Medical expert of the article
New publications
Osteophytes of the cervical spine
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
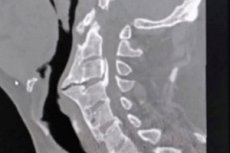
Spondylophytes or osteophytes of the cervical spine are bony outgrowths (from Greek osteon - bone and phyton - outgrowth) that can form on any of the seven cervical vertebrae by endochondral ossification, that is, ossification of cartilage.
Epidemiology
The formation of osteophytes in various parts of the spine is a common pathology, and their formation can begin after the age of 25. Clinical statistics show that more than 75% of people over 65 years of age have degenerative changes in the cervical spine of various degrees, including cervical osteophytes. [1], [2]
Among the elderly, the prevalence of anterior osteophytes in the cervical region is estimated to be 20-30%. [3]
Osteophytes can form at any level of the cervical region, but are most common at the C5-6 and C6-7 vertebrae.
Causes of the osteophytes of the cervical spine
A vertebral osteophyte of any localization, often referred to as a bone spur, is defined by NASS (North American Society of Vertebrologists) experts as a bony overgrowth near the edge of an intervertebral disc coming from the bone growth plate and the site of attachment of the disc to the vertebral body - the apophysis of the vertebral body. Such cervical marginal osteophytes have a broad base and can develop both near the edges of the bony-cartilaginous closure (end) plates of vertebral bodies (which are located between the spinal bones and intervertebral discs) and at the arcuate (facet or zygapophyseal) joints connecting the bodies of neighboring vertebrae.
In most cases, abnormal bony growths on the vertebrae are the result of osteoarthritis of the cervical spine, also called cervical spondylosis, which experts believe develops with age due to normal aging and wear and tear of spinal joint structures, including cartilage.
Osteophytes can also be caused by damage or inflammation of the ligaments and tendons around the bones and joints of the cervical spine; degenerative processes in the cervical spine affecting the vertebral body closure plates and intervertebral discs (nucleus pulposus and annulus fibrosus) - cervical osteochondrosis; disruption of the position of the vertebral joints - dislocation of the cervical vertebrae.
Risk factors
Specific risk factors for cervical bone spurs include:
- Cervical spine injuries;
- Excessive or insufficient physical activity;
- Age-related wear and tear and impaired cushioning function of intervertebral discs due to degenerative changes in their structure;
- Spinal instability, in which degeneration (sclerosis or hardening) of the vertebral closure plates, defined as discogenic vertebral sclerosis, develops due to increased activity of transforming growth factor-beta (TGFβ);
- Heredity and the presence of anomalies of the vertebral bodies and facet joints;
- Posture disorders;
- Cervical scoliosis;
- Diffuse idiopathic skeletal hyperostosis with ossification of ligamentous structures of the spine. [4], [5]
See also - risk factors and causes of osteoarthritis
Pathogenesis
Cartilage-covered bony overgrowths in the cervical vertebral region often form along the peripheral edges of vertebral bodies composed of trabecular (spongy) bone.
Overgrowth occurs at the border between cartilage and the periosteum (periosteum) covering the bone tissue, which is responsible for the growth and reparative regeneration of bone tissue and consists of two layers: the outer solid layer (formed by bundles of fibrous fibers) and the inner cambial (osteogenic) layer. The cambial layer is a collagen matrix with mesenchymal progenitor cells (stem cells), differentiated osteogenic progenitor cells (bone marrow stem cells), osteoblasts (immature bone cells) and connective tissue cells - fibroblasts.
The pathogenesis of osteophyte formation is associated with chondrogenic differentiation of highly self-renewing progenitor cells within the periosteum and is due to the cellular repair reaction - a protective and compensatory reaction - in response to articular cartilage and/or intervertebral disc damage.
Next, endochondral ossification occurs. Differentiating cells of cartilage tissue - chondrocytes - form the extracellular matrix of cartilage; chondrocytes proliferation is followed by their hypertrophy, and hypertrophied chondrocytes begin to suppress the expression of the main glycoprotein of cartilage tissue - type II collagen and produce collagen type X, which promotes bone formation, as well as bone morphogenetic protein BMP6 (inducing bone and cartilage growth), osteoblast differentiation-related transcription factor Runx2 and others.
As a result, it leads to destruction of intracellular cartilage matrix, its mineralization (deposition of hydroxyapatite crystals) and active differentiation of osteoblasts, which mature and, embedding in the matrix, transform into bone tissue cells - osteocytes.
Symptoms of the osteophytes of the cervical spine
Cervical osteophytes themselves do not hurt, but when they eventually begin to press on nerves, symptoms like:
- Pain of varying intensity in the neck region, which weakens at rest and increases with movement and may irradiate to the back of the neck, shoulder, arm or hand;
- Stiffness and muscle rigidity in the neck;
- Headaches;
- Numbness, burning and tingling sensations that can affect the shoulders, forearms and hands;
- Progressive weakness in one or both hands and/or arms with or without impaired finger mobility;
- Muscle spasms;
- Cervical osteophytes compress the back of the pharynx and esophagus, causing dysphagia. [6]
Osteochondrosis with osteophytes of the cervical region manifests itself in the same way, but its morphological feature is the presence of horizontal bony growths on the vertebral bodies - the so-called spines of Junghans.
Posterior cervical osteophytes are formed near the spinous process in the dorsal part of the spine, as well as with ossification of the posterior longitudinal ligament of the spinal column in the area of the cervical vertebrae. Such spondylophytes can cause severe pain due to mechanical pressure on the nerve trunks of the foraminal (intervertebral) foramen.
Anterior cervical osteophytes, which form in old age when the anterior longitudinal ligament of the spinal column ossifies in the cervical vertebrae, are usually asymptomatic. However, if the adjacent tissues swell and the bony growths compress the laryngeal nerve or esophagus, patients may experience vocal disturbances, difficulty swallowing, esophageal spasm, and shortness of breath.
Complications and consequences
A complication of osteophytes that form in the area of the uncovertebral junction (located between the hook-like processes of the cervical vertebral bodies) and point into the foraminal foramen and toward the spinal canal is the development of vertebral artery syndrome.
Complications and consequences of cervical osteophytes are also noted such as:
- Radicular syndrome - cervical radiculopathy;
- Spinal canal stenosis with various neurologic manifestations;
- Spinal cord compression with development of compression vertebrogenic myelopathy;
- Cervical facet syndrome;
- Development of vertebrobasilar syndrome.
Diagnostics of the osteophytes of the cervical spine
The presence of osteophytes is detected by cervical spine x-ray in three projections, as well as magnetic resonance imaging and computed tomography. Read more in the publications:
Differential diagnosis is made with disc herniation, ankylosing spondyloarthritis, osteochondroma of the cervical spine, pyrophosphate arthropathy, cervical myositis, myogelosis of the cervical spine, syringomyelia of the cervical spinal cord.
Who to contact?
Treatment of the osteophytes of the cervical spine
Osteophytes of the cervical spine do not always cause neck pain and other symptoms, meaning they do not always require treatment. By some estimates, about 40% of people with cervical bone spurs need symptom management.
In the presence of pain, symptomatic treatment involves the use of analgesics, and the main drugs are represented by non-steroidal anti-inflammatory drugs (NSAIDs); parenterally, corticosteroids may be used (in short courses); externally - various ointments for neck pain.
Long-term relief of symptoms - reducing pain and increasing neck mobility - is facilitated by such popular non-invasive methods as physical therapy (primarily therapeutic massage), LFK to increase range of motion, and acupuncture.
Read more:
- Drug treatment of osteoarthritis
- Local treatment of osteoarthritis
- Physiotherapy for osteoarthritis
- Physical therapy for osteoarthritis
Exercises for cervical osteophytes can be performed only if there is no acute pain. The exercises recommended by physiotherapists include:
- Slow left-right turns of the head, which should be performed with relaxed shoulders and back, repeating 10 times in each direction;
- Smooth arc-shaped turns of the head to the right-left with the chin up (several times in each direction):
- Tilting the head left-right to the shoulders, whereby pressing the opposite side of the head with the hand can slightly increase the tilt, creating a stretch on the opposite side of the neck. Hold the stretch for 10 seconds and repeat two or three times in both directions;
- Strengthening isometric rotation of the neck and stretching the muscles in the back of the neck, which is performed with the head stationary with the palm of the hand placed on the back of the head or slightly pressing the back of the hand to the chin. The optimal number of repetitions is at least ten.
When asked how to get rid of cervical osteophytes, AANS (American Association of Neurological Surgeons) experts say that osteophytes do not go away on their own, and the only way to get rid of them is osteophyte resection or osteophytectomy.
Therefore, in rare cases where conservative methods do not relieve symptoms or the patient's condition worsens due to the appearance of neurological problems, surgery may be considered as a last resort. In addition to osteophytectomy, surgery such as laminectomy with spondylodesis (fusion of adjacent vertebrae) and laminoplasty may be recommended to decompress the spinal cord, and radiofrequency ablation of the affected nerve may be recommended to eliminate pain.
At the same time, experts do not hide the fact that surgical intervention involves the risk of damage to nerves and spinal cord, as well as increased pain.
Prevention
Is it possible to prevent the formation of cervical osteophytes? General recommendations regarding the prevention of this pathology concern the notorious healthy lifestyle, especially the need for physical exercise.
Forecast
In terms of prognosis, if pain is present, it can become worse over time as osteophytes are able to progress, meaning they continue to grow, limiting physical activity. And as they grow, cervical spine osteophytes can compress nearby nerves, muscles, or other structures, significantly reducing quality of life.

