Medical expert of the article
New publications
Exudative pericarditis
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Among the many possible complications of cardiovascular pathologies, a special place belongs to pericarditis - these are diseases that are not always accompanied by pronounced clinical symptoms, but often pose a threat to both the health and life of the patient. One of these dangerous variants of pathology is exudative pericarditis, in which an excess volume of fluid accumulates in the space between the layers of the outer inflamed cardiac membrane. In a healthy person, this volume is within 25 ml, and with pericarditis it increases tenfold or more. Rapid filling of the space leads to compression of the muscle layer, which is a life-threatening condition and requires emergency medical care. With a slow accumulation of fluid, stagnation is observed, circulatory failure increases. [ 1 ]
Epidemiology
In most patients, exudative pericarditis becomes a complication or one of the signs of another cardiovascular or visceral disorder; only in rare cases does it become an independent disease.
Regardless of its origin, exudative pericarditis belongs to the category of dangerous (often life-threatening) conditions. According to pathological statistics, the disease (experienced or current at the time of the patient's death) is detected in approximately 5% of cases. But the frequency of lifetime diagnostics is significantly lower, which is primarily due to certain diagnostic difficulties.
Female and male patients suffer from pericardial effusion at approximately equal rates.
Pericardial effusion can occur in all ages and population groups. The predominant etiology of the effusion depends on demographic characteristics such as age, geography, and comorbidities. Data on the prevalence and incidence of pericardial effusions are scarce. Viral pericarditis causing effusion is the most common cause in developed countries. In developing regions, pericardial effusion due to Mycobacterium tuberculosis is quite common. Bacterial and parasitic etiologies are less common. Among noninflammatory pericardial effusions, multiple malignancies can cause pericardial effusion. In patients with pericardial effusion, malignancies account for 12% to 23% of pericarditis cases. In patients with HIV, pericardial effusion has been reported in 5% to 43%, depending on inclusion criteria, with 13% having moderate to severe effusion. According to a study conducted in pediatric patients, the main causes of pericarditis were postcardiac surgery (54%), neoplasia (13%), renal (13%), idiopathic or viral pericarditis (5%), and rheumatologic (5%). and pericardial effusion in children.[ 2 ], [ 3 ], [ 4 ]
Causes exudative pericarditis
Exudative pericarditis is more often a consequence than a primary cause: the disease develops in response to existing polyserositis or other pathology accompanied by damage to the pericardium.
According to the etiological factor, infectious exudative pericarditis (specific and non-specific), non-infectious pericarditis (immunogenic, mechanical, intoxication) and idiopathic (with an unknown cause) pericarditis are distinguished. [ 5 ]
The non-specific form of infectious pericarditis is most often provoked by:
- cocci (strepto or staphylococcus, pneumococcus);
- viral infection (influenza virus, enterovirus).
- A specific form of pericarditis can be provoked by the pathogen of such diseases:
- tuberculosis, brucellosis;
- typhoid fever, tularemia;
- fungal infections, helminthiasis, rickettsiosis.
Exudative pericarditis of tuberculous origin develops when mycobacteria enter the pericardium with the lymph flow from the lymph nodes of the mediastinum, trachea and bronchi. The purulent form of the disease can occur as a complication of coronary surgical interventions, as well as with infectious and inflammatory lesions of the endocardium, immunosuppressive treatment, and with spontaneous opening of a pulmonary abscess. [ 6 ]
The non-infectious type of exudative pericarditis is often idiopathic, meaning that the cause of its occurrence cannot be determined. If the cause is determined, then most often it is:
- about malignant lesions of the pericardium (in particular, about mesothelioma);
- about invasions and metastases in lung carcinoma, breast cancer, lymphoma or leukemia;
- about connective tissue pathologies (rheumatism, systemic lupus erythematosus, etc.);
- about allergic reactions (serum sickness);
- about uremia accompanying chronic renal failure;
- about radiation damage to the mediastinal organs;
- about the early stage of myocardial infarction;
- about decreased thyroid function;
- about cholesterol metabolism disorders. [ 7 ]
Risk factors
A small volume of effusion is always present in the pericardial space. This is necessary to ensure sliding during cardiac contractions. An increase in this volume occurs as a result of the inflammatory reaction and increased vascular permeability. As the pathology develops, the serous layers are unable to absorb excess effusion, which enters at an accelerated rate, so its level quickly increases. [ 8 ]
Exudative pericarditis is predominantly secondary in nature, as it is a complication of other diseases and pathological conditions:
- severe infectious diseases;
- autoimmune disorders;
- allergic processes;
- traumatic injuries (blunt trauma, penetrating wounds);
- effects of radiation;
- blood diseases;
- tumor processes;
- myocardial infarction;
- metabolic disorders;
- cardiological operations;
- insufficient renal function.
Pathogenesis
Impaired blood supply to the pericardium in exudative pericarditis may manifest itself to varying degrees, depending on the amount of accumulated fluid, the rate of accumulation, and the quality of adaptation to the load of the outer pericardial leaflet. If the fluid enters gradually, the leaflet has time to adapt and stretch: the pressure inside the pericardium changes insignificantly, and intracardiac circulation is compensated for a long time. Patients with exudative pericarditis may accumulate different amounts of exudate - from 400-500 ml to 1.5-2 liters. The greater the volume of such fluid, the more the organs and nerve endings located near the heart are compressed. [ 9 ]
If the exudate accumulates in large volumes over a short period of time, the pericardium does not have time to adapt, the pressure in the pericardial space increases significantly, and a complication develops – cardiac tamponade. [ 10 ]
The fluid in exudative pericarditis may subsequently be reorganized, being replaced by granulations. These processes cause pericardial thickening: the space is either preserved or obliterated. [ 11 ]
Symptoms exudative pericarditis
The first and main symptom of exudative pericarditis is chest pain, which intensifies during deep inhalation. The pain makes itself known abruptly, sharply, sometimes like a heart attack. The patient's suffering is somewhat alleviated in a sitting position.
Features of pain in exudative pericarditis:
- begins abruptly, lasts for a long time (sometimes does not go away within several days);
- located behind the sternum or slightly to the left;
- radiates to the left arm, collarbone, shoulder, neck area, and left half of the lower jaw;
- does not disappear after taking nitroglycerin;
- increases with inhalation, coughing or swallowing;
- gets worse in a horizontal position, especially when trying to lie on your back;
- decreases when sitting and leaning forward.
Fever is less common.
It is important to understand that exudative pericarditis often occurs simultaneously with other cardiac pathologies, in particular, with myocardial infarction. Therefore, the clinical picture can expand taking into account another disease or acute condition, which significantly complicates diagnosis.
First signs
As exudate accumulates in the pericardium, signs of compression of the myocardium and respiratory system are observed. The most common symptoms are:
- chest pain;
- persistent hiccups;
- an unexplained feeling of uneasiness;
- persistent cough;
- hoarse voice;
- feeling of lack of air;
- difficulty breathing when lying down;
- periodic depression of consciousness.
Chest pain sometimes resembles angina, heart attack or pneumonia:
- increases with physical activity, inhalation, swallowing;
- disappears when leaning forward in a sitting position;
- starts abruptly and lasts a long time;
- may have different intensity;
- may radiate to the left upper limb, shoulder, and neck area.
Position of the patient with exudative pericarditis
A patient with exudative pericarditis usually sits slightly forward: this position helps relieve pain. Other external signs also attract attention:
- skin is pale, fingers are bluish;
- the chest swells, the veins in the neck swell (they do not collapse when inhaling);
- the heartbeat is frequent, irregular, the heartbeat is not detectable or weak;
- heart sounds are weakened on auscultation;
- ascites increases, the liver is enlarged.
Forms
Today, the following classification of pericarditis is generally accepted:
- According to the etiological characteristics:
- bacterial pericarditis;
- infectious and parasitic pericarditis;
- unspecified pericarditis.
- According to pathogenetic and morphological characteristics:
- chronic adhesive;
- chronic constrictive;
- non-inflammatory pericarditis ( hydropericardium, chylopericardium);
- hemopericardium.
- By the nature of the flow:
- acute exudative pericarditis;
- chronic exudative pericarditis.
Acute pericarditis lasts less than six weeks, and chronic - more than six weeks. The acute form develops against the background of an infectious process, or becomes a complication of sepsis, tuberculosis, rheumatism, etc. The inflammatory reaction affects the outer and inner pericardial leaflets. The initial stages of the pathology most often occur without exudative phenomena, like dry pericarditis, but later exudative pericarditis develops.
If the acute form is not treated in a timely manner, it becomes chronic, in which the pericardial leaflets thicken and stick together: an exudative-adhesive process is formed.
Exudative-adhesive pericarditis is also called adhesive, adhesive. This division is considered conditional. This name refers to such an outcome of pericarditis, in which residual phenomena are observed in the form of an adhesive process between the pericardial leaflets, or between the pericardium and adjacent organs. Sometimes calcium crystals accumulate in the hardened pericardium, and calcification begins.
Complications and consequences
Pericardial effusion may be represented by transudate (hydropericarditis), exudate, purulent fluid (pyopericarditis) and blood (hemopericarditis). Large amounts of exudate are characteristic of tumor processes, tuberculosis, uremic or cholesterol forms of pericarditis, helminthiasis and myxedema. Gradually increasing effusion most often does not manifest itself with any symptoms, but with rapid accumulation of exudate, cardiac tamponade may occur.
Cardiac tamponade is a stage of decompensation in cardiac compression, when fluid accumulates in the pericardial space with an increase in pressure in it. Surgical tamponade is accompanied by a rapid increase in pressure, and in the case of an inflammatory reaction, this occurs over several days or weeks.
Local compression may cause dyspnea, difficulty swallowing, hoarseness, hiccups or nausea. Heart sounds are "distant". When the base of the lungs is compressed, dullness is noted under the left shoulder blade. With the onset of tamponade, intrathoracic discomfort, dyspnea, stress tachypnea with transition to orthopnea appear, coughing occurs, the patient may periodically lose consciousness.
In turn, cardiac tamponade can be complicated by renal failure, “shock” liver, mesenteric ischemia, and plethora of abdominal organs.
If difficulties with diagnosis arise, pericardiocentesis, pericardioscopy, epicardial and pericardial biopsy are performed (PCR, immunochemistry and immunohistochemistry are used).
Diagnostics exudative pericarditis
Exudative pericarditis is diagnosed based on information obtained during physical examination, laboratory and instrumental diagnostics.
A medical examination includes listening to the heart with a stethoscope. In case of exudative pericarditis, there will be some protrusion of the anterior surface of the chest and slight edema in the pericardial zone, weakness or loss of the apical impulse, extended boundaries of relative and absolute cardiac dullness, dullness of the percussion sound. The onset of the complication - cardiac tamponade - is indicated by an increase in central venous pressure, a decrease in arterial pressure, increased heart rate with transient disturbance of the heart rhythm, paradoxical pulse. [ 12 ]
The analyses are carried out in the general diagnostic aspect:
- general blood test (possible leukocytosis, increased ESR, signs of secondary pericarditis);
- general urine analysis (signs of nephrotic syndrome, renal failure).
Additionally diagnosed:
- blood electrolytes;
- total protein and fractions;
- blood urea;
- creatinine level and glomerular filtration rate;
- AST, ALT, bilirubin (total, direct);
- lipid spectrum;
- coagulogram;
- immunogram;
- tumor markers;
- PCR for tuberculosis in blood;
- antinuclear antibodies;
- rheumatoid factor;
- thyroid hormones;
- procalcitonin test.
Instrumental diagnostics includes the following procedures:
- chest x-ray;
- echocardiography, electrocardiography;
- pericardial puncture
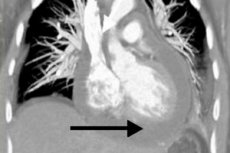
Radiography is prescribed if pericarditis is suspected to assess the level of exudate in the pericardial space. The cardiac shadow may appear enlarged if there is a large amount of fluid in the cavity. With a relatively small volume of effusion, radiography may not indicate pathology. In general, radiographic signs of exudative pericarditis include an enlarged shadow and smoothing of the heart contour, weak pulsation, and a change in the shape of the organ (triangle - if chronic effusion is present for a long time). For clarification, multispiral computed tomography may be prescribed, which usually confirms the presence of pathological fluid and thickening of the pericardial layers. [ 13 ]
Exudative pericarditis on the ECG is manifested by a decrease in the amplitude of all teeth. With additional ultrasound of the heart (echocardiography), it is possible to determine the limitation of cardiac mobility by fluid. [ 14 ], [ 15 ]
Pericardial puncture with further examination of the nature of the exudate is necessary to clarify the cause of the disorder. The removed fluid is subjected to general clinical, bacteriological, cytological analysis, as well as examination for AHAT and LE cells. [ 16 ]
Differential diagnosis
The course of exudative pericarditis should be distinguished from a serious complication of this disease – cardiac tamponade.
Clinical picture of tamponade |
Changes in blood pressure, increased heart rate, paradoxical pulse, shortness of breath against the background of clear lungs. |
Provocative mechanisms |
Medicines (anticoagulants, thrombolytics), cardiac surgery, catheterization, closed chest injuries, tumor processes, connective tissue pathologies, sepsis or renal failure. |
Electrocardiogram |
Normal or non-specific ST-T changes, bradycardia, electromechanical dissociation, electrical alternans. |
Chest X-ray |
Enlargement of the cardiac shadow against the background of clear lung fields. |
Echocardiogram |
Diastolic collapse of the anterior wall of the right ventricle, right atrial or left atrial collapse, increased rigidity of the left ventricular wall in diastole, dilated inferior vena cava, "floating" heart. |
Dopplerography |
Decreased systolic and diastolic venous blood flow during inhalation, increased reverse blood flow during atrial contraction. |
Color Doppler (M-mode) |
Marked respiratory fluctuations in blood flow are observed in the mitral/tricuspid valve. |
Cardiac catheterization |
The diagnosis is confirmed and hemodynamic disturbances are assessed. |
Ventriculography |
Atrial collapse and small hyperactive chambers of the ventricles. |
Coronary angiography |
Compression of the coronary arteries in diastole |
CT |
Subepicardial fat of both ventricles is not visualized, indicating a tubular configuration of the anteriorly displaced atria. |
Myocarditis and pericardial effusion often accompany each other, which is manifested by a general or local dysfunction of the heart muscle. Laboratory features of this phenomenon include an increased level of cardiac troponins I and T, MB fraction of CPK, the level of myoglobin and tumor necrosis factor in the blood. The electrocardiogram shows a concordant rise in the ST segment.
Who to contact?
Treatment exudative pericarditis
Treatment tactics for exudative pericarditis depend on the causes and clinical course of the disease.
Among non-steroidal anti-inflammatory drugs, preference is given to Ibuprofen, which is associated with relatively rare side effects, a positive effect on coronary circulation and the ability to change the dosage within wide limits. Usually, the patient is prescribed 300-800 mg of the drug every 7 hours, for a long time (until the pericardial exudate disappears). [ 17 ]
All patients are prescribed proton pump inhibitors to protect the digestive tract.
Corticosteroids are prescribed when indicated:
- connective tissue pathologies;
- autoreactive pericarditis;
- uremic pericarditis.
Intrapericardial administration of corticosteroids is effective and helps prevent the development of side effects that occur with their systemic use. Against the background of a gradual reduction in the dosage of Prednisolone, Ibuprofen is prescribed in advance.
In case of cardiac tamponade, surgical treatment in the form of pericardiocentesis is indicated.
Essential Medicines for Pericardial Exudative Disease
Nonsteroidal anti-inflammatory drugs (Ibuprofen 200-400 mg, Diclofenac 25-50 mg, etc.) |
Up to 3 times a day as a pathogenetic anti-inflammatory treatment. Side effects: gastrointestinal disorders. |
Systemic glucocorticoid agents (Prednisolone 5 mg, Prednisolone 25 mg/ml, etc.) |
In individual dosages, as a pathogenetic anti-inflammatory treatment for systemic pathologies. |
Glucocorticoid agents for intrapericardial administration (Triamcinolone 1 ml/0.01 g, 1 ml/0.04 g, etc.) |
According to individual protocol. |
Proton pump inhibitors (Omeprazole 20 mg, Pantoprazole 20 mg) |
Once daily to protect the digestive tract. |
Acetylsalicylic acid 75 mg, 100 mg. |
Once a day if exudative pericarditis is combined with infarction. |
Azathioprine 0.05 g |
1-2.5 mg/kg per day in 1-2 doses, if non-steroidal anti-inflammatory drugs and corticosteroids are ineffective. |
Cyclophosphamide 50 mg, 100 mg |
Orally 1-5 mg/kg per day, intravenously 10-15 mg/kg if nonsteroidal anti-inflammatory drugs and corticosteroids are ineffective. |
Aminoglycosides (Tobramycin 1 ml 4%) |
For bacterial exudative pericarditis, 1-2 times a day until clinical signs of eradication appear (1-3 weeks). |
Antiarrhythmic drugs (Amiodarone 150 mg in ampoules, 200 mg in tablets; Verapamil 5 mg in ampoules, 40-80 mg in tablets) |
1-2 times a day to eliminate and prevent arrhythmias. |
Inotropic drugs (Dobutamine 20 ml 250 mg) |
With a sharp decrease in blood pressure and with a peripheral picture of collapse. Side effects: dizziness, headache. |
Physiotherapy treatment
Massage is recommended for chronic exudative pericarditis, during remission. Massage the back, lower limbs (starting from the proximal parts), chest and abdomen. The techniques used are stroking, rubbing, kneading, muscle shaking, excluding blows and squeezing. The duration of a massage session is about 15 minutes. The course will require 10 to 15 sessions. Oxygen therapy is performed after the massage.
In case of heart rhythm disturbances, therapeutic physical training, walking, skiing, and swimming are recommended. Physical therapy classes are conducted with musical accompaniment. Before going to bed, massage the collar zone, back, and lower extremities. Coniferous and oxygen baths, electrophoresis, electrosleep, and diet therapy with additional food vitaminization are recommended.
Upon completion of the treatment course, spa treatment with swimming, walks along the shore, and oxygen cocktails are recommended.
Herbal treatment
A good help in the treatment of exudative pericarditis is folk remedies. Home and affordable recipes will help strengthen the heart, improve blood circulation, restore well-being and cardiac function.
- Infusion of elecampane rhizome and oats. Take 100 g of oat grains, rinse together with the husk, pour 500 ml of drinking water, bring to a boil, remove from heat. Pour in 100 g of crushed elecampane rhizome, bring to a boil again, remove from heat, cover with a lid and leave for 2 hours. Then filter, add 2 tsp of honey. Take according to the scheme: drink 100 ml of the remedy three times a day half an hour before meals, for two weeks.
- Bean broth. Grind bean pods (2 tbsp), pour 1 liter of water, bring to a boil and boil for five minutes. Add 1 tbsp each of hawthorn, motherwort, mint, lily of the valley, boil for another 3 minutes. Cover with a lid, leave for 4 hours, then filter. Store the remedy in the refrigerator. Take 4 tbsp three times a day, half an hour before meals.
- Hawthorn decoction. Take 500 g of hawthorn berries, pour 1 liter of water, bring to a boil and boil for 15 minutes, filter and cool. Add 20 g of honey, stir. Take 2 tbsp. of the remedy before meals daily for a month.
- Viburnum infusion. Take 500 g of berries (dried, fresh, frozen), pour 1 liter of boiling water, leave for 1.5 hours. Drink 200 ml twice a day, with honey. The course of treatment is 1 month, then after 2 months the treatment can be repeated.
- Thistle decoction. Take 1 tbsp. of medicinal raw material, pour 250 ml of water, boil for 15 minutes. Cool, filter, take 100 ml 4 times a day, but the condition improves.
Surgical treatment
Absolute indications for pericardiocentesis in exudative pericarditis are:
- cardiac tamponade;
- large amount of exudate in the pericardial space;
- suspicion of purulent or tuberculous pericarditis, neoplastic pericardial effusion.
Aortic dissection is considered a contraindication to the procedure. Relative contraindications may include uncorrected coagulopathy, anticoagulant therapy, and thrombocytopenia.
Pericardiocentesis under fluoroscopic control and ECG monitoring is performed by access from under the xiphoid process. A long needle with a stylet is advanced toward the left shoulder, maintaining an angle of 30° to the skin surface, which prevents damage to the cardiac, pericardial, and internal thoracic arteries. Periodic attempts are made to aspirate the exudate.
After the catheter is correctly installed, the exudate is removed in parts, no more than 1000 ml at a time, to avoid acute dilation of the right ventricle and the development of sudden decompression syndrome. Continue drainage until the volume of effusion decreases to less than 25 ml per day (every 5 hours). [ 18 ]
All patients are monitored for early detection of decompensation, which may occur after pericardial drainage. Treatment is primarily directed at eliminating the cause of pericardial effusion, rather than eliminating the effusion itself.
Possible complications of pericardiocentesis:
- myocardial perforation;
- hemothorax, pneumothorax;
- air embolism;
- arrhythmia (often vasovagal bradycardia);
- infection;
- damage to the abdominal organs and peritoneum.
The only radical method of treating chronic constriction in exudative pericarditis is pericardiectomy surgery. [ 19 ]
Prevention
After the patient has recovered from exudative pericarditis, the following preventive rules are established:
- Long-term use of non-steroidal anti-inflammatory drugs with discontinuation after elimination of pericardial exudate.
- Timely use of corticosteroids in individually selected dosages.
- Gradually discontinue corticosteroids (over at least three months) and switch to nonsteroidal anti-inflammatory drugs.
- Prevention of gastrointestinal disorders associated with long-term use of non-steroidal anti-inflammatory and corticosteroid drugs.
- Timely pericardiocentesis in case of signs of cardiac tamponade.
- Timely pericardiectomy in symptomatic constrictive pericarditis.
- Providing treatment for the underlying disease (tumor processes, tuberculosis, systemic diseases, etc.).
- Upon completion of treatment of acute exudative pericarditis, the patient is observed for 12 months to detect exacerbations or complications in a timely manner. Blood tests, electrocardiograms, and echocardiograms are performed once every three months.
In general, timely diagnosis of heart disease and treatment of other disease processes that can spread to the heart area contributes to a significant reduction in the risk of developing exudative pericarditis.
The main preventive measures are as follows:
- eradication of bad habits;
- proper nutrition;
- normalization of work and rest regimes;
- active lifestyle;
- avoiding stress and hypothermia;
- timely treatment of any pathologies in the body;
- hardening, strengthening the immune system;
- timely visits to the doctor, including for preventive examinations.
Forecast
The main complication of acute exudative pericarditis is cardiac tamponade. In every third patient, the inflammatory process spreads to the heart muscle, which leads to the appearance of paroxysmal atrial fibrillation or supraventricular tachycardia. Exudative pericarditis often transforms into a chronic or constrictive form.
Correct and timely treatment in the absence of complications guarantees recovery in about three months. The patient gradually returns to his normal rhythm of life. A longer rehabilitation is discussed in the development of a recurrent disease, when periodic repeated accumulation of exudate occurs. [ 20 ]
Postoperative recovery is usually longer: the patient is hospitalized for a week, then discharged to their place of residence, with further cardiac observation. Full restoration of cardiac function occurs after about 6 months. [ 21 ]
With the development of cardiac tamponade, the risk of patient death increases significantly. In general, the prognosis depends on the cause of the pathology and the timeliness of diagnosis and treatment. [ 22 ]
Exudative pericarditis, not complicated by cardiac tamponade, has a relatively favorable prognosis. Full therapy or surgery can restore cardiac function, and the person will be considered practically recovered. Life expectancy may be reduced due to the formation of numerous adhesions even after surgery.

