Medical expert of the article
New publications
pituitary gland
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The pituitary gland (hypophysis, s.glandula pituitaria) is located in the hypophyseal fossa of the sella turcica of the sphenoid bone and is separated from the cranial cavity by a process of the dura mater of the brain, forming the diaphragm of the sella. Through the opening in this diaphragm, the pituitary gland is connected to the infundibulum of the hypothalamus of the diencephalon. The transverse size of the pituitary gland is 10-17 mm, the anteroposterior is 5-15 mm, the vertical is 5-10 mm. The mass of the pituitary gland in men is approximately 0.5 g, in women - 0.6 g. The pituitary gland is covered externally by a capsule.
In accordance with the development of the pituitary gland from two different rudiments, two lobes are distinguished in the organ - the anterior and the posterior. The adenohypophysis, or anterior lobe (adenohypophysis, s.lobus anterior), is larger, making up 70-80% of the total mass of the pituitary gland. It is denser than the posterior lobe. In the anterior lobe, a distal part (pars distalis) is distinguished, which occupies the anterior part of the pituitary fossa, an intermediate part (pars intermedia), located on the border with the posterior lobe, and a tuberous part (pars tuberalis), going upward and connecting with the infundibulum of the hypothalamus. Due to the abundance of blood vessels, the anterior lobe has a pale yellow color with a reddish tint. The parenchyma of the anterior pituitary gland is represented by several types of glandular cells, between the strands of which sinusoidal blood capillaries are located. Half (50%) of the adenohypophysis cells are chromophilic adenocytes, which have fine-grained granules in their cytoplasm that stain well with chromium salts. These are acidophilic adenocytes (40% of all adenohypophysis cells) and basophilic adenocytes (10%). Basophilic adenocytes include gonadotropic, corticotropic, and thyrotropic endocrinocytes. Chromophobic adenocytes are small, they have a large nucleus and a small amount of cytoplasm. These cells are considered to be precursors of chromophilic adenocytes. The other 50% of the adenohypophysis cells are chromophobic adenocytes.
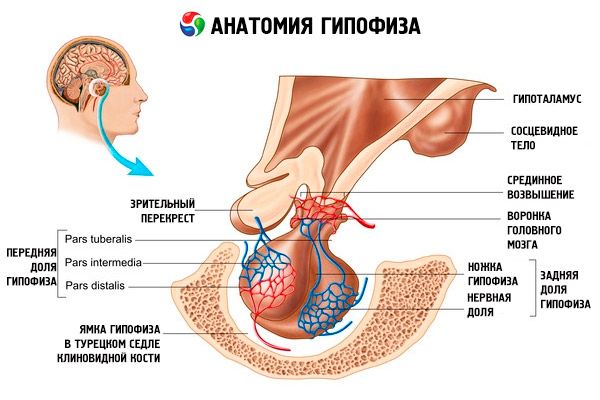
The neurohypophysis, or posterior lobe (neurohypophysis, s.lobus posterior), consists of the neural lobe (lobus nervosus), which is located in the posterior part of the pituitary fossa, and the funnel (infundibulum), located behind the tuberous part of the adenohypophysis. The posterior lobe of the pituitary gland is formed by neuroglial cells (pituitary cells), nerve fibers that go from the neurosecretory nuclei of the hypothalamus to the neurohypophysis, and neurosecretory corpuscles.
The pituitary gland, via nerve fibers (pathways) and blood vessels, is functionally connected to the hypothalamus of the diencephalon, which regulates the activity of the pituitary gland. The pituitary gland and hypothalamus, together with their neuroendocrine, vascular and nerve connections, are usually considered the hypothalamic-pituitary system.
Hormones of the anterior and posterior pituitary glands affect many functions of the body, primarily through other endocrine glands. In the anterior pituitary gland, acidophilic adenocytes (alpha cells) produce somatotropic hormone (growth hormone), which participates in the regulation of growth and development processes in young organisms. Corticotropic endocrinocytes secrete adrenocorticotropic hormone (ACTH), which stimulates the secretion of steroid hormones by the adrenal glands. Thyrotropic endocrinocytes secrete thyrotropic hormone (TSH), which affects the development of the thyroid gland and activates the production of its hormones. Gonadotropic hormones: follicle-stimulating (FSH), luteinizing (LH) and prolactin - affect the sexual maturation of the body, regulate and stimulate the development of follicles in the ovary, ovulation, growth of the mammary glands and milk production in women, the process of spermatogenesis in men. These hormones are produced by basophilic adenocytes (beta cells). Lipotropic factors of the pituitary gland are also secreted here, which affect the mobilization and utilization of fats in the body. In the intermediate part of the anterior lobe, melanocyte-stimulating hormone is formed, which controls the formation of pigments - melanins - in the body.
Neurosecretory cells of the supraoptic and paraventricular nuclei in the hypothalamus produce vasopressin and oxytocin. These hormones are transported to the cells of the posterior pituitary gland along axons that make up the hypothalamic-pituitary tract. From the posterior pituitary gland, these substances enter the blood. The hormone vasopressin has a vasoconstrictive and antidiuretic effect, for which it is also called the antidiuretic hormone (ADH). Oxytocin has a stimulating effect on the contractility of the uterine muscles, increases milk secretion by the lactating mammary gland, inhibits the development and function of the corpus luteum, and affects changes in the tone of the smooth (non-striated) muscles of the gastrointestinal tract.
Development of the pituitary gland
The anterior lobe of the pituitary gland develops from the epithelium of the dorsal wall of the oral bay in the form of a ring-shaped outgrowth (Rathke's pouch). This ectodermal protrusion grows toward the bottom of the future third ventricle. Towards it, from the lower surface of the second cerebral vesicle (the future bottom of the third ventricle), a process grows, from which the gray tubercle of the infundibulum and the posterior lobe of the pituitary gland develop.
Vessels and nerves of the pituitary gland
From the internal carotid arteries and vessels of the arterial circle of the cerebrum, the superior and inferior pituitary arteries are directed to the pituitary gland. The superior pituitary arteries go to the gray nucleus and the infundibulum of the hypothalamus, anastomose with each other here and form capillaries penetrating the brain tissue - the primary hemocapillary network. From the long and short loops of this network, the portal veins are formed, which are directed to the anterior lobe of the pituitary gland. In the parenchyma of the anterior lobe of the pituitary gland, these veins break up into wide sinusoidal capillaries, forming the secondary hemocapillary network. The posterior lobe of the pituitary gland is supplied with blood mainly by the inferior pituitary artery. There are long arterial anastomoses between the superior and inferior pituitary arteries. The outflow of venous blood from the secondary hemocapillary network is carried out through a system of veins that flow into the cavernous and intercavernous sinuses of the dura mater of the brain.
Sympathetic fibers that enter the organ along with arteries participate in the innervation of the pituitary gland. Postganglionic sympathetic nerve fibers depart from the plexus of the internal carotid artery. In addition, numerous endings of the processes of neurosecretory cells located in the nuclei of the hypothalamus are found in the posterior lobe of the pituitary gland.
Age-related features of the pituitary gland
The average weight of the pituitary gland in newborns reaches 0.12 g. The organ's weight doubles by the age of 10 and triples by the age of 15. By the age of 20, the weight of the pituitary gland reaches its maximum (530-560 mg) and remains almost unchanged in subsequent age periods. After 60 years, a slight decrease in the weight of this endocrine gland is observed.
 [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
[ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
Pituitary hormones
The unity of nervous and hormonal regulation in the body is ensured by the close anatomical and functional connection of the pituitary gland and hypothalamus. This complex determines the state and functioning of the entire endocrine system.
The main endocrine gland that produces a number of peptide hormones that directly regulate the function of the peripheral glands is the pituitary gland. It is a reddish-gray bean-shaped formation covered with a fibrous capsule weighing 0.5-0.6 g. It varies slightly depending on the sex and age of a person. The generally accepted division of the pituitary gland into two lobes that differ in development, structure and function remains: the anterior distal - adenohypophysis and the posterior - neurohypophysis. The first makes up about 70% of the total mass of the gland and is conventionally divided into the distal, infundibular and intermediate parts, the second - into the posterior part, or lobe, and the pituitary stalk. The gland is located in the pituitary fossa of the sella turcica of the sphenoid bone and is connected to the brain through the stalk. The upper part of the anterior lobe is covered by the optic chiasm and optic tracts. The blood supply to the pituitary gland is very abundant and is carried out by branches of the internal carotid artery (the superior and inferior pituitary arteries), as well as by branches of the arterial circle of the cerebrum. The superior pituitary arteries participate in the blood supply of the adenohypophysis, and the inferior ones - the neurohypophysis, contacting with the neurosecretory endings of the axons of the large-cell nuclei of the hypothalamus. The former enter the median eminence of the hypothalamus, where they disperse into a capillary network (the primary capillary plexus). These capillaries (with which the terminals of the axons of the small neurosecretory cells of the mediobasal hypothalamus contact) collect into portal veins descending along the pituitary stalk into the parenchyma of the adenohypophysis, where they again divide into a network of sinusoidal capillaries (the secondary capillary plexus). Thus, the blood, having previously passed through the median eminence of the hypothalamus, where it is enriched with hypothalamic adenohypophysotropic hormones (releasing hormones), enters the adenohypophysis.
The outflow of blood saturated with adenohypophyseal hormones from numerous capillaries of the secondary plexus is carried out through the system of veins, which in turn flow into the venous sinuses of the dura mater and then into the general bloodstream. Thus, the portal system of the pituitary gland with a descending direction of blood flow from the hypothalamus is a morphofunctional component of the complex mechanism of neurohumoral control of the tropic functions of the adenohypophysis.
The pituitary gland is innervated by sympathetic fibers that follow the pituitary arteries. They originate from postganglionic fibers that pass through the internal carotid plexus, connected to the superior cervical ganglia. There is no direct innervation of the adenohypophysis from the hypothalamus. The posterior lobe receives nerve fibers from the neurosecretory nuclei of the hypothalamus.
The adenohypophysis is a very complex formation in its histological architecture. It has two types of glandular cells - chromophobic and chromophilic. The latter are in turn divided into acidophilic and basophilic (a detailed histological description of the pituitary gland is given in the corresponding section of the manual). However, it should be noted that the hormones produced by the glandular cells that make up the parenchyma of the adenohypophysis, due to the diversity of the latter, are to some extent different in their chemical nature, and the fine structure of the secreting cells must correspond to the biosynthesis features of each of them. But sometimes transitional forms of glandular cells that are capable of producing several hormones can be observed in the adenohypophysis. There is evidence that the type of glandular cells of the adenohypophysis is not always determined genetically.
Under the diaphragm of the sella turcica is the funnel-shaped part of the anterior lobe. It embraces the stalk of the pituitary gland, contacting the gray tubercle. This part of the adenohypophysis is characterized by the presence of epithelial cells and abundant blood supply. It is also hormonally active.
The intermediate (middle) part of the pituitary gland consists of several layers of large secretory-active basophilic cells.
The pituitary gland performs various functions through its hormones. Its anterior lobe produces adrenocorticotropic (ACTH), thyroid-stimulating (TSH), follicle-stimulating (FSH), luteinizing (LH), lipotropic hormones, as well as growth hormone - somatotropic (STO) and prolactin. In the intermediate lobe, melanocyte-stimulating hormone (MSH) is synthesized, and in the posterior lobe, vasopressin and oxytocin accumulate.
ACTH
Pituitary hormones are a group of protein and peptide hormones and glycoproteins. Of the hormones of the anterior pituitary gland, ACTH has been studied best. It is produced by basophilic cells. Its main physiological function is to stimulate the biosynthesis and secretion of steroid hormones by the adrenal cortex. ACTH also exhibits melanocyte-stimulating and lipotropic activity. In 1953, it was isolated in pure form. Later, its chemical structure was established, consisting of 39 amino acid residues in humans and a number of mammals. ACTH has no species specificity. At present, chemical synthesis of both the hormone itself and various fragments of its molecule, more active than natural hormones, has been carried out. The structure of the hormone has two sections of the peptide chain, one of which ensures the detection and binding of ACTH to the receptor, and the other provides a biological effect. It apparently binds to the ACTH receptor through the interaction of electrical charges of the hormone and the receptor. The role of the biological effector of ACTH is performed by the fragment of the 4-10 molecule (Met-Glu-His-Phen-Arg-Tri-Tri).
The melanocyte-stimulating activity of ACTH is due to the presence in the molecule of the N-terminal region, consisting of 13 amino acid residues and repeating the structure of alpha-melanocyte-stimulating hormone. This region also contains a heptapeptide present in other pituitary hormones and possessing some adrenocorticotropic, melanocyte-stimulating and lipotropic activities.
The key moment in the action of ACTH is considered to be the activation of the enzyme protein kinase in the cytoplasm with the participation of cAMP. Phosphorylated protein kinase activates the enzyme esterase, which converts cholesterol esters into a free substance in fat droplets. The protein synthesized in the cytoplasm as a result of phosphorylation of ribosomes stimulates the binding of free cholesterol to cytochrome P-450 and its transfer from lipid droplets to mitochondria, where all the enzymes that ensure the conversion of cholesterol into corticosteroids are present.
 [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
[ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
Thyroid-stimulating hormone
TSH - thyrotropin - the main regulator of the development and functioning of the thyroid gland, the processes of synthesis and secretion of thyroid hormones. This complex protein - glycoprotein - consists of alpha and beta subunits. The structure of the first subunit coincides with the alpha subunit of luteinizing hormone. Moreover, it largely coincides in different animal species. The sequence of amino acid residues in the beta subunit of human TSH has been deciphered and consists of 119 amino acid residues. It can be noted that the beta subunits of human and cattle TSH are similar in many ways. The biological properties and nature of biological activity of glycoprotein hormones are determined by the beta subunit. It also ensures the interaction of the hormone with receptors in various target organs. However, the beta subunit in most animals exhibits specific activity only after it combines with the alpha subunit, which acts as a kind of activator of the hormone. The latter with equal probability induces luteinizing, follicle-stimulating and thyrotropic activities determined by the properties of the beta subunit. The similarity found allows us to conclude that these hormones arose in the process of evolution from one common predecessor, the beta subunit also determines the immunological properties of the hormones. There is an assumption that the alpha subunit protects the beta subunit from the action of proteolytic enzymes, and also facilitates its transportation from the pituitary gland to the peripheral target organs.

Gonadotropic hormones
Gonadotropins are present in the body in the form of LH and FSH. The functional purpose of these hormones is generally reduced to ensuring reproductive processes in individuals of both sexes. They, like TSH, are complex proteins - glycoproteins. FSH induces the maturation of follicles in the ovaries of females and stimulates spermatogenesis in males. LH causes follicle rupture in females with the formation of the corpus luteum and stimulates the secretion of estrogens and progesterone. In males, the same hormone accelerates the development of interstitial tissue and the secretion of androgens. The effects of gonadotropins are dependent on each other and occur synchronously.
The dynamics of gonadotropin secretion in women changes during the menstrual cycle and has been studied in sufficient detail. In the preovulatory (follicular) phase of the cycle, the LH content is at a fairly low level, while FSH is increased. As the follicle matures, estradiol secretion increases, which promotes increased production of gonadotropins by the pituitary gland and the occurrence of both LH and FSH cycles, i.e. sex steroids stimulate the secretion of gonadotropins.
Currently, the structure of LH has been determined. Like TSH, it consists of 2 subunits: a and b. The structure of the alpha subunit of LH in different animal species largely coincides, it corresponds to the structure of the alpha subunit of TSH.
The structure of the beta subunit of LH differs significantly from the structure of the beta subunit of TSH, although it has four identical sections of the peptide chain consisting of 4-5 amino acid residues. In TSH, they are localized in positions 27-31, 51-54, 65-68 and 78-83. Since the beta subunit of LH and TSH determines the specific biological activity of the hormones, it can be assumed that homologous sections in the structure of LH and TSH should ensure the connection of beta subunits with the alpha subunit, and sections that differ in structure should be responsible for the specificity of the biological activity of the hormones.
Native LH is very stable to the action of proteolytic enzymes, but the beta subunit is quickly cleaved by chymotrypsin, and the a subunit is difficult to hydrolyze by the enzyme, i.e. it plays a protective role, preventing chymotrypsin from accessing the peptide bonds.
As for the chemical structure of FSH, researchers have not yet obtained definitive results. Like LH, FSH consists of two subunits, but the beta subunit of FSH differs from the beta subunit of LH.
Prolactin
Another hormone, prolactin (lactogenic hormone), plays an active role in reproduction processes. The main physiological properties of prolactin in mammals are manifested in the form of stimulation of development of mammary glands and lactation, growth of sebaceous glands and internal organs. It promotes the manifestation of the effect of steroids on secondary sexual characteristics in males, stimulates the secretory activity of the corpus luteum in mice and rats, and participates in the regulation of fat metabolism. Much attention has been paid to prolactin in recent years as a regulator of maternal behavior; such polyfunctionality is explained by its evolutionary development. It is one of the ancient pituitary hormones and is found even in amphibians. At present, the structure of prolactin in some mammalian species has been completely deciphered. However, until recently, scientists expressed doubts about the existence of such a hormone in humans. Many believed that its function was performed by the growth hormone. Now convincing evidence has been obtained of the presence of prolactin in humans and its structure has been partially deciphered. Prolactin receptors actively bind growth hormone and placental lactogen, indicating a single mechanism of action of the three hormones.
Somatotropin
The growth hormone, somatotropin, has an even broader spectrum of action than prolactin. Like prolactin, it is produced by acidophilic cells of the adenohypophysis. STH stimulates skeletal growth, activates protein biosynthesis, has a fat-mobilizing effect, and promotes an increase in body size. In addition, it coordinates metabolic processes.
The participation of the hormone in the latter is confirmed by the fact of a sharp increase in its secretion by the pituitary gland, for example, when the blood sugar level decreases.
The chemical structure of this human hormone is now fully established - 191 amino acid residues. Its primary structure is similar to that of chorionic somatomammotropin or placental lactogen. These data indicate a significant evolutionary proximity of the two hormones, although they exhibit differences in biological activity.
It is necessary to emphasize the high species specificity of the hormone in question - for example, STH of animal origin is inactive in humans. This is explained by both the reaction between the receptors of STH of humans and animals, and the structure of the hormone itself. Currently, studies are underway to identify active centers in the complex structure of STH that exhibit biological activity. Individual fragments of the molecule that exhibit other properties are studied. For example, after hydrolysis of human STH by pepsin, a peptide consisting of 14 amino acid residues and corresponding to the molecule section 31-44 was isolated. It did not have a growth effect, but significantly exceeded the native hormone in lipotropic activity. Human growth hormone, unlike the similar hormone of animals, has significant lactogenic activity.
The adenohypophysis synthesizes many peptide and protein substances that have a fat-mobilizing effect, and the pituitary tropic hormones - ACTH, STH, TSH and others - have a lipotropic effect. In recent years, beta- and y-lipotropic hormones (LPG) have been particularly emphasized. The biological properties of beta-LPG have been studied in most detail; in addition to lipotropic activity, it also has a melanocyte-stimulating, corticotropin-stimulating and hypocalcemic effect, and also produces an insulin-like effect.
At present, the primary structure of sheep LPG (90 amino acid residues), lipotropic hormones of pigs and cattle has been deciphered. This hormone has species specificity, although the structure of the central region of beta-LPG is the same in different species. It determines the biological properties of the hormone. One of the fragments of this region is found in the structure of alpha-MSH, beta-MSH, ACTH and beta-LPG. It is suggested that these hormones arose from the same precursor in the process of evolution. γ-LPG has a weaker lipotropic activity than beta-LPG.
Melanocyte-stimulating hormone
This hormone, synthesized in the intermediate lobe of the pituitary gland, stimulates the biosynthesis of the skin pigment melanin in its biological function, promotes an increase in the size and number of pigment cells melanocytes in the skin of amphibians. These qualities of MSH are used in biological testing of the hormone. There are two types of the hormone: alpha- and beta-MSH. It has been shown that alpha-MSH does not have species specificity and has the same chemical structure in all mammals. Its molecule is a peptide chain consisting of 13 amino acid residues. Beta-MSH, on the contrary, has species specificity, and its structure differs in different animals. In most mammals, the beta-MSH molecule consists of 18 amino acid residues, and only in humans is it extended from the amino acid end by four amino acid residues. It should be noted that alpha-MSH has some adrenocorticotropic activity, and its effect on the behavior of animals and humans has now been proven.
Oxytocin and vasopressin
Vasopressin and oxytocin, which are synthesized in the hypothalamus, accumulate in the posterior lobe of the pituitary gland: vasopressin in the neurons of the supraoptic nucleus, and oxytocin in the paraventriculatory nucleus. Then they are transferred to the pituitary gland. It should be emphasized that the precursor of the vasopressin hormone is synthesized in the hypothalamus first. At the same time, the protein neurophysin types 1 and 2 are produced there. The first binds oxytocin, and the second binds vasopressin. These complexes migrate in the form of neurosecretory granules in the cytoplasm along the axon and reach the posterior lobe of the pituitary gland, where the nerve fibers end in the vascular wall and the contents of the granules enter the blood. Vasopressin and oxytocin are the first pituitary hormones with a completely established amino acid sequence. In their chemical structure, they are nonapeptides with one disulfide bridge.
The hormones under consideration produce various biological effects: they stimulate the transport of water and salts through membranes, have a vasopressor effect, enhance contractions of the smooth muscles of the uterus during childbirth, and increase secretion of the mammary glands. It should be noted that vasopressin has a higher antidiuretic activity than oxytocin, while the latter has a stronger effect on the uterus and mammary gland. The main regulator of vasopressin secretion is water consumption; in the renal tubules, it binds to receptors in the cytoplasmic membranes with subsequent activation of the enzyme adenylate cyclase in them. Different parts of the molecule are responsible for binding the hormone to the receptor and for the biological effect.
The pituitary gland, connected through the hypothalamus with the entire nervous system, unites the endocrine system into a functional whole, participating in ensuring the constancy of the internal environment of the body (homeostasis). Within the endocrine system, homeostatic regulation is carried out based on the principle of feedback between the anterior lobe of the pituitary gland and the "target" glands (thyroid gland, adrenal cortex, gonads). Excess of the hormone produced by the "target" gland inhibits, and its deficiency stimulates the secretion and release of the corresponding tropic hormone. The hypothalamus is included in the feedback system. It is in it that the receptor zones sensitive to the hormones of the "target" glands are located. By specifically binding to hormones circulating in the blood and changing the response depending on the concentration of hormones, hypothalamic receptors transmit their effect to the corresponding hypothalamic centers, which coordinate the work of the adenohypophysis, releasing hypothalamic adenohypophysiotropic hormones. Thus, the hypothalamus should be considered as a neuroendocrine brain.

