnostics pituitary microadenomas
To diagnose a pituitary microadenoma, a complete patient history and laboratory tests are required: blood tests for hormone levels (produced by the pituitary gland), including a radioimmunoassay of blood serum for prolactin levels.
If prolactin is normal with a pituitary microadenoma, then this tumor is hormonally inactive. But if there are symptoms of prolactinoma, then such a false negative result may be the result of either a laboratory test error, or the patient has developed a macroadenoma that compresses the pituitary stalk.
In addition, additional tests may be required, for example, for the level of thyroid hormones (T3 and T4), immunoglobulins, interleukin-6 in the blood serum.
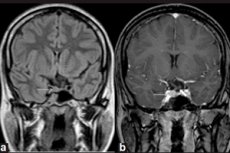
Microadenoma can only be detected by instrumental diagnostics using magnetic resonance imaging (MRI) of the brain. And MRI for microadenoma is considered the standard of visualization, with the sensitivity of MRI with contrast enhancement being 90%.
MRI signs of pituitary microadenoma include: volume of the gland on the side of the microadenoma; an increase in the size of the sella turcica; thinning and changes in the contour of its fundus (lower wall); lateral deviation of the pituitary infundibulum; isointensity of the rounded area compared to gray matter on T1- and T2-weighted images; slight hyperintensity on T2-weighted images. [ 11 ]
Differential diagnosis
Differential diagnostics are carried out with craniopharyngioma, granular cell tumor (choristoma) of the pituitary gland, Rathke's pouch cyst, dermoid formation, inflammation of the pituitary gland - autoimmune or lymphocytic hypophysitis, pheochromocytoma, thyroid diseases, etc.
In women with an anovulatory cycle, pituitary microadenoma and polycystic ovary syndrome are differentiated, since 75-90% of cases of lack of ovulation are a consequence of polycystic ovary syndrome.
Who to contact?
Treatment pituitary microadenomas
In case of adenomas and microadenomas of the pituitary gland, treatment can be medical and surgical. At the same time, if the tumors are asymptomatic, it is recommended to monitor them, that is, periodically conduct MRI, so as not to miss the beginning of their enlargement.
The prescription of a particular drug is determined by the type of tumor the patient has.
Pharmacotherapy of tumors secreting PRL is carried out with drugs from the group of stimulators of dopamine D2 receptors of the hypothalamus (selective dopamine agonists), and most often used are Bromocriptine (Parlodel, Bromergol), Norprolac and the ergot derivative Cabergoline or Dostinex for pituitary microadenoma with increased secretion of prolactin.
Side effects of Dostinex (Cabergoline) may include allergic reactions; headaches and dizziness; nausea, vomiting and abdominal pain; constipation; a feeling of weakness or fatigue; sleep disturbances. And among the side effects of Bromocriptine (in addition to allergic reactions) are chest pain; increased heart rate and breathing with a feeling of shortness of breath; coughing up blood; deterioration in coordination of movements, etc.
The drugs Octreotide (Sandostatin), Lanreotide (Somatuline), Pegvisomant, used for micro- and macroadenomas that secrete growth hormone, are inhibitors of STH and antagonists of its receptors.
And for ACTH-secreting neoplasms of the adenohypophysis with Itsenko-Cushing syndrome, Metyrapone (Metopirone) or Mitotane (Lysodren) are used.
Surgical treatment should be considered for functioning (hormonally active) microadenomas. In cases where conservative treatment is ineffective and the tumor has a slight suprasellar expansion within the sella turcica, pituitary adenomectomy may be prescribed - an operation to remove the pituitary microadenoma. Currently, transnasal or transsphenoidal microdissection is performed, that is, removal of the pituitary microadenoma through the nose.
Possible complications and consequences of pituitary microadenoma removal include postoperative bleeding and cerebrospinal fluid leakage (often requiring reoperation), as well as inflammation of the meninges, visual impairment, hematoma formation, transient diabetes insipidus, and recurrence of the microadenoma.
Homeopathy for pituitary microadenoma with hyperprolactinemia uses drugs whose action can help to partially relieve symptoms. For example, for irregular menstruation and amenorrhea, a remedy made from cuttlefish ink Sepia and a remedy made from the meadow pasqueflower plant Pulsatilla are prescribed, and for galactorrhea, a remedy based on the root of European cyclamen is prescribed.
Obviously, one should not hope that folk treatment for pituitary microadenoma can be more effective. And not only because with this diagnosis herbalists are guided only by the complaints of patients (without knowing their true etiology), but also because of the unreliability of many "folk remedies". You don't have to go far for examples.
Some Internet sources recommend using a mixture of primrose, ginger root and sesame seeds to reduce prolactin levels. But primrose helps with prolonged dry coughs, thinning phlegm, and ginger root, like sesame seeds, exhibits lactogenic properties.
You can also find advice to take a tincture of bugbane. But, in reality, this remedy is used internally for flatulence, and externally for rheumatic joint pain. In all likelihood, bugbane was confused with the roots of black cohosh (other names for it are black cohosh and black cohosh), which are used for hot flashes during menopause.
Nutrition for pituitary microadenoma should be balanced - with reduced sugar and salt consumption. This is not a special diet, but simply less caloric.
Alcohol is excluded in case of pituitary microadenoma.
Which doctor should I see for a pituitary microadenoma? Endocrinologists, gynecologists, and neurosurgeons deal with the problems that arise with this type of tumor.
Prevention
Because the environmental or lifestyle causes of pituitary tumors are unknown, there is simply no way to prevent the development of pituitary microadenomas.
Forecast
Most pituitary tumors are curable. If a hormonally active pituitary microadenoma is diagnosed in time, the chances of recovery are high and the prognosis is favorable.
Disability and pituitary microadenoma: disability may be associated with tumor growth and damage to the optic nerve, as well as other consequences of this pathology, the severity of which is individual. And recognition of a patient as disabled depends on existing health problems and the level of functional disorders, which must meet legislatively approved criteria.
Microadenoma of the pituitary gland and the army: patients with this tumor (even if it is successfully removed) should not overheat, stay in the sun for a long time and overexert themselves physically. So, they are not suitable for military service.
How long do people live with pituitary microadenoma? This tumor is not cancer, so there are no life expectancy limits. Although with active STH-producing microadenoma, patients may develop hypertension and an increase in heart size, and this can significantly reduce their life expectancy. An increased risk of death in patients over 45 years of age is noted with Itsenko-Cushing's disease and acromegaly.

