Medical expert of the article
New publications
Paracoccidia are the causative agents of paracoccidioidosis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Paracoccidioidomycosis (synonyms: South American blastomycosis, Lutz-Splendore-Almeida syndrome) is a chronic mycosis characterized by lesions of the lungs, skin, mucous membranes of the oral cavity and nose, a progressive course with the development of a disseminated form of the disease. The causative agent is Paracoccidioides braziliensis.
 [ 1 ]
[ 1 ]
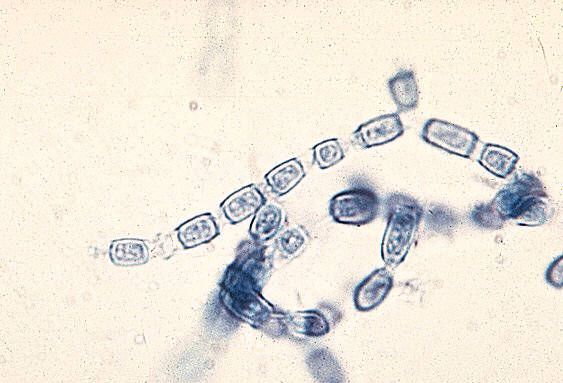
Morphology of paracoccidia
A dimorphic fungus that forms a yeast phase at 37 °C. Yeast cells are large (10-60 µm) with multiple buds 2-10 µm in diameter. The mycelium of the fungus is thin, septate, and forms chlamydospores. Microconidia are 2-3 µm in size.
Cultural properties of paracoccidia
The fungus is undemanding to the nutrient substrate, actively reproduces in sterile soil, vegetable particles, water. On natural substrates (yeast extract, soil extract) intensive sporulation is observed. At 25 °C it grows with the formation of hyaline hyphae, and at 37 °C it forms large spherical yeast cells with many budding cells, which gives this structure the characteristic appearance of a "sea steering wheel".
Biochemical activity of paracoccidia
When yeast cells are grown in a nutrient medium, a fungicidal metabolite accumulates, similar in chemical structure to phenol and benzoic acid, causing protein denaturation.
Antigenic structure of paracoccidia
When grown in liquid medium for 3 days, the mycelial form produces exoantigens 1, 2, 3, which can be determined using immunodiffusion in gel.
Ecological niche of paracoccidia
Soil of endemic areas in South America, especially Brazil, but also in Mexico and Costa Rica.
Environmental persistence of paracoccidia
The yeast phase is unstable in the external environment. The mycelium is resistant to changes in pH, temperature fluctuations, and drying. It is very sensitive to the antagonistic action of normal microflora in the environment.
Antibiotic sensitivity
Paracoccidia are sensitive to ketoconazole, itraconazole, amphotericin B, trimethoprim/sulfamethoxazole.
Sensitivity to antiseptics and disinfectants
Paracoccidia are sensitive to the action of commonly used antiseptics and disinfectants.
Pathogenesis of paracoccidioidosis
Infection occurs with microconidia. The lesions are located on the skin, mucous membrane of the cornea, nose, and lungs. Skin lesions are ulcerative in nature, with areas of suppuration and scarring alternating within them. With dissemination, bones, adrenal glands, liver, brain, skin, and mucous membranes are affected. In all patients, the spleen is involved in the inflammatory process.
Cellular immunity. Its intensity and duration have not been studied.
Epidemiology of paracoccidioidosis
The source of the infectious agent is the soil of endemic zones. The transmission mechanism is airborne, the transmission route is airborne and dusty. The susceptibility of the population is unknown, rural residents predominate among those infected. The patients are safe for others.
Symptoms of paracoccidioidosis
Only people get sick. Painless ulcers form on the mucous membrane of the oral cavity or nose. Usually the lesions are multiple, less common are single pustular lesions or subcutaneous abscesses. Ulcerative lesions of the skin and mucous membranes are accompanied by an increase in regional lymph nodes. Pulmonary lesions are accompanied by symptoms such as: cough, chest pain, formation of infiltrates.
Laboratory diagnostics of paracoccidioidomycosis
The materials examined include pus, cerebrospinal fluid, sputum, urine, and lymph node puncture.
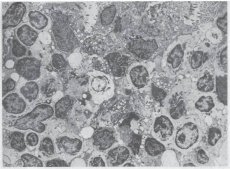
Microscopic examination involves studying native or Gram-, Romanovsky-Giemsa- and other-stained smears from the material being examined. Fungal cells are large, round or ellipsoidal in shape, and have thick walls. The mother cell is surrounded by small daughter buds and looks like a crown. Similar cells are also found in tissue sections. The morphology of the yeast phase is very characteristic, so when such fungal cells are detected, the diagnosis is beyond doubt.
To isolate a pure culture, the material is seeded on nutrient media with carbohydrates, blood and serum agar, which are incubated at 25-30 and 37 °C to obtain mycelial and yeast colonies, respectively. The pathogen grows slowly, forming colonies resembling yeast colonies after 3 weeks.
The bioassay is carried out on mice or guinea pigs, infecting them intraperitoneally with the material to be tested and isolating a pure culture from their internal organs.
Serological testing determines antibodies in the serum of patients in RP, ELISA or RSC, especially in the late stages of the disease. RP and RSC are of diagnostic value.
An allergy test is performed with an allergen from the tissue form of the fungus.

