Medical expert of the article
New publications
Liver atrophy
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Such a pathological condition as liver atrophy (from Greek trophe - nutrition with the negative prefix a-) means a decrease in the functional mass of the liver - a reduction in the number of cells capable of ensuring the full function of this organ. [1]
Epidemiology
While chronic hepatitis affects almost 1% of adult Europeans, liver cirrhosis - 2-3%, and fatty liver disease is found in 25% of the world's population, even approximate statistics of cases of liver atrophy are not given in scientific literature. At the same time, the number of cases of all chronic liver diseases on a global scale is estimated at 1.5 billion per year.
Causes of the liver atrophy
Etiologically, liver atrophy has been associated with many diseases and pathologies, including:
- Chronic hepatitis (viral, cholestatic, autoimmune, drug-induced, etc.);
- Liver cirrhosis (primary and secondary biliary, cytomegalovirus, alcoholic, toxic);
- Parasitic infestations of the liver, such as liver echinococcosis, opistorchiasis or schistosomiasis;
- Primary liver cancer as well as metastatic carcinoma;
- Liver damage by toxic substances (heavy metals, arsenic, phosphorus, etc.) - with the development of intoxication syndrome hepatotropic character;
- Hepatolenticular degeneration (hepatocerebral dystrophy) or hereditary copper intoxication - wilson-Conovalov disease;
- Hereditary excess iron in the liver - hemochromatosis;
- Liver granuloma - of infectious origin, drug-related (associated with the use of antineoplastic drugs) or due to systemic sarcoidosis;
- Inflammation and intrahepatic bile duct obstruction in chronic cholangitis;
- Idiopathic portal hypertension.
Often the causes of atrophic changes in the liver lie in hepatic veno-occlusive disease - blockage of the central veins of the hepatic lobules and their sinusoidal capillaries or obliterative thrombophlebitis of hepatic veins - budd-Chiari syndrome. In both cases, there is atrophy of the liver with congestive hyperemia (passive venous stasis) - an increased amount of blood in the peripheral vessels of the liver.
In addition, atrophy may result from progressive liver dystrophy.
Risk factors
Hepatologists consider the main risk factors for the development of atrophic processes in the liver to be: alcohol abuse (more than 90% of heavy drinkers develop liver obesity), type 2 diabetes (insulin resistance), obesity and overnutrition, viral infections and parasite infestation, biliary tract obstruction (after cholecystectomy and in bile duct carcinoma), tuberculosis, amyloidosis, genetically determined cystic fibrosis (cystic fibrosis), congenital anomalies of hepatic veins, portal circulation disorders (blood circulation in the portal vein and hepatic artery system), autoimmune and metabolic diseases (e.g., glycogen storage diseases), exposure to ionizing radiation, bone marrow transplantation, and acute conditions such as disseminated intravascular coagulation syndrome (DIC) and hELLP syndrome in late pregnancy.
Also see:
Pathogenesis
In different etiologies of atrophy, the mechanism of its development may not be the same, but the common feature is that in all cases hepatocytes - the main parenchymatous cells of the liver - are damaged.
Emerging as a consequence of chronic hepatic alteration and inflammation, cirrhosis causes a fibrogenic response to damage - formation of scar tissue, i.e. Diffuse liver fibrosis, which is initiated by hepatic stellate cells. In fibrosis the morphology of the tissue changes with the appearance of protein contractile fibers, increased proliferation in the areas of greatest damage and replacement of normal liver structures by regenerative micro- and macro nodules.
Fibrotic degeneration of hepatic parenchyma is also due to the pathogenesis of its atrophy in parasite infestation (fibrosis is subjected to the tissues surrounding the parasitic cyst), Wilson-Conovalov disease or hemochromatosis.
In acute venous hyperemia, blood functions and blood flow in the liver are disturbed; ischemic damage to hepatocytes occurs - with the development of acute centrilobular or central liver necrosis (hypoxic hepatopathy, which is called shock liver). In addition, sinusoidal capillaries overfilled with blood squeeze the liver tissue, and degenerative and necrotic processes occur in hepatic lobules.
Blood stasis impedes the outflow of lymph, and this leads to the accumulation of fluid that contains products of tissue metabolism, as well as increased oxygen starvation of hepatocytes.
In fatty liver disease, transport of fatty acids from adipose tissue to the liver is increased - with triglycerides deposited in the cytoplasm of hepatocytes, which undergo microvesicular and then macrovesicular fatty changes, often accompanied by inflammation (steatohepatitis). [2]
The mechanism of the damaging effect of ethanol on hepatocytes is discussed in detail in the publication - alcoholic Liver Disease.
Symptoms of the liver atrophy
Atrophy of part of the liver (lobular or segmental) or at the initial stage of structural disorders, the first signs are manifested by general weakness and daytime sleepiness, a feeling of heaviness and dull pain in the right side, icteric (jaundice of the skin and eyeballs), nausea and vomiting, GI motility disorders, decreased diuresis.
The more extensive the area of atrophic hepatocyte damage, the more severe its symptoms (in various combinations), including: ascites (fluid accumulation in the abdominal cavity); tremors and seizures; enlargement of the liver and spleen; dyspnea and heart rhythm disturbances; multiple subcutaneous hemorrhages; progressive confusion; and personality and behavioral disorders. That is, symptoms develop acute liver failure.
Distinguish such types of atrophic changes in the liver as:
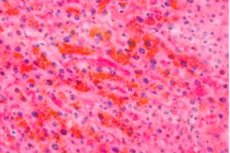
- Brown atrophy of the liver, which usually develops in extreme exhaustion (cachexia) and in the elderly and is associated with a decrease in the intensity of metabolic processes and oxidative stress (damage to hepatocytes by free radicals). And brown color of hepatic tissue, in which the number of functionally complete cells decreases, is given by intracellular deposition of lipoprotein pigment lipofuscin;
- Yellow liver atrophy or yellow acute liver atrophy - with shriveling of the liver and softening of the parenchyma - is rapid extensive liver cell death caused by viral hepatitis, toxic substances, or hepatotoxic medications. This atrophy may be defined as transient or fulminant hepatitis; [3]
- Fatty liver atrophy, fatty liver dystrophy, fatty liver disease, fatty liver degeneration, fatty hepatosis, focal or diffuse hepatosteatosis or liver steatosis (simple - in obesity or type 2 diabetes, and also associated with alcoholic liver disease) may be virtually asymptomatic or manifest with generalized weakness and pain in the upper right abdomen;
- Muscat liver atrophy is the result of chronic venous hemorrhage in the liver or obliterative thrombophlebitis of the hepatic veins (Budd-Chiari syndrome); due to proliferation of connective tissue cells, the liver tissue is thickened, and the presence of dark red and yellow-gray areas on a slice resembles the kernel of a nutmeg. In this condition, patients complain of right subcostal pain, skin itching, and swelling and cramping of the lower extremities.
Complications and consequences
Due to atrophy of hepatocytes and parenchymatous cells liver functions - bile formation; detoxification of blood and maintenance of its chemical composition; metabolism of proteins, amino acids, carbohydrates, fats and trace elements; synthesis of many blood clotting factors and innate immunity proteins; insulin metabolism and catabolism of hormones - are impaired.
Complications and consequences of liver atrophy are manifested by alteration of the hepatobiliary system in the form of acute liver failure, postnecrotic cirrhosis, hepatic encephalopathy (when the level of unconjugated bilirubin in the serum rises, it diffuses into the CNS), toxic liver and kidney damage - hepatorenal syndrome, esophageal varices, as well as autointoxication and hepatic coma. [4]
Diagnostics of the liver atrophy
In diagnosis, both physical methods of liver research, and laboratory studies - tests are used: a detailed biochemical blood test, for hepatitis virus, coagulogram, blood tests for liver tests, for the level of total bilirubin, albumin, total protein and alpha1-antitrypsin, immunologic blood tests (for the level of B- and T-lymphocytes, immunoglobulins, anti-HCV-antibodies); general urinalysis. Puncture liver biopsy may be required.
Instrumental diagnostics are performed for visualization: X-ray, ultrasound or CT of the liver and biliary tract; radioisotope hepatography, elastometry (fibroscanning) of the liver, color Doppler echography, angiography of the liver (venohepatography), X-ray of the biliary tract with contrast agent.
Differential diagnosis
Differential diagnosis should exclude hepatic hypoplasia and hemangioma, abscess, neoplasms and liver metastases.
Treatment of the liver atrophy
Liver atrophy is a terminal condition and its treatment to reduce the degree of liver failure may require resuscitative measures to allow other systems and oganes to function.
Severe jaundice and intoxication of the body requires intravenous detoxification therapy using plasmapheresis and hemosorption. Peritoneal dialysis and blood transfusion are also used.
The same principles of intensive care for hepatic coma.
When part of the liver is affected, it is used:
- Drugs to treat and restore the liver
- Liver cleansing drugs (hepatotropic agents)
- Names and ratings of liver medications
In cases of atrophy of half of the liver, a partial hepatectomy (excision of the affected tissue) may be performed, and if the entire organ is affected and acute liver failure cannot be treated, liver transplantation may be required. [5]
Prevention
At the heart of the prevention of liver atrophy is the refusal of alcohol and treatment of liver diseases and all pathologies that in one way or another lead to its atrophic lesion.
Forecast
In liver atrophy, the prognosis depends on its etiology, the functional state of the liver, the stage of the disease and the presence of complications. And if at the initial stage the loss of liver cell mass can be compensated, the terminal stage in 85% of cases leads to death.

