Medical expert of the article
New publications
Mycoplasma pneumonias
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Causes mycoplasma pneumoniae
Mycoplasmas are a special type of microorganism. They do not have a cell wall. In morphology and cellular organization, mycoplasmas are similar to L-forms of bacteria, and in size they are close to viruses.
12 species of mycoplasma have been isolated from the nasopharynx and urogenital tract of humans, but only three have pathogenic properties for humans: Mycoplasma pneumoniae, Mycoplasma hominis, Mycoplasma urealyticum.

M.pneumoniae affects the mucous membrane of the respiratory tract, and M.hominis and M.urealyticum affect the genitourinary system (cause the development of urethritis, cervicitis, vaginitis).
Symptoms mycoplasma pneumoniae
Mycoplasma pneumoniae is a common cause of respiratory tract infections. M.pneumoniae was first isolated in 1930 during a study of atypical pneumonia, and in 1962 it was characterized and classified as a separate species of bacteria.
The disease is transmitted by airborne droplets.
According to V. I. Pokrovsky (1995), all clinical manifestations of mycoplasma pneumonia are grouped as follows.
- Respiratory
- upper respiratory tract (pharyngitis, tracheitis, bronchitis);
- pulmonary (pneumonia, pleural effusion, abscess formation).
- Non-respiratory
- hematological (hemolytic anemia, thrombocytopenic purpura);
- gastrointestinal (gastroenteritis, hepatitis, pancreatitis);
- musculoskeletal (myalgia, arthralgia, polyarthritis);
- cardiovascular (myocarditis, pericarditis);
- dermatological (polymorphic erythema, other rashes);
- neurological (meningitis, meningoencephalitis, peripheral and cranial neuritis, cerebellar ataxia);
- generalized infections (polylymphoadenopathy, septicopyemia).
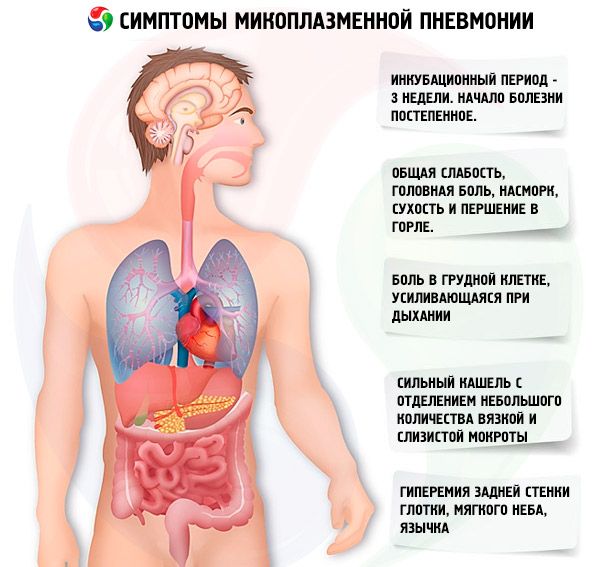
Mycoplasma infection has an incubation period of 3 weeks on average. The development of pneumonia is preceded by clinical manifestations of upper respiratory tract lesions. The onset of the disease is gradual. Patients are bothered by moderate general weakness, headache, runny nose, dry and sore throat, cough (initially dry, then with the separation of viscous mucous sputum). Characteristic features of cough are its duration and paroxysmal nature. During a coughing attack, its intensity is quite pronounced. Hyperemia of the posterior pharyngeal wall, soft palate, and uvula is constantly observed. With the development of bronchitis, harsh breathing and dry wheezing are heard. With a mild course of mycoplasma ARI, catarrhal rhinitis and pharyngitis are mainly observed. With a moderate course, there is a combined lesion of the upper and lower respiratory tract in the form of rhinobronchitis, pharyngobronchitis, nasopharyngobronchitis. The body temperature of patients is usually subfebrile.
The above symptoms of mycoplasma infection increase by the 5th-7th day, the body temperature rises to 39-40°C and can remain at these figures for 5-7 days, then it decreases to subfebrile and remains for 7-12 days, sometimes longer. A characteristic sign of mycoplasma pneumonia is a prolonged and severe cough with the release of a small amount of viscous and mucous sputum. The cough continues for at least 10-15 days. The vast majority of patients also experience chest pain, which intensifies with breathing.
Physical signs of pneumonia usually appear on the 4th-6th day of illness and are characterized by focal weakening of vesicular breathing, crepitation, fine bubbling rales, shortening of percussion sound, but this is an uncommon sign. Approximately 20% of patients do not have physical signs of pneumonia, lung damage is diagnosed only by X-ray examination.
Some patients may develop fibrinous or moderately exudative pleurisy.
Where does it hurt?
What's bothering you?
Diagnostics mycoplasma pneumoniae
Radiologically, mycoplasma pneumonia may have the following manifestations:
- strengthening and thickening of the pulmonary pattern, mainly interstitial changes in 50% of cases;
- segmental and focal infiltration of lung tissue (in 30% of patients); the infiltrate is localized mainly in the lower pulmonary fields, less often in the upper and middle lobes of the right lung, in the basal segments. Infiltrates are heterogeneous and non-homogeneous, without clear boundaries; in 10-40% they are bilateral;
- extensive lobar infiltration (rare variant).

 [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ]
Laboratory diagnostics of mycoplasma pneumonia
A general analysis of peripheral blood is characterized by a predominantly normal number of leukocytes (no more than 8 x 10 9 /l), in 10-15% of cases - leukopenia or leukocytosis; a regular increase in the number of lymphocytes; no shift in the leukocyte formula to the left; an increase in ESR.
It should be taken into account that mycoplasma pneumonia is often mixed (mycoplasma-bacterial) due to the addition of bacterial microflora (mainly pneumococcus). These are, as a rule, later pneumonias. Primary mycoplasma pneumonias develop in the first days of the disease. In general, the course of mycoplasma pneumonia is most often not severe, but long-term. However, in some cases, a severe course is possible; it is due to the severity of the pneumonia itself or the addition of non-respiratory manifestations of mycoplasma infection.
 [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ]
[ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ]
Diagnostic criteria for mycoplasma pneumonia
When diagnosing mycoplasma pneumonia, the following basic principles must be taken into account.
- Gradual onset with a short prodromal period, acute pharyngitis, rhinitis, tracheitis, intense prolonged cough with viscous, difficult to separate mucous sputum.
- Mild physical signs of pneumonia.
- The presence of extrapulmonary (extrarespiratory) manifestations: hemolytic anemia, myocarditis, pericarditis, hepatitis, skin rashes, polylymph adenopathy.
- Positive results of serological diagnostics. To confirm the diagnosis of mycoplasma pneumonia, antibodies to mycoplasma in the blood are determined using the complement fixation reaction; paired sera are examined at an interval of 15 days. A 4-fold increase in the antibody titer (not less than 1:64) is diagnostically significant.
Cultural diagnostics (sputum culture) is practically not used for mycoplasma pneumonia due to the need to use highly selective media and the low information content of the method.
- Detection of mycoplasma antigens in sputum using monoclonal antibodies using the immunofluorescence method or enzyme immunoassay. In recent years, mycoplasma (its DNA molecules) has been identified in sputum using the polymerase chain reaction method. Mycoplasma is not detected during routine bacterioscopy of a sputum smear.
What do need to examine?
Who to contact?
Treatment mycoplasma pneumoniae
Mycoplasma is highly sensitive to erythromycin and new macrolides (azithromycin, clarithromycin, etc.), and new macrolides are more effective than erythromycin and are considered first-line drugs. Tetracyclines are also effective against mycoplasma pneumonia. Mycoplasma is resistant to β-lactam antibiotics (penicillins, cephalosporins).
More information of the treatment
Drugs

