Medical expert of the article
New publications
Pericardial effusion: norm, method of determination
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
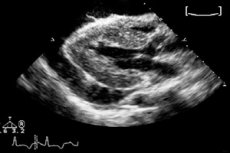
If the volume of fluid in the pericardial space tends to increase pathologically, then we speak of pericardial effusion. During the examination, a darkened echo-negative cavity is detected - mainly through subcostal access. Pericardial effusion can be caused by various factors, and treatment is primarily aimed at eliminating the underlying causes of the pathology.
Epidemiology
Pericardial effusion is found in 6-7% of adult patients. This is a fairly average indicator, which depends on the age category of patients:
- less than 1% of cases with effusion are diagnosed in people 20-30 years old;
- About 15% of cases with effusion are detected in patients over 80 years of age.
After cardiac surgery (correction of the valve system, aortocoronary bypass), pericardial effusion is observed in 77% of operated patients. In 76% of such cases, there is no need for additional treatment.
Causes pericardial effusion
With the improvement of diagnostic methods, pericardial effusion is detected much more often than before. The most common causes are inflammatory processes in the pericardium, tumor formations, and iatrogeny.
In the absence of inflammation in the pericardium, the mechanism of effusion development in many cases remains unclear.
Certain risk factors play a significant role in the appearance of effusion:
- inflammatory processes in the heart tissue;
- cardiac surgery;
- acute myocardial infarction;
- cardiac insufficiency;
- chronic renal failure;
- iatrogenic factor;
- metabolic diseases;
- autoimmune processes;
- chest injuries;
- chylopericardium (accumulation of lymphatic fluid in the pericardial cavity);
- period of bearing a child.
There is also the concept of “idiopathic” effusion – this type of pathology is spoken of when the cause of the disease cannot be determined.
Pathogenesis
Pericardial effusion is the accumulation of varying amounts of fluid surrounding the heart.
The pericardium is a two-layered bag that surrounds the heart. Any healthy person has a small amount of fluid in the pericardial cavity, and this is considered normal.
With various diseases or injuries affecting the pericardium, the fluid in the cavity becomes significantly larger. In this case, the presence of an inflammatory process is not at all necessary. Often, the effusion becomes an accumulation of bloody discharge after surgery or traumatic injury.
If the volume of effusion becomes too large, exceeding the maximum permissible pericardial level, then additional pressure on the heart structures can be created in the cavity. In all cases, this directly affects its functionality.
If the patient does not receive timely medical care, pericardial effusion can lead to a number of negative consequences, including death.
Symptoms pericardial effusion
Pericardial effusion is painless in most cases: pain is typical for effusion caused by acute pericarditis. When listening, muffled heart tones and sometimes pericardial friction noise are noticeable. If the effusion is voluminous, compression of the basal segment of the left lung is possible, which is characterized by weak breathing, microbubble rales, and crepitus. Pulse and blood pressure indicators usually do not go beyond the normal range, unless the condition is close to tamponade.
If pericardial effusion is associated with a heart attack, the patient may have a feverish condition, and pericardial friction rubs are clearly audible. Fluid also accumulates in the pleura and abdominal cavity. Such problems are usually detected starting from the 10th day and up to 2 months after the heart attack.
The first signs are not always noticeable and depend on how quickly the effusion accumulates in the pericardium, how much the heart is compressed, etc. Most often, patients complain of a feeling of heaviness and pain behind the breastbone. If nearby organs are compressed, breathing and swallowing difficulties are observed, coughing and hoarseness appear. Many patients experience swelling of the face and neck, swelling of the venous vessels of the neck (during inhalation), and signs of insufficient cardiac activity increase.
General symptoms may be associated with the development of an exudative inflammatory process:
- the infection is accompanied by chills, signs of intoxication, fever;
- Tuberculosis is characterized by increased sweating, loss of appetite, weight loss, and enlarged liver.
If pericardial effusion is associated with tumor processes, then chest pain, atrial rhythm disturbances, and increasing tamponade are typical.
With a large amount of effusion, patients often prefer to take a sitting position, as the most optimal for their well-being.
 [ 16 ]
[ 16 ]
Forms
Pericardial effusion may be different – first of all, the composition of the fluid in the effusion differs. Thus, it can be serous, fibrous-serous, purulent, bloody (hemorrhagic), putrefactive, cholesterol. Serous effusion is typical for the initial inflammatory stage: such fluid contains protein and water. Fibrin threads are additionally present in fibrous-serous effusion. Bloody effusion occurs with vascular damage: it contains many erythrocytes. Purulent exudate contains leukocytes and particles of dead tissue, and putrefactive exudate contains anaerobic flora.
Clinical features also influence the development of a particular type of pericardial effusion: thus, the pathology may or may not be accompanied by cardiac tamponade.
Complications and consequences
The pericardial cavity can only hold a certain volume of fluid. If the pericardial effusion exceeds the permissible limits, various disorders occur.
The inner lining of the pericardium is formed by a thin layer of cells adjacent to the heart. The outer layer is thicker and more elastic, so when excess effusion accumulates, the pericardial tissues are squeezed inward, putting pressure on the heart.
The stronger the pressure exerted by the fluid, the more difficult it is for the heart to function properly. The chamber structures are insufficiently filled or even partially damaged. Such processes lead to the so-called cardiac tamponade: the organ function is impaired, systemic hemodynamics are upset. With rapid aggravation of the pathology, the heart rhythm is disturbed, a heart attack, cardiogenic shock and even a fatal outcome can develop.
Late consequences include the development of fibrinous pericarditis and loss of impulse conduction between the ventricles and atria.
Diagnostics pericardial effusion
A preliminary diagnosis of pericardial effusion can be made based on the characteristic clinical picture. But most often, doctors think about the possible appearance of effusion only when examining the results of an X-ray, where an increase in the cardiac contour is clearly visible.
The ECG shows a decrease in the voltage of the QRS complex, with the sinus rhythm preserved in the absolute majority of patients. If we are talking about a significant amount of effusion, then on the ECG this is displayed as electrical alternans (an increase and decrease in the amplitude of the P, T waves, or the QRS complex, depending on the moment of cardiac contraction).
Echocardiography is a particularly sensitive method that is often used when pericardial effusion is suspected. The diagnosis is confirmed by visualizing a persistent echo-negative space in the anterior or distal segment of the pericardial bursa. As a rule, effusion is characterized by circulation, but the fluid may also be located regionally. In the latter case, 2D echocardiography is successfully used for diagnosis. If there is no chamber collapse, cardiac tamponade can be excluded.
Additional instrumental diagnostics may include methods such as computed tomography and magnetic resonance imaging. These procedures allow for an accurate assessment of the spatial localization and volume of pericardial effusion. However, their use is only justified if echocardiography is not possible or if there is local effusion.
Laboratory tests are performed to assess the general condition of the body:
- blood clotting parameters and cholesterol levels are assessed;
- the presence of an inflammatory process in the body is determined;
- The functional capacity of the kidneys and liver is monitored.
 [ 31 ]
[ 31 ]
Differential diagnosis
Echocardiographic data in pericardial effusion should be differentiated from left-sided pleurisy and increased proliferation of epicardial fatty tissue.
When effusion accumulates, the atria suffer, causing cardiac and aortic separation: such changes are not typical for pleural effusion. However, in many cases, there are difficulties in differentiating the listed pathologies. In addition, pleural and pericardial effusion are often present together. Right-sided pleural effusion can be seen in the subcostal approach: the pathology has the appearance of an echo-negative space located close to the liver.
The epicardial fat layer on the echocardiogram is distinguished by a granular or fine-grained structure. It is localized around the free edge of the right ventricle. This condition is more often present in elderly patients or in people with problems with excess weight or diabetes.
Treatment pericardial effusion
Treatment measures include the impact on the underlying disease - if it is determined. Then they act directly on the presence of pericardial effusion.
In case of minor effusion – if the patient does not present any complaints, treatment may not be used. It is recommended to undergo a repeat echocardiogram control after three months and six months to assess the dynamics.
Dynamic clinical monitoring is necessary for both moderate and severe effusion, along with conservative treatment.
Treatment with nonsteroidal anti-inflammatory drugs is used. Among such drugs, preference is most often given to Diclofenac sodium, as well as Nimesulide and Movalis. Taking Acetylsalicylic acid helps to eliminate pain, and Colchicine can prevent the recurrence of effusion.
In severe pain and fever, in some cases it is appropriate to use glucocorticoids - for example, Prednisolone, in a short course with absolute withdrawal after 7-14 days. Glucocorticoids are used mainly for autoimmune or postoperative causes of effusion.
To prevent bleeding, anticoagulants are often avoided. They are not prescribed if the patient develops an acute inflammatory process in the pericardium.
Pericardial effusion: medications
- Diclofenac sodium - 75 mg is administered as an intramuscular injection, every day for 10-12 days. You can use the tablet drug - 100 mg / day, for 1-1.5 months.
- Nimesulide - taken orally at 100 mg per day. The duration of treatment is determined by the doctor.
- Movalis – take 7.5 mg daily for two weeks or one month.
- Celebrex – take 200 mg in the morning and evening for two weeks (continuation of use for up to one month is possible).
- Prednisolone - taken 40-60 mg daily, in a minimum short course.
During treatment, it is necessary to take into account the high probability of developing side effects from medications. Thus, non-steroidal anti-inflammatory drugs can provoke drowsiness, headaches, dizziness. Digestive system problems are often observed: nausea, abdominal pain, heartburn, mucosal erosions. The blood picture may change: anemia, thrombocytopenia, leukopenia, agrenulocytosis are detected.
The use of Prednisolone is accompanied by side effects mainly with prolonged treatment. Therefore, it is not recommended to conduct a long therapeutic course, as well as to abruptly discontinue the drug.
Vitamins
The list of nutrients that are very important for heart health is quite extensive. However, if there is a problem such as pericardial effusion, then you should definitely try to include in your diet at least most of the vitamins listed below:
- Ascorbic acid – improves the course of basal metabolism, strengthens the heart muscle and blood vessels, prevents hypercholesterolemia.
- Vitamin A – prevents the development of atherosclerosis, strengthens blood vessels.
- Vitamin E – inhibits fat oxidation, protects heart tissue from damage.
- Vitamin P – helps strengthen arterial walls and prevents bleeding.
- Vitamin F (fatty acids: linolenic, linoleic and arachidonic) – strengthens heart tissue, normalizes blood cholesterol levels, prevents increased thrombus formation.
- Coenzyme Q10 is a vitamin-like component synthesized in the liver that can prevent damage to cardiac tissue, prevent premature aging of the body, and has a beneficial effect on heart rhythm.
- Vitamin B 1 – necessary for the high-quality transmission of nerve impulses and improved myocardial contractility.
- Vitamin B 6 – promotes the removal of excess cholesterol from the body.
Physiotherapy treatment
Physiotherapy and exercise therapy can be used only at the stage of patient rehabilitation, after stabilization of all vital signs. Massage and light gymnastics for all muscle groups are recommended. Exercises with a ball, sticks, and exercise machines are gradually added. As recovery progresses, low-mobility strength exercises and games are allowed. Dosed walking and morning warm-ups are recommended.
The following physiotherapy procedures are often recommended:
- Electrosleep with a frequency of 5-10 Hz, for 20-30 minutes, once every two days. The course of therapy is up to 12 procedures.
- Oxygen therapy – 50-60% with a session duration of 20-30 minutes, 2-3 times a day.
- Foot carbon dioxide, sulphide, radon and iodine-bromine baths, every other day. The course involves 10-12 procedures.
A good recovery effect is expected from aerotherapy and air baths.
Folk remedies
To maintain heart health, it is very important to eat right and not overeat. The diet should include seafood, nuts, citrus fruits, pumpkin, greens, berries, dried fruits. It is also recommended to take flaxseed oil, fish oil, honey, and bee bread.
- Freshly squeezed coltsfoot juice (leaves) is considered a good folk remedy for pericardial effusion. Drink the juice up to six times a day, 1-2 tbsp. According to experts, one two-week course of treatment per year is enough to improve the health of the heart.
- Prepare a mixture of equal amounts of honey and walnuts. To cure pericardial effusion faster, eat 60 g of this mixture daily.
- Mix 100 ml of aloe leaf juice and 200 ml of natural honey, add 200 ml of quality Cahors wine. Take 1 teaspoon of the mixture before each meal.
If pericardial effusion is associated with inflammatory processes in the cardiac tissue, then cornflower tincture can be a good remedy. Take one tablespoon of dried cornflowers (flowers), pour 100 ml of alcohol (or high-quality vodka), insist in a closed container for two weeks. Then filter the tincture and take 20 drops three times a day, half an hour before meals. The duration of treatment varies, depending on the patient's condition.
Herbal treatment
Traditional medicine recipes often include herbal treatment. There are many known ways to get rid of pericardial effusion using medicinal plants. Let's list the most popular of them.
- Prepare a mixture of motherwort, immortelle, hawthorn flowers and medicinal chamomile. Mix all ingredients well, add 1 tbsp of the mixture to 250 ml of boiling water. Infuse under a lid overnight, filter. Take 100 ml three times a day between meals.
- Mix star anise, crushed valerian root, yarrow herb and lemon balm. Pour 250 ml of boiling water over one tablespoon of the mixture, keep it under the lid for about half an hour, filter. Drink the resulting amount of infusion during the day 2-3 times.
- Take large birch "catkins", pour them into a jar (1 l), filling it 2/3, then fill the jar to the top with vodka. Close the container and infuse the medicine for two weeks. Do not filter the tincture. Drink 20 drops of the remedy every day 30 minutes before breakfast, lunch and dinner.
In addition, it is recommended to prepare herbal infusions and teas daily, which include the following herbs: dandelion, aspen buds, knotweed, hop cones, lemon balm leaves, thyme, spring adonis, mint leaves.
Homeopathy
The treatment prescribed by the doctor can be successfully supplemented with homeopathic medicines. They are selected depending on the cause of the pericardial effusion. The main symptoms of the pathology, the constitutional features of the patient, his age and the presence of concomitant diseases are also taken into account. Most often, with pericardial effusion, specialists advise using the following medicines:
- Aconite - helps to eliminate chest pain, normalize heart rhythm and blood pressure. Aconite is especially recommended for the rapid development of cardiac pathology.
- Arnica is often used to restore the heart after a heart attack, as it tones the myocardium, normalizes heart contractions, and promotes the healing of damage to heart tissue.
- Cactus - it is prescribed if pericardial effusion is accompanied by a decrease in pressure, a weak pulse, and a feeling of constriction in the chest.
- Arsenicum album - used for weak constitution with increased fatigue, chronic pericardial effusion, burning pain in the chest.
- Carbo vegetabilis is prescribed for chronic tissue hypoxia, impaired pericardial blood flow, and chronic cardiopulmonary insufficiency.
- Glonoin helps if pericardial effusion is associated with angina pectoris, acute coronary insufficiency, hypertension.
- Krategus - used to eliminate effusion in the elderly, as well as in cardiac edema, myocardial hypertrophy, and stable angina.
Surgical treatment
If a large volume of effusion accumulates, it must be pumped out. This is done by surgical pericardial puncture, with the insertion of a hollow needle into the pericardial space. This procedure is often performed to relieve the heart and remove excess fluid, and is considered a relatively safe treatment method.
The puncture is performed only by a doctor. A special needle with a large lumen is inserted into a certain point just below the border of the heart. If there is a lot of effusion, it is not removed immediately, approximately 150-200 ml at a time. If pus is detected in the effusion, antibiotic solutions can be injected into the pericardial cavity.
In severe cases, a thoracotomy may be required, which is an operation to cut open the chest and resect the pericardium. This procedure is not performed often, and the mortality rate for resection is up to 10%.
Prevention
Basic prevention of pericardial effusion is aimed at preventing pathologies that contribute to its occurrence. Particular attention should be paid to the general strengthening of the body and improving the quality of immune protection.
Doctors advise:
- often walk in green areas, breathe clean air;
- practice moderate physical activity, do morning exercises;
- maintain electrolyte balance, drink enough fluids;
- eat well, supplying the body with all the necessary nutrients;
- Avoid smoking (including passive smoking), do not abuse alcohol.
Even completely healthy people are recommended by doctors to systematically monitor the state of the cardiovascular system: do an ECG or ultrasound of the heart once every 2 years.
Forecast
The prognosis of pericardial effusion depends on many factors. The main probable complication is the development of cardiac tamponade, as well as paroxysmal atrial fibrillation or supraventricular tachycardia. Exudative pericarditis often becomes chronic and constrictive.
The highest mortality rate is found in cardiac tamponade, so it is impossible to clearly predict the outcome of the disease in such a situation. Experts point out that the quality of such a forecast largely depends on the cause of the pathology, on the timeliness of the medical care provided. If you do not allow tamponade to develop, then pericardial effusion can be eliminated without any negative consequences for the patient.

