Medical expert of the article
New publications
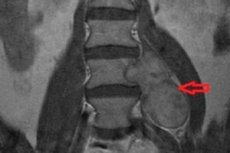
Neurinoma of the spine
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Spinal benign tumor of the peripheral nervous system - spinal neurinoma - takes its development on the basis of schwann cells responsible for the formation of the epineurium. Another name for this neoplasm is schwannoma.
The pathological focus is characterized by relatively slow growth - about 2 mm per year. Despite this, over the years, the tumor can reach a fairly large size, which has an extremely negative impact on the quality of life of the patient. Treatment of pathology is surgical. [1]
Epidemiology
Spinal neurinoma is a spinal benign neoplasm with slow growth. The pathological focus is capable of affecting any of the departments of the peripheral nervous system and develops on the basis of its structural part - Schwann cells, which are able to grow both inside (in 70% of cases) and from the outer part (in 20% of cases) of the dural medulla. In 10% of cases, they leave the cerebrospinal canal along the course of the peripheral nerve through the foraminal foramen.
The most common sites of neurinoma development are thought to be:
- Pontine cerebellar angle (acoustic neurinoma);
- Sensitive nerve endings of the spinal cord (spinal neurinoma).
The latter most often occurs in the upper-middle spinal segments (cervical-thoracic spine - in 75% of cases). The lumbosacral spine is affected in 25% of cases.
The greatest danger is not so much the neurinoma itself, but the surrounding tissues that are affected. The neoplasm usually has a connective tissue capsule and accounts for about 30% of all primary benign tumors of the spine. Pathology affects with equal frequency representatives of the male and female sex.
Spinal neurinoma is capable of occurring regardless of age, but most cases are diagnosed in patients 40-60 years old. [2]
Causes of the spinal neurinomas
Scientists cannot yet name the exact causes of the development of spinal neurinoma. However, they do not rule out the involvement of the following provoking factors:
- Hereditary predisposition;
- Radiation, radiation exposure;
- Spinal injuries;
- Internal intoxication, prolonged negative effects of toxic, chemical substances.
Many patients have neurinoma and neurofibromatosis at the same time, which can also be considered a factor that increases the likelihood of tumor development. In addition, the spinal lesion may be a manifestation of multiple pathologies, in which similar neoplasms are found elsewhere in the body.
Often, spinal neurinoma is accompanied by a gene mutation in chromosome 22: a protein that restricts the fusion of schwann cells is incorrectly encoded. The "incorrect" protein promotes the overgrowth of the nerve's myelin sheath. This change in genotype can be accidental or inherited. For example, in patients with neurofibromatosis type 2 (with autosomal dominant inheritance), neurinoma is found in 50% of cases. [3]
Risk factors
Some predisposing factors that contribute to the development of spinal neurinoma include:
- Teratogenic effects on the fetus during pregnancy;
- Prolonged intoxication of any genesis;
- Trauma, spinal disorders of various origins;
- Neurofibromatosis, unfavorable oncologic heredity;
- The presence of other tumors in the body, both malignant and benign.
The danger of neurinoma in children is sharply increased if at least one of the parents was found to have this pathology. [4]
Pathogenesis
A spinal neurinoma is a capsular, rounded, clearly delineated, lumpy mass. In section, the tumor is brownish-brown or grayish, has multiple areas of fibrosis, sometimes - cysts with brown liquid content.
As the neurinoma develops and grows, nearby tissues and structures are compressed, which determines the clinical symptomatology.
Microscopic examination of the neoplasm reveals parallel cell rows with rod-shaped nuclei alternating with tissue fibers. On the periphery of the focus there is a developed vascular network, which is not the case with the central part. It is for this reason that dystrophic changes often occur in the center. The morphological structure changes, epithelioid, xanthomatous, angiomatous neoplasia is noted.
Symptoms of the spinal neurinomas
The initial stages of spinal neurinoma development are usually not accompanied by any pronounced symptomatology. The first signs appear when the neoplasm begins to compress nearby structures. Patients most often talk about the following symptoms:
- Increasing, constantly bothering pain in the back, mainly in the area of localization of the pathological focus, not disappearing after taking standard drugs (analgesics, non-steroidal anti-inflammatory drugs);
- Irradiation of pain to the extremities (upper or lower), scapula, shoulder;
- Bladder and/or bowel disorders;
- Increasing weakness in the muscles of the limb;
- Loss of ability to work, decreased motor skills;
- Numbness of a part of the body or limbs below the affected area (tingling, burning, feeling of "crawling goosebumps");
- Decreased libido.
In severe cases, partial or complete paralysis may develop. [5]
Features of symptomatology are in close dependence on the localization and volume of the neoplasm. [6]
- Neurinoma of the cervical spine is often manifested by pain in the upper extremities. Turning and tilting the head becomes painful. There may be tinnitus, pain in the head, irritability, sleep disturbance, paresthesias.
- Neurinoma of the thoracic spine is accompanied by shingling pain in the chest, scapula. There may be weakness in the arms. Back pain, as a rule, sharp, intense, the patient becomes difficult to perform any activity, including everyday activities.
- Neurinoma of the lumbar spine provokes pain in the back of the corresponding localization, with innervation to the lower extremities. The patient becomes difficult to walk, sometimes there are failures in the work of the pelvic organs. There may be numbness in the legs and lower back, decreased sensation.
Complications and consequences
The most common adverse effects of spinal neurinoma are paresis and paralysis - complications that are accompanied by weakening or inability to perform voluntary movements. This problem is associated with compression of spinal structures by the tumor: with strong pressure, paralysis occurs, and with weak pressure, paresis occurs.
Against the background of the lesion of the motor apparatus develop trophic disorders, decreased muscle tone.
The radicular pain syndrome is manifested by constant and severe pain along the course of the spine, possible sensory and motor problems in the area of nerve innervation.
The autonomic nervous system suffers: over time there are disorders of urination, intestinal emptying, and when the thoracic section is affected - arrhythmias, digestive disorders.
As the neoplasm, a spinal neurinoma, grows, the functions for which the spinal structures below the level of the lesion are responsible are impaired. Tactile and temperature sensitivity on the affected side and pain sensitivity on the opposite side are reduced. Limb movements are either weakened or become impossible. [7]
Diagnostics of the spinal neurinomas
Spinal neurinoma is detected through comprehensive diagnostic measures.
The tests are generally informative in nature. As a rule, general and biochemical blood tests, urine analysis are prescribed.
Instrumental diagnosis in spinal neurinoma is represented by the following investigations:
- MRI - magnetic resonance imaging with contrast - is the most informative procedure that allows visualizing the neoplasm even of relatively small size, as well as assessing the degree of compression of surrounding tissues;
- CT scanning allows only large neurinomas to be viewed and involves the use of contrast enhancement;
- Ultrasound is not sufficiently informative, but can sometimes be used as part of differential diagnosis;
- Radiography allows identification of bony changes due to tumor growth;
- Biopsy - is performed to find out the structural characteristics of the neoplasm.
CT manifestations of spinal neurinoma:
- The neoplasm is encapsulated and clearly demarcated;
- There may be a cystic component, combined with neurofibromatosis;
- Can spread extradurally through the intervertebral foramen.
Spinal nerve root neurinoma is located more often in the cervical and thoracic spine. Neurofibromatosis patients may have multiple neoplasms.
Mandatory consultations of a neurologist, oncologist, surgeon, rheumatologist, traumatologist. [8]
Differential diagnosis
Spinal neurinomas are differentiated from other possible tumor processes.
A pontine cerebellar neoplasm should be distinguished from astrocytomas, meningiomas, and cerebellar tumors.
Spinal neurinoma proper is differentiated from other extramedullary tumors.
Peripheral nerve damage is distinguished from neuropathy of ischemic-compression or inflammatory origin.
With back pain perform differential diagnosis with aortic aneurysm dissection, acute renal colic, acute pancreatitis, infectious lesions of the spinal column, primary and metastatic malignant tumors, spinal compression fracture, seronegative spondyloarthritis.
Who to contact?
Treatment of the spinal neurinomas
In the early stages of spinal neurinoma development, a conservative treatment option may be chosen, but in practice this rarely happens: experts recommend removing the tumor without waiting until it begins to show pathological symptoms, squeezing the surrounding structures.
If you still consider conservative methodology, it may include taking analgesics and antispasmodics, as well as diuretics and medications that improve blood circulation in the area of the spinal column.
Among the cardinal surgical techniques, open surgery and radiosurgery lead the way in terms of efficacy.
Endoscopic method is used to remove not very large spinal neurinomas together with the capsule. Radiosurgery is used if scalpel intervention is not possible or if the patient refuses to undergo surgery. [9]
Medications
Drug therapy for spinal neurinoma is prescribed on an individual basis and may include the following drugs:
- Non-selective cyclooxygenase inhibitors 2:
- Diclofenac 75-150 mg per day in two doses
- Ketorolac 20 mg per day in two doses (for 3-5 days);
- Dexketoprofen 25-75 mg per day in 1-2-3 doses;
- Ketoprofen 100-300 mg per day in 2 doses;
- Lornoxicam 8-16 mg per day in 2 doses.
Possible side effects of taking the drugs for too long: dyspepsia, peptic ulcer disease, gastrointestinal bleeding, aggravation of cardiovascular disease.
- Selective cyclooxygenase inhibitors 2:
- Nimesulide 200 mg per day in 2 doses;
- Celecoxib 200-400 mg per day in 2 doses.
Possible side effects: nausea, vomiting, abdominal pain, skin itching, bitterness in the mouth, with prolonged use - ulcers of the GI mucosa.
- Myorelaxants - at signs of muscle spasm, short courses - no more than one week. Prolonged use is limited by side effects (weakness, dizziness, low blood pressure):
- Tizanidine 2-4 mg 2-3 times a day;
- Tolperisone 150 mg three times a day.
Other types of drug therapy - according to individual indications and at the discretion of doctors.
Surgical treatment
Spinal neurinoma in the vast majority of cases requires its removal. A wait-and-see approach is rarely practiced, as there is a high risk of developing adverse health and life complications, including malignization of the tumor process. In addition, neurinomas often grow to a large size, and treatment becomes more complicated and the risk of complications increases significantly.
Endoscopic and microsurgical removal of tumors, radical intervention for tumors of large size are standard.
The course of surgery varies depending on the location and size of the neoplasm. If the neurinoma is localized in the spinal canal, a gentle microsurgical intervention is performed, which makes it easier for the patient to recover. The pathological focus is removed with the help of neurosurgical instruments, microscopic equipment and neurophysiological monitoring. The nerve is isolated from the neoplasm and placed according to its anatomical location.
The main contraindication to surgical intervention is infection in the area of the incision. Treatment may be postponed in pregnancy, certain diseases of the cardiovascular system, as well as in case of renal or respiratory failure in the patient. [10]
After surgery, the patient stays about 5-7 days on hospital observation, receives medication support and care of the postoperative wound. As a rule, full recovery is reported in about 2 months, provided that all recommendations of doctors are followed.
The operated patient is advised:
- Avoid lifting heavy objects and loads;
- Do not engage in sports involving stress on the spine and the risk of back injury;
- Stick to a healthy diet.
Prevention
Scientists can not name the exact causes of spinal neurinoma, the disease occurs sporadically - that is, randomly due to the transformation of schwann cells. On this basis, the primary prevention of neoplasm is not in question.
If you have a family history of neurofibromatosis type 2 or other spinal tumors, you should be vigilant about your health and periodically perform diagnostic measures - especially if any suspicious symptoms or complaints arise.
According to experts, the risks of developing spinal neurinoma are increased:
- Exposure to radiation, ionizing radiation;
- Severe fluctuations in hormones;
- Aggressive external factors (exposure to chemical toxic substances, unfavorable environmental conditions, etc.);
- Improper diet;
- Trauma to the spinal column.
It is important to lead a healthy lifestyle, and if you notice any suspicious symptoms - do not delay to visit a doctor. Do not self-medicate - it is dangerous.
Forecast
The outcome of spinal neurinoma can be called favorable only if the tumor was timely detected and removed. In almost all patients, the neoplasm is removed without problems and completely, recurrences are rare.
The most frequent and complex problem that patients may face if left untreated is paralysis, which develops in 50% of cases. Surgical intervention performed as early as possible can prevent muscle atrophy and speed up the recovery of patients.
Spinal neurinoma is a pathology that in principle cannot be treated conservatively. Therefore, the preferred option for its elimination is surgery. The choice of a wait-and-see approach can only be applied to small and non-progressive neoplasms detected by chance.

