Medical expert of the article
New publications
Meningioma of the brain
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A well-defined, horseshoe-shaped or spherical tumor that develops on the base of the dura mater is a meningioma of the brain. The neoplasm resembles a peculiar nodule, which often fuses with the dural sheath. It can be both benign and malignant, with localization in any cerebral part. It is most often found in the hemispheres.
Treatment of the pathology is complex and combined: it includes a combination of radiation therapy, stereotactic radiotherapy (surgery), and surgical resection. [1]
Epidemiology
In almost nine out of ten cases, meningioma of the brain is benign in nature, but many experts classify it as a relatively malignant formation due to its unfavorable course and widespread signs of compression of brain structures.
Truly malignant meningioma is less common, but is characterized by an aggressive course and an increased likelihood of recurrence even after surgical resection.
Most commonly, meningioma of the brain affects:
- The large cerebral hemispheres;
- A large occipital opening;
- The pyramid of the temporal bone;
- The wings of the cuneiform bone;
- The tentorial notch;
- Parasagittal sinus;
- The pontocerebellar angle.
In the vast majority of situations, meningiomas have a capsule. Cysts, as a rule, are not formed. The average diametric size of the neoplasm ranges from a couple of millimeters to 150 or more millimeters.
When the tumor grows towards the brain structures, the pressure on the brain substance increases rather quickly. When the pathologic focus grows towards the cranial bones, it grows into the skull with further thickening and distortion of bone structures. Sometimes the neoplasm grows simultaneously in all directions.
Overall, meningiomas account for about 20% of all cases of head tumor processes. The incidence of specifically meningioma of the brain is estimated to be about 3 cases per hundred thousand population. Over the years, the risks of developing pathology increase: the peak of the disease occurs between 40 and 70 years of age, in women slightly more often than in men. In childhood, it occurs in only 1% of all pediatric tumors of the central nervous system.
In most cases, meningiomas of the brain occur singly. Multiple development occurs in about 10% of patients. [2]
Causes of the brain meningiomas
In many cases, experts attribute the development of brain meningioma to a genetic defect in chromosome 22. This defect is particularly common in patients with neurofibromatosis type II, an autosomal dominant inherited disease.
There is also a confirmed correlation of tumorigenesis with active hormonal changes in women. Abrupt changes in the hormonal background occur during pregnancy, with the onset of menopause, with cancer of the mammary glands, etc. It is noted that in female patients diagnosed meningiomas accelerate their growth with the onset of pregnancy.
Among other provoking factors, scientists emphasize:
- Head trauma (traumatic brain injury);
- Exposure to radiation (ionizing radiation, X-rays);
- Exposure to poisonous substances (intoxication).
There is no single reason for the development of the tumor process. Specialists are inclined to the theory of multifactorial occurrence of pathology. [3]
Risk factors
Experts have identified several factors that can increase the risks of brain meningioma.
- Hereditary predisposition. The involvement of a defect in chromosome 22 in the possible development of tumors has been scientifically proven. Such a violation is present in the owners of the gene for neurofibromatosis, which cause a high probability of meningioma in persons suffering from this hereditary pathology. The gene defect becomes a factor in the development of meningiomas in every second patient.
- Age predisposition. Meningioma of the brain is diagnosed in 3% of elderly patients (older than 50-60 years). The disease is practically uncommon in children.
- Female gender. Hormonal changes - in particular, occurring during pregnancy or against the background of breast cancer therapy - can affect the development of the tumor process in the brain.
- External negative influences - such as head injuries, radiation effects, intoxication.
Pathogenesis
Meningioma is a neoplasm (mostly benign in nature) originating from the arachnoendothelial tissue of the dura mater. The pathologic focus is more often formed on the cerebral surface, but sometimes found in other areas of the brain. In many cases, it is latent and may be an incidental finding during CT or MRI.
Under the influence of provoking factors, meningioma of the brain begins to grow expansively. A single nodular formation is formed, which gradually enlarges and presses on the surrounding structures, displacing them. Multicentric development of neoplasm from multiple foci is not excluded.
According to macroscopic characteristics, menigioma has a rounded configuration, sometimes horseshoe-shaped. The pathologic nodule is predominantly fused with the dural sheath, dense, and in many cases there is a capsule. The size of the formation varies - from a couple of millimeters to 1.5 or more decimeters. The color shade of the focal section is from grayish to grayish-yellowish. Cystic inclusions are usually absent.
Meningioma of the brain is more often benign in nature, growing slowly. But even in this case, the nidus can not always be removed qualitatively. It is not excluded and the occurrence of recurrences and malignancy of the tumor: in such a situation, the node accelerates its growth, sprouts into the surrounding tissues, including brain and bone structures. Against the background of malignization, metastases spread throughout the body.
Symptoms of the brain meningiomas
Meningioma of small size exists for a long time without any obvious manifestations. However, doctors note that even when symptoms appear, it is almost impossible to diagnose the tumor process based only on the patient's complaints: the clinical picture of pathology is nonspecific. Among the most common manifestations: prolonged pain in the head, general weakness, paralysis, visual impairment, speech disorders.
The specificity of symptoms depends on the location of the tumor focus.
- Frontal lobe meningioma is characterized by recurrent epileptic seizures, pain in the head, weakness in the arms and legs, difficulty speaking, and limited visual field.
- Frontal lobe meningioma is characterized by frequent epileptic seizures, weakness in the arms and legs, pain in the head, psycho-emotional disorders, deterioration of intellectual abilities, severe apathy, emotional instability, tremor, blunted affect.
- Meningioma of the cuneiform crest manifests itself with eye bulge, visual impairment, oculomotor paralysis, epileptic seizures, memory impairment, psycho-emotional disturbances, and head pain.
- Cerebellar meningioma often presents with erratic and uncoordinated movements, increased intracranial pressure, vocal and swallowing disorders.
- When meningioma is localized in the pontocerebellar angle, hearing loss, weakening of the facial musculature, dizziness, motor uncoordination and discoordination, increased intracranial pressure, vocal and swallowing disorders are noted.
- When the Turkish saddle and olfactory fossa are affected, anosmia, psycho-emotional disturbances, memory and visual function disorders, euphoric states, impaired concentration, and urinary incontinence are often found.
First signs
Against the background of the predominantly slow growth of the neoplasm, the initial symptoms are not detected immediately, but only when the surrounding structures are compressed directly by the tumor focus or swelling. The first symptoms are nonspecific. They may be:
- Head pain (dull, constant, pressing);
- Psycho-emotional instability, sudden mood swings;
- Behavioral disorders;
- Vestibular disorders, dizziness;
- Sudden deterioration of vision, hearing;
- Frequent nausea, independent of food intake.
After a while, the clinical picture expands. There are:
- Paresis and paralysis (unilateral);
- Speech dysfunction (difficulties with speech production, stuttering, etc.);
- Seizures;
- Mental impairment;
- Memory impairment;
- Coordination and orientation disorders.
Stages
Depending on the histologic picture, meningioma of the brain may have several stages or degrees of malignancy:
- Grade I includes benign, gradually developing tumors that do not grow into nearby tissues. Such meningiomas are characterized by a relatively favorable course and do not tend to recur. They occur in 80-90% of cases. Benign meningiomas are further classified depending on the cellular structure. Thus, neoplasms are meningothelial, fibrous, mixed, angiomatous, psammomatous, microcystic, secretory, luminal, metaplastic, chordoidal, imphoplasmocytic.
- Grade II includes atypical foci characterized by more aggressive development and a tendency to recurrence. In some cases, infiltrative growth into brain tissue is noted. Meningiomas of the second degree, in turn, are atypical, chordoidal and luminal. Such neoplasms occur in about 18% of cases.
- Grade III includes malignant meningiomas of three categories: papillary, anaplastic and rhabdoid. All of them are characterized by an aggressive course with infiltrative growth, metastasis and a high incidence of recurrence. However, such foci are relatively rare - about 2% of cases.
Forms
According to the local manifestations of meningioma of the brain can be divided into the following types:
- Falx meningioma is a nidus sprouting from the sickle process. The clinic is characterized by convulsive seizures (epileptic), possible paralysis of limbs and dysfunction of pelvic organs.
- Atypical meningioma corresponding to grade 2 malignancy. It is characterized by neurological symptoms and rapid growth.
- Anaplastic meningioma is a malignant pathologic nodule.
- Petrified neoplasm - manifested by a strong feeling of fatigue, weakness in the limbs, dizziness.
- Parasagittal neoplasm - accompanied by seizures, paresthesias, intracranial hypertension.
- Frontal lobe lesions are characterized by mental and emotional disorders, impaired concentration, hallucinations, depressive states.
- Convexital temporal zone tumor - manifested by auditory and speech disorders, tremor.
- Obstructed parietal meningioma - accompanied by the appearance of thought and orientation problems.
- Meningotheliomatous neoplasm - characterized by slow growth and the appearance of primary focal symptoms.
- Turkish saddle tubercle nodule is a benign focus that manifests with unilateral visual function impairment and chiasmal syndrome (optic atrophy and bitemporal hemianopsia).
Complications and consequences
The likelihood of adverse effects and complications of brain meningioma depends on many factors. In patients who have undergone surgical removal of the neoplasm, the chances of complete cure are much higher. But the refusal of surgery, if indicated, in most cases leads to an irreparable outcome: the patient's condition may steadily worsen until death.
The success of treatment is closely related to the quality of the surgical intervention and the postoperative rehabilitation period. The rate at which the patient returns to normal life is also influenced by:
- Absence of pathologies of the cardiovascular system;
- Absence of diabetes mellitus;
- Elimination of bad habits;
- Accurate fulfillment of the doctor's recommendations.
In some cases, even after surgical resection of the tumor focus, recurrences occur after some time:
- Meningiomas with atypical course recur in 40% of cases;
- Malignant meningiomas recur in almost 80% of cases.
Foci located in the region of the cuneiform bone, Turkish saddle and cavernous sinus are more prone to "return" of the tumor process after treatment. The recurrence of neoplasms formed in the cranial vault is much less frequent. [4]
Diagnostics of the brain meningiomas
Meningioma of the brain is detected mainly by diagnostic radiation techniques.
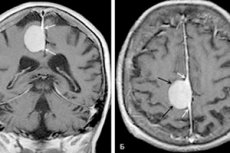
MRI - magnetic resonance imaging - helps to detect tumor process of any localization. In the course of diagnostics, the structure of the brain substance, the presence of pathological foci and zones with abnormal blood circulation, as well as vascular neoplasms, inflammatory and post-traumatic disorders of the brain membranes are primarily determined.
For differential diagnosis and assessment of the size of the pathologic nodule, MRI with injection of contrast enhancing agent is used. Meningiomas often have a so-called "dural tail", a linear area of contrast enhancement extending beyond the borders of the tumor base. The appearance of such a "tail" is not due to infiltration, but to reactive changes in the membranes located near the tumor.
CT - computed tomography - helps to find out whether the cranial bones are involved in the pathological process, whether there are calcifications or areas of internal hemorrhage, which is not always visible on MRI. If indicated, it is possible to use bolus contrast - intravenous injection of X-ray contrast enhancement with a special syringe.
Laboratory tests are mainly represented by such blood tests:
- General analysis - helps to assess the total number of platelets, red blood cells, white blood cells and other blood cells, which helps to identify an inflammatory or anemic process;
- Biochemical analysis - allows you to determine the chemical composition of the blood;
- Cancer marker study.
If necessary, additional instrumental diagnostics is prescribed:
- Electroencephalography (records brain activity);
- Angiography (reveals the intensity of blood supply to the tumor focus);
- Positron emission tomography (PET helps detect recurrences of neoplasm).
Differential diagnosis
During the differential diagnosis of brain tumor processes it is necessary to take into account various factors, including general diagnostic and epidemiological. Magnetic resonance imaging is considered to be the "number 1" study. In the course of diagnostic measures, it is absolutely necessary to take into account:
- Frequency of pathologies (1/3 - glial tumors, 1/3 - metastatic foci, 1/3 - other neoplasms);
- Age of the patient (children are more likely to have leukemias and lymphomas, anaplastic tumors and teratomas, as well as craniopharyngiomas, medulloblastomas and ependymomas; in adult patients, glioblastomas and astrocytomas, meningiomas and schwannomas are found predominantly; in elderly patients, meningiomas, glioblastomas and metastatic tumors are diagnosed more often);
- Localization (supratentorial, infratentorial, intraventricular, sellar-parasellar, cerebellopontine angle, etc.);
- Type of spread (along the spinal cord - oligodendroglioma, ependymoma, medulloblastoma, lymphoma; to the opposite hemisphere - glioblastoma, astrocytoma of low differentiation; with involvement of the cortex - oligodendroglioma, ganglioglioma);
- Features of the internal structure (calcification is more characteristic of oligodendroglioma and craniopharyngeoma, but also occurs in 20% of meningiomas);
- Diffusion (clear diffusion-weighted foci on MRI are typical of abscesses, epidermoid cystic masses, acute stroke; tumor processes have a low signal on diffusion-weighted MRI of the brain).
Who to contact?
Treatment of the brain meningiomas
The scheme of therapy for brain meningioma is prescribed according to an individual program, taking into account the size and location of the neoplasm, existing symptoms, intensity of growth, age of the patient. Most often, doctors turn to one of the three main techniques: observation tactics, surgical resection and radiation therapy.
Observational tactics are applied to meningiomas that grow slowly, no more than 1-2 mm per year. Patients with such neoplasms should undergo annual diagnostic magnetic resonance imaging:
- If it is a small node, with no or mild symptoms and preserved quality of life;
- If the pathology is detected in an elderly person against the background of slowly progressive symptoms.
Surgical treatment is considered the mainstay of meningioma removal. Surgery is mandatory if the nidus is located in an accessible location away from functionally significant areas of the brain. If possible, the surgeon will try to completely remove the neoplasm to prevent recurrence in the future, and at the same time restore (preserve) the functionality of the nervous system. Unfortunately, this possibility is not always present. For example, if the focus is located at the base of the skull, or grows into the venous sinuses, then complete resection is canceled because of the high probability of serious complications. In such a situation, the surgeon performs a partial excision to reduce compression of brain structures. Then patients are obligatorily treated with radiosurgery and radiation therapy.
Gamma Knife radiosurgery is indicated for all patients with primary meningioma, regardless of the location of the pathological node, as well as for patients with residual tumors after incomplete resection or irradiation (if the maximum size of the focus does not exceed 30 mm). Gamma knife is more suitable for impact on formations with their location in deep brain structures, difficult to access for conventional surgical intervention. The method is also applied to patients who are unable to tolerate conventional surgery. Radiosurgery stops the growth of meningioma by destroying its DNA and thrombizing the feeding vascular network. This treatment is effective in more than 90% of cases.
"Pros" of Gamma Knife treatment:
- The surrounding brain structures aren't affected;
- There is no need for the patient to be hospitalized;
- The method is non-invasive, so there is no risk of infection or blood loss;
- There is no need for general anesthesia;
- There is no need for a long recovery period.
Conventional radiation therapy is indicated for patients with multiple or large meningiomas and involves the use of ionizing radiation. Depending on the indication, a distinction is made between X-ray therapy, β-therapy, γ-therapy, proton and neutron exposure. The therapeutic efficacy is based on the damage of tumor DNA of actively proliferating cells, which entails their death.
Chemotherapy for benign meningioma of the brain is inappropriate and is practically not used. However, this method is prescribed in malignant neoplasms as an auxiliary effect to slow growth and prevent the spread of the pathological process to deep brain tissue.
Additionally prescribe symptomatic therapy, to relieve the patient's condition and improve blood circulation in the brain.
Medications
As a preoperative preparation, patients with cerebral meningioma are administered drugs to stabilize blood pressure. If there are no hypothalamic-pituitary crises, Proroxan 0.015-0.03 g three times a day or Butyroxan 0.01-0.02 g three times a day are administered against the background of blood pressure monitoring (it is important to monitor the patient's condition, as a sharp drop in BP, bradycardia, fainting, heart rhythm disturbances are possible). If persistently elevated BP, Prazosin 0.5-1 mg three times a day is recommended. It is a synthetic vasodilator, and possible side effects include dyspnea, orthostatic BP lowering, leg swelling.
Taking into account the degree of adrenal insufficiency, hormone replacement therapy with Cortisone, Hydrocortisone, Prednisolone is performed. Before surgery, patients are administered Hydrocortisone 50 mg every 8 hours (also administered immediately before the intervention, during its process and for several days after, in individual doses).
If indicated, thyroid hormones and sex hormones are used. For the purpose of prophylaxis a day before the intervention, therapy with cephalosporins is started. Traditionally, it is Ceftriaxone 1-2 g up to two times a day intramuscularly, with continued treatment for five days after surgery. In the development of inflammatory processes (meningoencephalitis), antibiotic therapy is prescribed taking into account the identified pathogen, for two weeks, and patients with immunodeficiency states - for 3 or more weeks. Parenteral administration of penicillins, fluoroquinolones, III generation cephalosporins, glycopeptides is possible.
What vitamins cannot be taken with meningioma of the brain?
The daily intake of vitamins in the body of cancer patients is especially important. For people weakened by tumor processes, useful substances are vital, and they should be supplied not only with food, but often in the form of special medicines - tablets or injections. The decision on the need for additional introduction of vitamins is made by the attending doctor. In most cases, vitamin therapy is indicated to increase the body's defenses, activate recovery processes, strengthen immunity, weakened by radiation or surgery. In addition, vitamins often reduce the side effects of drug therapy.
Most vitamin preparations have only a positive effect on the body - provided that the prescribed dosage is followed. However, some vitamins doctors advise caution and should not be taken without the prescription of a doctor. We are talking about such drugs:
- Alpha-tocopherol (vitamin E);
- Methylcobalamin (vitamin B12);
- Thiamine (B1);
- Folic acid (B9).
Requires caution when taking vitamins A and D3, as well as multivitamin preparations containing iron.
Rehabilitation
Surgical resection of meningioma of the brain is a rather serious operation. Even if the intervention is perfectly performed, it is very important to conduct the rehabilitation period correctly to ensure a full recovery without the risk of tumor reoccurrence.
There are a number of prohibitions to keep in mind after surgery:
- You can't drink alcoholic beverages;
- You cannot travel by air (unless your doctor approves);
- Do not go to sauna and sauna, use a solarium, sunbathe during the period of active sun;
- For the first time, you should not engage in active sports involving increased stress;
- You should avoid scandals, quarrels and other situations that can negatively affect the central nervous system and blood pressure.
The rehabilitation program is developed individually for each patient. During the recovery process, the scheme may change, depending on the existing dynamics. In case of edema and residual pain syndrome, physiotherapy may be used. In paresis of the limbs, to improve blood circulation and lymph flow, increase neuromuscular conduction and sensitivity, massages and manual therapy are prescribed. Therapeutic exercise helps to restore lost functions, form reflex connections, stabilize the work of the vestibular apparatus.
Prevention
According to experts, many cancer pathologies have a connection with human nutrition. For example, preference for red meat is associated with various types of cancer. Alcoholic beverages, smoking, consumption of low-quality and unnatural food also have a negative impact.
Doctors recommend:
- Keep a balance between caloric intake and physical activity;
- To maintain normal body weight;
- To be physically active;
- In the diet to give preference to fruits, vegetables, greens, avoid convenience foods and red meat;
- Limit alcohol consumption.
Sufficient and adequate night rest is also important to strengthen the body in its ability to resist the development of oncology. Quality sleep contributes to the normalization of hormonal state, stabilization of the main vital processes. At the same time, lack of sleep leads to increased stress levels, disruption of healthy rhythms, which can give rise to the development of brain meningioma.
For preventive purposes, it is strongly recommended not to forget to undergo regular examinations, visit doctors in a timely manner.
Forecast
If benign meningioma of the brain is detected in time without sprouting into nearby tissues, the prognosis can be considered favorable. Most patients recover completely. In about 3% of cases, there is a recurrence of pathology. Atypical tumors are prone to recurrence in almost 40% of patients, and malignant tumors - in 75-80% of patients.
Specialists distinguish a five-year criterion for meningioma re-growth, which depends on the area of localization of the pathological focus. The least tendency to recurrence have neoplasms located near the cranial vault. Somewhat more often recurring tumors in the area of the Turkish saddle, even more often - lesions near the body of the cuneiform bone (within five years, 34% of such meningiomas grow again). Foci localized near the wings of the cuneiform bone and cavernous sinus are most prone to recurrence (60-99%).
The outcome of the disease directly depends on a responsible attitude to their own health and timely referral to doctors.
Alcohol for meningioma of the brain
Regardless of the location of brain meningioma, alcoholic beverages should be forgotten by all patients diagnosed with this disease. Alcoholic beverages should not be combined with any cancer, including benign ones. Alcohol is also contraindicated in patients who undergo chemotherapy. Even a small amount of alcoholic beverage can cause serious consequences, up to the death of the patient.
The reasons for this prohibition are as follows:
- Immune defense suffers, there are favorable conditions for the development of fungal, microbial or viral infection;
- The body carries an additional load and spends energy on eliminating alcohol intoxication, instead of directing them to fight the tumor process;
- The side effects of the chemo drugs are amplified;
- The liver and kidneys are subjected to increased strain and the risk of liver and kidney failure increases;
- Increased risk of metastasis;
- Significantly worsens the patient's well-being, worsening symptoms.
In some cases, alcohol can offset the effects previously achieved during chemotherapy, so it is important for meningioma patients to avoid alcohol completely.
Disability
Whether a disability can be awarded depends on a number of factors:
- Malignancy or benignity of the neoplasm;
- The possibility, fact and quality (completeness) of the surgical intervention;
- If there's been a recurrence;
- The nature and degree of functional disorders, the presence of disability;
- From social criteria such as age, occupation.
The first disability group is assigned if the patient has stable or increasing brain disorders, limitations in terms of self-care, movement, etc.
The second group is indicated for persons operated on for benign, malignant or metastatic tumor with unfavorable rehabilitation prognosis or with moderate but permanent disability.
The third group is assigned to patients with moderate impairment of brain function, which prevents adequate orientation, cognitive abilities, mobility, and labor activity.
If meningioma of the brain does not have pronounced symptoms, the patient's ability to work after treatment is preserved, then the granting of a disability group is not possible.

