Medical expert of the article
New publications
Fibrinous pericarditis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Various pathologies of the cardiovascular system can be complicated by such a disorder as fibrinous pericarditis. Such a complication requires immediate examination and treatment, which is necessary to prevent further development of other serious consequences. If such treatment is timely and competent, then most patients experience a favorable outcome of the disease. [ 1 ]
Pericarditis is an inflammatory reaction involving the pericardium. Inflammation is most often caused by primary systemic pathology or structural pericardial changes: damage, infectious and non-infectious lesions.
Fibrinous pericarditis is defined as pericarditis with deposition of fibrinous filaments in the pericardial bursa due to an inflammatory reaction. The condition is characterized by chest pain, which increases with deep breathing or coughing, as well as severe weakness, fever, and auscultatory pericardial friction rub. [ 2 ]
Epidemiology
In clinical practice, fibrous pericarditis is diagnosed relatively rarely – in approximately 0.1% of patients. Postmortem data on the frequency range from 3 to 6%. In men, the pathology develops one and a half times more often than in women aged 20 to 50 years. [ 3 ]
The most common causes of fibrous pericarditis are:
- viruses (up to 50% of cases);
- bacteria (up to 10% of cases);
- acute myocardial infarction (up to 20% of cases);
- metabolic disorders (renal failure, uremia, myxedema – up to 30% of cases), as well as autoimmune pathologies.
It is impossible to establish the cause of fibrous pericarditis in 3-50% of cases. The pathology is rarely diagnosed during the life of patients, and is mainly discovered during autopsy.
Causes fibrinous pericarditis
The most common cause of fibrinous pericarditis is considered to be viral diseases: such a connection is present in almost every second patient. Most often we are talking about enteroviruses, cytomegaloviruses, Coxsackie virus, as well as the causative agent of mumps and HIV.
Fibrinous pericarditis can be caused by:
- acute myocardial infarction;
- traumatic injury (including surgery);
- infectious disease;
- autointoxication (uremia);
- systemic pathologies;
- neoplastic processes.
If we consider oncological causes of fibrinous pericarditis, then most often we are talking about malignant pulmonary tumors and neoplasms of the mammary glands. Leukemia and lymphoma are noted somewhat less often, as well as infiltrative lesion of the pericardium by non-lymphocytic leukemia.
In some situations, the exact origin of the disease cannot be determined: neither tumor structures, nor bacterial microorganisms, nor viruses are determined histologically. Such cases are called idiopathic fibrinous pericarditis.
Risk factors
Etiological risk factors may include:
- autoimmune processes – in particular, systemic lupus erythematosus, rheumatoid arthritis, etc.;
- systemic infectious-allergic inflammation of connective tissue (rheumatism);
- tuberculosis;
- bacterial infectious and inflammatory processes;
- chronic renal failure (terminal stage);
- pneumonia;
- myocardial infarction;
- malignant tumors;
- septic conditions;
- traumatic chest injuries, surgical operations in the heart area.
Risk groups include:
- elderly people (after 55 years);
- patients with elevated blood lipid levels (triglycerides and cholesterol);
- patients suffering from hypertension;
- heavy smokers;
- people with limited or no physical activity;
- persons suffering from obesity and/or diabetes.
Certain dietary habits (abuse of salty, fatty foods, processed foods and fast food), alcohol consumption, and frequent stress are also considered unfavorable factors.
Pathogenesis
In fibrinous pericarditis, no hemodynamic disturbances are observed, since the gradual increase in fluid volume is accompanied by a slow stretching of the outer pericardial leaflet. If the exudation is rapid, then the supporting capacity of the pericardium is activated, which consists in limiting the boundaries of the diastolic expansion of the cardiac chambers. [ 4 ]
Pericardial tissue is characterized by good elasticity, but this property is relatively quickly lost with strong stretching of the pericardium.
Hemodynamic disorders in the form of decreased arterial pressure and venostasis appear when the pressure inside the bursa reaches 50-60 mm Hg. Venous pressure indicators increase and begin to exceed intrapericardial indicators by 20-30 mm Hg. When a critical exudative volume is reached, causing severe compression of the heart, cardiac tamponade develops. The rate of its development depends on the intensity of fluid accumulation. [ 5 ]
The etiology is often infectious, allergic or autoimmune, which is due to the trigger mechanism of the development of pathology. Direct damage to the cardiac membranes by viral and other agents is not excluded.
The pathogenetic pattern of disease development can be described as follows: the pericardium becomes inflamed → vascular permeability increases → liquid fractions of blood and fibrinogen, which are deposited as fibrin, leak into the pericardium → catarrhal pericarditis develops → fibrinous pericarditis develops. [ 6 ]
Pathological anatomy
The appearance of fibrous pericarditis is associated with increased exudation of blood components into the pericardial sac. The fluid accumulation is absorbed by non-inflamed pericardial zones. If vascular permeability is impaired, coarsely dispersed plasma proteins sweat, fibrinogen precipitates, an inflammatory infiltrate is formed, and limited or widespread fibrous pericarditis develops.
Abundant fluid accumulations in the sac indicate an abnormal absorption process and the spread of the inflammatory reaction to the pericardium. If the pericarditis is compressive, the processes of fibrous scarring and adhesion of the leaflets lead to the formation of a dense pericardial membrane. With a prolonged course of the disease, the pericardium calcifies, forming a solid capsule, which is called an "armored" heart. In advanced cases, the muscular layer of the ventricles is damaged, local pathological disorders are noted against the background of myocardial fibrosis. The myocardium becomes thinner, degenerates into fatty tissue and atrophies due to a decrease in the functional load on the ventricles. [ 7 ]
Symptoms fibrinous pericarditis
Symptomatically, fibrous pericarditis may manifest itself with the following signs:
- Heart pain: [ 8 ]
- increasing over several hours;
- of varying intensity (from mild to severe);
- aching, burning, stabbing, scratching, or squeezing, squeezing;
- with localization in the cardiac projection zone, in the epigastrium (usually not radiating to the limb or shoulder, as in ischemic heart disease, but with possible irradiation to the neck and liver area);
- intensifying during swallowing, deep breathing, coughing fits, bending and turning, without any obvious connection with physical activity;
- disappearing as exudate accumulates;
- with relief in a position on the right side with the knees drawn up to the chest;
- disappearing after taking analgesics, non-steroidal anti-inflammatory drugs, but not responding to taking nitroglycerin.
- General weakness, increased sweating, high temperature, headache, as well as signs of general intoxication syndrome.
- Persistent hiccups, nausea (sometimes with vomiting, without subsequent relief), tachypnea, increased heart rate, arrhythmia.
First signs
The initial symptoms of fibrous pericarditis usually manifest as an infectious process, which complicates the diagnosis of the disease. Patients experience general weakness, increased sweating, loss of appetite, and subfebrile temperature.
The symptoms increase and worsen, and a characteristic pericardial pain syndrome is added:
- pain is felt in the epigastrium or behind the breastbone;
- has varying intensity – from slight discomfort to sharp “heart attack” pain;
- According to patients’ descriptions, the pain is burning, tingling, scratching, cutting or pulling;
- increases with coughing movements, position on the left side;
- weakens in the position on the right side, with a forward bend, in the knee-elbow position;
- is not eliminated by taking nitroglycerin.
In addition to pain, there may be painful coughing fits that do not bring relief, as well as nausea and swallowing strain. Breathing movements are shallow, the patient complains of a lack of air. [ 9 ]
Stages
The following stages of pericarditis are distinguished:
- Acute stage – if the disease lasts up to 1-2 months from the onset of the pathology. It is the acute course that is characteristic of exudative and fibrinous pericarditis.
- Subacute stage – if the disease lasts from two to six months from the onset of the pathology. Characteristic for exudative, adhesive and constrictive pericarditis.
- Chronic stage – if the disease lasts more than six months from the onset of the pathology. Characteristic for exudative, adhesive, constrictive pericarditis, as well as for calcification (armored heart).
Forms
Acute fibrinous pericarditis is divided into infectious and infectious-allergic according to the etiologic factor. The subtypes of the disease are:
- tuberculous;
- specific bacterial (syphilitic, gonorrheal, dysenteric, etc.);
- non-specific bacterial (streptococcal, pneumococcal, meningococcal, staphylococcal, etc.);
- viral (adenovirus, influenza, Coxsackie, etc.);
- rickettsial (in patients with Q fever, typhus);
- chlamydial (urogenital infections, ornithosis);
- mycoplasma (pneumonic, acute respiratory disease);
- mycotic (candidal, actinomycosis, histoplasmosis, etc.);
- caused by protozoa (amoebic, malarial);
- allergic;
- rheumatic;
- malignant;
- traumatic, etc.
Dry fibrinous pericarditis can be idiopathic, that is, it does not have a specific cause for the pathology.
Acute pericarditis can be dry (fibrinous), exudative (serofibrinous, fibrinous-purulent), with or without cardiac tamponade.
As fibrinous pericarditis progresses, exudative pericarditis may develop. For example, serous-fibrinous pericarditis is diagnosed when a significant volume of serous-fibrinous effusion accumulates in the pericardial cavity. If purulent effusion forms in the pericardial sac, then the diagnosis is fibrinous-purulent pericarditis.
Complications and consequences
Fibrinous pericarditis, if left untreated, is often complicated by adhesion of the pericardial leaflets, as well as by myocardial conduction disorders. In advanced pathological processes, symptoms are present and worsen over a long period of time. Pericardial noise in many patients remains even after treatment.
Cardiac tamponade occurs when the pressure in the pericardium is high enough to prevent the right side of the heart from filling.[ 10 ]
Patients may complain of chest pain and difficulty breathing after physical activity, which is caused by the increase in the volume of the heart muscle and the contact of dense pericardial leaflets. Most often, this condition is not treated, but is observed dynamically.
Even after a favorable outcome of fibrous pericarditis, patients may experience arrhythmia attacks. The inflammatory reaction changes the impulse susceptibility of the myocardium, which can provoke the appearance of paroxysmal tachycardia, atrial and ventricular fibrillation, and blockades. With regular heart rhythm disturbances, heart failure may develop.
Diagnostics fibrinous pericarditis
The diagnosis of acute fibrinous pericarditis can be made if the patient exhibits the typical triad: [ 11 ], [ 12 ]
- heart pain;
- pericardial friction rub;
- characteristic ECG picture.
Instrumental diagnostics usually include ECG, echocardiography and chest X-ray to exclude the presence of exudate.
The ECG shows a concordant ST wave convex downwards no more than 7 mm, with a transition to high T without accompanying reciprocal depression of ST in other leads. Fibrinous pericarditis for 1-2 days is accompanied by an elevation of the segment, covering all standard leads with a limit in the second standard lead. [ 13 ]
The main auscultatory sign of fibrinous dry pericarditis is the friction noise of the pericardial leaflets. It is felt in the area of the left lower edge of the sternum, in the area of absolute cardiac dullness. The noise is heard synchronously with heart contractions, has no connection with respiratory movements, but is variable and tends to increase when pressed with a phonendoscope. It disappears with the appearance of exudate. The nature of the noise is sometimes soft, more often rough, scraping, can be felt when palpating.
Pericardial friction rub in fibrinous pericarditis can be continuous (systolic-diastolic), two-component (ventricular systole and rapid filling of the left ventricle) or three-component (the so-called “locomotive rhythm”).
During the diagnosis of fibrinous pericarditis, it is necessary to obtain micro and macro preparations, which is only possible by performing a histological examination of part of the biomaterial removed during a pericardial biopsy.
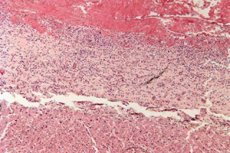
Microslide of fibrinous pericarditis:
- under low microscopic magnification, pronounced fibrin deposits with a characteristic lilac-pinkish color are visualized on the epicardial surface;
- leukocytes are observed between the fibrinous fibers;
- epicardial vessels are dilated and full-blooded.
Macrodrug of fibrinous pericarditis:
- thickening of the epicardium (visceral pericardial layer);
- whitish-grayish color, coarse fibrous film;
- "hairy" heart;
- depending on the outcome of the disease: fibrin breakdown and resolution of the inflammatory process, or the formation of adhesions (“armored” heart).
The term fibrinous pericarditis is often associated with the concept of "hairy heart", which is caused by the deposition of a large amount of proteins and fibrinous threads on the pericardial layers, which gives the heart a peculiar "hairiness".
Laboratory tests (particularly a complete blood count) are general in nature and can help determine the origin of the disease and assess the intensity of inflammation.
Differential diagnosis
Differential diagnosis of fibrinous pericarditis is carried out:
- with myocardial infarction;
- with dissecting aortic aneurysm;
- with pulmonary embolism;
- with spontaneous pneumothorax;
- with angina pectoris;
- with myopericarditis;
- with pleurisy;
- with herpes zoster;
- with esophagitis, esophageal spasm;
- with acute gastritis, stomach ulcer.
Differential ECG signs:
With fibrinous pericarditis |
In acute myocardial infarction |
|
ST segment |
The changes are diffuse, combined with a positive T wave. A return to the isoline is noted over several days. |
The changes are local, discordant, in combination with a negative T wave. In patients with an uncomplicated course, the ST segment returns to the isoline within a few hours. |
PQ or PR interval |
Depression of the interval is noted. |
No changes. |
Q wave, QS complex |
Atypical pathological Q wave. |
Pathological Q wave develops rapidly. |
Atrial and ventricular arrhythmias |
Not typical. |
Typical. |
The difference between fibrinous pericarditis and acute coronary syndrome:
- With the development of fibrinous pericarditis, pains often appear suddenly, with retrosternal or epigastric localization. The nature of the pains is acute, persistent, dull, aching, sometimes squeezing, constant (increasing-decreasing). Nitroglycerin is ineffective.
- In acute coronary syndrome, the pain increases, radiating to the shoulder, forearm, upper limb, and back. The pain is paroxysmal: attacks last for about half an hour. The patient's body position does not affect the severity of the pain syndrome. After taking Nitroglycerin, the symptoms subside.
Who to contact?
Treatment fibrinous pericarditis
The patient is prescribed strict bed rest for a period of up to 7-14 days (then - depending on the course of the disease), diet table No. 10 (10A).
If it is possible to determine the cause of the development of fibrinous pericarditis, then, according to indications, antibiotics, antiparasitic, antifungal and other drugs are prescribed.
Antibiotics are used when there is an obvious infectious factor - for example, sepsis, pneumonia, tuberculosis, purulent foci, etc.
Antiviral drugs are prescribed when the viral origin of the disease is proven:
- cytomegalovirus requires the use of immunoglobulin once a day 2-4 ml/kilogram according to the scheme;
- Coxsackie virus requires the administration of interferon-A;
- For adenovirus and parvovirus B19, immunoglobulin 10 g is used intravenously.
Pathogenetic treatment involves the use of the following drugs:
- Nonsteroidal anti-inflammatory drugs – have analgesic, anti-inflammatory, and mild immunosuppressive effects. It is appropriate to use acetylsalicylic acid, Voltaren (0.05 g three times a day), Ibuprofen (0.4 g three times a day), and Meloxicam (0.015 g twice a day). [ 14 ]
- Glucocorticosteroids – have a strong anti-inflammatory, anti-shock, immunosuppressive effect. They are prescribed when non-steroidal anti-inflammatory drugs are ineffective.
In the idiopathic variant of fibrinous pericarditis and the absence of active foci of inflammation, antibiotics are not the drugs of choice. The treatment regimen includes non-steroidal anti-inflammatory drugs (Diclofenac 150 mg/day, Meloxicam 15 mg/day, Ibuprofen three times a day at 200 mg), as well as Colchicine (1 mg/day), corticosteroids (1 mg/kilogram). [ 15 ], [ 16 ]
Surgical treatment is appropriate if the patient develops constrictive pericarditis, if serous-fibrinous pericarditis recurs, or if drug therapy is ineffective. Pericardiocentesis is the treatment of choice for cardiac tamponade. If this recurs, a pericardial window may be performed. Pericardiectomy is the treatment of choice for constrictive pericarditis. [ 17 ]
Prevention
There is no specific prevention for the development of fibrinous pericarditis. Doctors suggest following the following recommendations to reduce the risk of such complications:
- Quit smoking, avoid visiting smoking areas (passive smoke inhalation). It has been proven that smoking even five cigarettes daily increases the risk of developing cardiovascular diseases by almost 50%.
- Stick to a low-cholesterol diet, reduce the consumption of saturated fats (fatty meat and lard should be replaced with white meat and seafood), introduce cereals, vegetables, greens, fruits, and vegetable oils into the diet.
- Reduce salt intake to 3-5 g per day, which will reduce the risk of developing cardiovascular diseases by 25%.
- Introduce foods rich in magnesium and potassium into your diet (seaweed, dried fruits, apricots, pumpkin, buckwheat, bananas).
- Monitor your body weight and eat a balanced diet.
- Ensure adequate physical activity (walking, swimming, cycling – at least half an hour daily or five times a week).
- Regularly monitor fat metabolism indicators, visit a doctor for preventive diagnostics.
- Limit or eliminate alcohol consumption.
- Avoid deep and prolonged stress.
Even making small changes to your lifestyle can significantly slow down the development of heart and vascular pathologies. It is important to understand that it is never too late to start living a healthy lifestyle. If any signs of heart disease do appear, you should see a doctor without delay, preventing the disease from progressing and the symptoms from worsening.
Forecast
It is difficult to assess the prognosis of the disease, since it is relatively rarely detected during the patient's lifetime. In general, the following are considered criteria for an unfavorable prognosis:
- a significant increase in temperature (above 38 degrees);
- subacute onset of symptoms;
- intense exudation into the pericardial sac;
- development of cardiac tamponade;
- no positive response to acetylsalicylic acid or other nonsteroidal anti-inflammatory drugs after at least 7 days of treatment.
If fibrinous pericarditis is not treated, the risk of death increases significantly, primarily due to the development of complications and intoxication. [ 18 ] Patients who have had this disease should be under regular supervision of a cardiologist.

