Medical expert of the article
New publications
Eggs and ovogenesis
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Unlike male reproductive cells, egg cells reproduce, their number increases in embryos, female fetuses, i.e. when the fetus is still in the womb. In this case, so-called primordial follicles are formed, located in the deep layers of the ovarian cortex. Each such primordial follicle contains a young female reproductive cell - oogonia, surrounded by one layer of follicular cells. Oogonia repeatedly divide mitotically, turning into primary oocytes (first-order oocytes), which are preserved in the girl's ovary until her puberty. By the beginning of puberty, the ovaries contain about 300,000 primary oocytes, each about 30 µm in diameter. Together with the surrounding two layers of follicular epithelium cells, the primary oocyte makes up the primary follicle.
In girls during puberty and in sexually mature women, most primary oocytes die. During a woman's life, only 400-500 eggs mature. Every 21-28 days, according to the individual menstrual cycle, usually one follicle (or, less often, two) reaches maturity. The diameter of a mature (vesicular) follicle reaches 1 cm. The remaining follicles growing at this time undergo reverse development - atresia. At the site of death of such immature and dead follicles, structures remain, called atretic bodies.
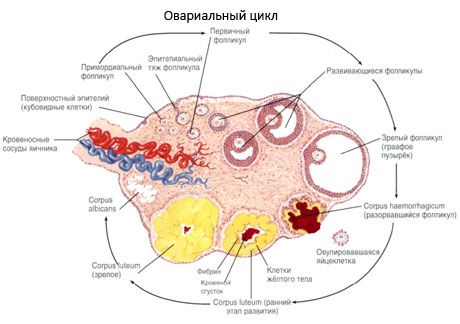
During the maturation process, the primary oocyte goes through the stages of meiosis. As a result of meiotic division, a secondary oocyte is formed, which already has a single (haploid) set of chromosomes (n=23), and a small, so-called polar body with the same (n=23) set of chromosomes. In this case, the primary follicles turn into secondary follicles. Liquid accumulates inside such follicles, and two membranes are formed around each secondary oocyte - the cytolemma and a layer of follicular cells. Thus, the secondary follicle turns into a vesicular (mature) follicle filled with follicular fluid.
During the growth and development of the primary follicles, the egg increases in size. A transparent membrane of glycosaminoglycans and other substances forms around it, and around this membrane there is a layer of cubic follicular cells secreting follicular fluid containing female sex hormones - estrogens. At this time, the egg is surrounded by follicular cells and, together with the latter, it shifts to the wall of the follicle, where it forms an egg-bearing hillock (cumulus oophorus). Thus, the primary follicle turns into a secondary (vesicular). The oocyte no longer increases in size, the follicles themselves continue to grow larger. In this phase, the oocyte, together with the surrounding transparent membrane (zona pellucida) and the layer of follicular cells called the radiant crown (corona radiata), moves to the top of the growing follicle. As the follicle grows in size, the connective tissue around it thickens and forms an outer membrane - the theca folliculi. Numerous blood capillaries grow into this membrane.
The theca has two layers: internal and external. The internal layer of the theca (shell) near the blood capillaries contains numerous interstitial cells, and the external layer (shell) of the theca consists of dense fibrous connective tissue. Inside the mature follicle, reaching 1 cm in diameter, there is a cavity containing follicular fluid (liquor follicularis).
As the follicle matures, it gradually reaches the surface layer of the ovary. During ovulation, the wall of such a follicle ruptures, the egg along with the follicular fluid enters the peritoneal cavity, where it gets on the fimbria of the tube, and then into the abdominal (peritoneal) opening of the fallopian tube. At the site of the ruptured follicle, a blood-filled depression remains, in which the corpus luteum is formed. If fertilization of the egg does not occur, the corpus luteum is small in size (up to 1.0-1.5 cm), does not exist for long and is called the cyclic (menstrual) corpus luteum (corpus uteum ciclicum, s.menstruationis). Later, it grows with connective tissue and is called the whitish body (corpus albicans), which dissolves after some time. If the egg is fertilized, pregnancy occurs, the corpus luteum graviditatis increases in size, reaches 1.5-2.0 cm in diameter and exists throughout the pregnancy, performing an endocrine function. Later, it is also replaced by connective tissue and turns into a whitish body (corpus albicans). In places of ruptured follicles, depressions and folds remain on the surface of the ovary; their number increases with age.
What do need to examine?


 [
[