Medical expert of the article
New publications
Erythrocytes in the urine of a child: what does it mean?
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
When passing a general urine test, among the many components determined in the course of its biochemical and microscopic examination, blood components can be detected - red blood cells in the urine of a child.
What does it mean and what kidney or urinary tract problems might it indicate?
Elevated red blood cells in a child's urine
Depending on the number of red blood cells in the urine, nephrology defines erythrocyturia and microhematuria - when the content of red blood cells does not change the color of the urine. Also distinguished hematuria (glomerular or non-glomerular macrohematuria), in which the impurity of blood affects the color of the urine. Read more - urine is red in a child. [1]
Trace, conditionally acceptable number of red blood cells - the norm of red blood cells in the urine of a child is no more than 1-2/HPF (that is, in the visualization field of the microscope).
In diagnostic terms, more accurate is considered a urine analysis according to Nechiporenko, in which the number of all red blood cells in a urine sample of 1 ml is counted.
Erythrocytes in the urine according to Nechiporenko in a child are elevated if there are more than one thousand in 1 ml. It should be borne in mind that nechiporenko test is appointed when diagnosing nephrologic inflammatory diseases, as well as pathologies of systemic nature, which can affect kidney function. Most often this study is necessary if, against the background of the absence of other symptoms for several days, there is an elevated (> +38.3 ° C) temperature and erythrocytes in the urine of the child, detected when taking a general analysis.
If the urine specimen has been obtained correctly, it provides sufficient information and the results should be interpreted according to the age of the patients. Erythrocyturia may have a tubular or postglomerular etiology, but in children - more often than in adults - the cause of erythrocytes in the urine is the tubules of the renal nephrons rather than the urinary tract. Through damage to the capillary walls, erythrocytes can penetrate the lumen of the capillary network of the renal parenchyma and cross the endothelial barrier of the nephrons.
Temporarily elevated erythrocytes in the urine of a child may be detected during systemic infections, during febrile conditions, or after physical exertion, which is considered a renal hemodynamic response whose mechanisms are still unknown.
The degree of microhematuria may vary: at 10-15/HPF (according to others, more than 5-10) - insignificant; at 20-35/HPF - moderate; at 40/HPF and more - significant.
When conducting a urine analysis by Nechiporenko also determine the degree of hematuria: up to 10x10³ erythrocytes / ml (> 1000 erythrocytes / ml) - minimal, within 60x10³ / ml - moderate, and everything above - pronounced.
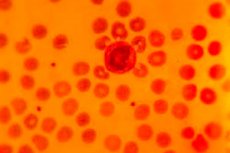
For diagnosis, phase-contrast microscopy of the urine sediment is performed, since eumorphic, that is, unchanged erythrocytes in the urine of a child are often detected simultaneously with white blood cells - leukocytes, which nephrologists associate with nephrolithiasis (renal nodules) and damage to the tissues of the organ of various etiologies.
In addition, the analysis may show dysmorphic erythrocytes, that is, altered red blood cells in the child's urine: smaller, spherical, oval or spike-shaped, which indicates the presence of abnormalities of the renal tubules (glomeruli), including congenital.
In chronic glomerulonephritis in children microhematuria is determined and partially hemolyzed (hemoglobin-free) - leached red blood cells are detected in the child's urine. [2]
The same analysis is characterized by nephrotic syndrome in children, acute glomerular inflammatory process, as well as intoxications in which protein also appears in the urine. [3]
Causes of the red blood cells in a baby's urine.
The most likely causes of an elevated red blood cell count in a child's urine include:
- Traumatic injury to the kidney;
- Certain drugs (aspirin and other NSAIDs, sulfonamides, anticoagulants) and toxins (lead, tin compounds, phenols, carbon monoxide);
- Kidney prolapse or nephroptosis; [4]
- Renal vein thrombosis;
- Congenital anomalies of the urinary tract leading to hydronephrosis;
- Vesicoureteral reflux in children with risk of nephrosclerosis outcomes;
- Inflammation of renal tissue of non-bacterial origin or interstitial nephritis;
- Chronic glomerulonephritis in children;
- Nephrocalcinosis (calcium oxalate deposits in the kidneys);
- IgA nephropathy, also known as IgA nephritis or Berger's disease;
- Nephroblastoma - wilms tumor;
- Sickle cell anemia.
Many red blood cells are found in a child's urine in a congenital abnormality of the basal membrane of the renal tubules - hereditary nephritis (Alport syndrome) in children, as well as in the presence of renal cysts, such as medullary cystic disease - Fanconi's nephronophthisis. [5]
Erythrocytes and leukocytes in a child's urine
Often, red blood cells and white blood cells can be detected in a child's urine at the same time. The number of white blood cells may increase in response to intense physical exertion, seizures, acute emotional reactions, pain, infections and intoxication.
Leukocytes are protective cells of the body, and their appearance in the urine in the amount of more than 5-10/HPF or above 2000 in 1 ml (according to Nechiporenko) is defined as leukocyturia or pyuria.
In children, an increase in white blood cells is a sign of urinary tract infections (cystitis) with corresponding symptoms or a systemic inflammatory reaction.
In addition, leukocyturia is manifested by:
- Inflammation of the kidneys caused by bacterial infection - pyelonephritis, including purulent;
- Acute poststreptococcal glomerulonephritis in children;
- Uroi nephrolithiasis (stones in the bladder and/or kidneys).
Protein and red blood cells in a child's urine
Usually in normal urine, especially after exercise, protein food is found a small trace amount of proteins (filtered by the tubules and produced by the cells of the tubules of the nephrons) - up to 0.08-0.2 g / day: according to other data - up to 0.035 g / L or up to 10 mg/100 ml per day.
And if the analysis showed increased protein and erythrocytes in the child's urine, then proteinuria combined with erythrocyturia (or hematuria) makes doctors suspect cystitis, urethritis, glomerulonephritis (or glomerulopathy), tuberculosis or renal neoplasm, requiring further examination of the patient. [6]
When signs of mild proteinuria persist (<1 g/m2/day) or the albumin/creatinine ratio exceeds 2 mg/mg (except in cases of orthostatic proteinuria), the most likely provisional diagnosis is still glomerulonephritis or tubulointerstitial nephropathies. [7]
As noted by nephrologists, with moderately elevated protein in the urine (up to 1-3 g / day) is possible as pyelonephritis or the presence of cystic formations in renal tissue, and their amyloid degeneration, the development of which may be associated with frequent pneumonia in the child, rheumatoid arthritis, bone inflammation (osteomyelitis), Hodgkin's lymphoma, etc.
Severe proteinuria (above 3 g per day) often reflects the presence of congenital nephrotic syndrome in children infants and up to 8-10 years of age.
Differential diagnosis
Urinalysis findings such as erythrocyturia/hematuria, leukocyturia, and proteinuria may be isolated, but a combination is more commonly noted. Hematuria can occur in the tubules, renal tubules, renal interstitium or urinary tract, including the ureter, bladder or urethra.
The results should therefore be interpreted on the basis of history, symptoms and physical examination. However, children with significant proteinuria (> 500 mg/24 hours) require immediate referral to a nephrologist, and if the child has erythrocytes and leukocytes in the urine, they should undergo a stepwise evaluation to determine a differential diagnosis.
The differential diagnosis takes into account the possibility of focal segmental or progressive membranoproliferative glomerulonephritis, immune disorders, and connective tissue diseases, particularly secondary glomerulonephritis in systemic lupus erythematosus or hemorrhagic vasculitis in children (formerly known as Henoch-Schenlein purpura). [8]
For this purpose, additional tests are performed, including general blood tests, for C-reactive protein, creatinine, cystatin C, electrolytes, IgA levels, cytoplasmic antibodies (p-/c-ANCA) and complement C3 in the blood, etc.
Cystourethrography (especially in patients with urinary tract infections); ultrasound (USG), CT or MRI of the kidneys, bladder and urinary tract; dynamic renal scintigraphy, urinary cystourethrogram, etc. Are needed.
More information in the material - kidney study
Treatment of the red blood cells in a baby's urine.
Microhematuria - red blood cells in a child's urine - is a common condition of concern for parents, and for good reason, as most cases of microhematuria point to medical conditions that usually require referral to a pediatric nephrologist. Indications requiring referral to a urologist are less common but include stone obstruction, kidney damage due to trauma, and anatomical abnormalities.
It is easiest to treat urinary tract infections in children, and the main drugs prescribed for cystitis or urethritis are antibiotics: Amoxicillin, Amoxiclav (Amoxicillin with clavulanic acid), Doxycycline (used only from the age of 8 years), drugs of the group of cephalosporins, as well as Nitrofurantoin (Furadonin) and others.
Dosages, side effects and all necessary information with material - how urinary tract infections are treated and review - antibiotics for cystitis.
Children with vesicoureteral reflux have an increased risk of kidney infection with kidney damage, which can lead to chronic kidney failure in children. In severe cases of urinary reflux, there is a surgical option to address the problem, but children with mild to moderate vesicoureteral reflux are more likely to outgrow the condition. See - treatment of vesicoureteral reflux
However, the prognosis for developing kidney disease or kidney failure in adulthood is estimated to be 40-50%.
Also, more useful information can be found in publications:
Использованная литература

