Medical expert of the article
New publications
Acute and chronic nephrotic syndrome
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
If the patient's kidneys are affected and edema appears, and diagnostics determine the presence of proteinuria, electrolyte, protein and fat metabolism disorders, then the doctor can diagnose "nephrotic syndrome" - this term has been used in medicine for about 70 years. Previously, the disease was called nephrosis or lipoid nephrosis.
Nephrotic syndrome often develops as a result of inflammatory processes in the kidneys, as well as against the background of other complex pathologies, including those of an autoimmune nature.
Definition of Nephrotic Syndrome: What is it?
The disease we are considering is a complex of symptoms, a pathological condition in which there is a significant daily excretion of protein with urine (more than 3.5 g/1.73 m²). The pathology is also characterized by hypoalbuminuria, lipiduria, hyperlipidemia, and edema.
In healthy people, the daily physiological excretion of protein through the kidneys is less than 150 mg (usually about 50 mg). Such proteins are represented by plasma albumins, enzyme and hormonal substances, immunoglobulins, and renal glycoprotein.
In nephrotic pathology, such disorders as hypoalbuminuria, dysproteinemia, hyperlipidemia, lipiduria, as well as pronounced edema on the face, in cavities and throughout the body are detected.
Nephrotic syndrome is divided into primary and secondary types, depending on the etiology of the disease. The primary type is spoken of if it develops against the background of other kidney diseases. The secondary type is diagnosed somewhat less frequently: its development is associated with the "intervention" of other diseases (collagenoses, rheumatism, hemorrhagic vasculitis, chronic purulent-inflammatory processes, infections, tumors, allergies, etc.).
Causes nephrotic syndrome
The causes of nephrotic syndrome are varied, but most often the disease develops as a consequence of glomerulonephritis - either acute or chronic. Statistics indicate that with glomerulonephritis, complications occur in approximately 75% of cases.
Other common factors include:
- primary amyloidosis;
- hypernephroma;
- nephropathy in pregnancy.
Secondary nephrotic syndrome develops against the background of:
- diabetes mellitus;
- infectious pathologies (such as malaria, syphilis, tuberculosis);
- autoimmune diseases (systemic lupus erythematosus, systemic scleroderma, rheumatoid arthritis);
- allergic processes;
- periarteritis;
- septic endocarditis;
- hemorrhagic vasculitis;
- lymphogranulomatosis;
- severe intoxication;
- malignant processes;
- thrombotic complications affecting the renal veins, inferior vena cava;
- frequent and long courses of treatment with various medications, including chemotherapy.
This type of development of nephrotic disease, the cause of which cannot be determined, is called idiopathic. It occurs mainly in children.
Risk factors
The development of nephrotic syndrome can be triggered by the following risk factors:
- long-term or regular treatment with non-steroidal anti-inflammatory drugs (acetylsalicylic acid, voltaren);
- frequent and prolonged antibiotic therapy;
- infectious diseases (tuberculosis, syphilis, malaria, hepatitis B and C, human immunodeficiency virus);
- allergic processes;
- autoimmune processes;
- endocrine diseases (thyroid disease, diabetes, etc.).
Pathogenesis
Today, there are a number of theories that presumably explain the development of the nephrotic symptom complex. The immunological concept of the disease is considered the most plausible. Its evidence is the frequent development of pathology in people with allergic and autoimmune processes in their bodies. This theory is also confirmed by the high percentage of successful treatment with the use of immunosuppressants. During the development of nephrotic syndrome, immune complexes are formed in the blood, which are a consequence of the relationship between internal and external antigens and antibodies.
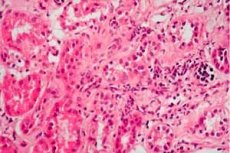
The formed immune complexes are able to settle inside the kidneys, which causes a response inflammatory process. Microcirculation disorders occur in the capillary network of the glomeruli, and coagulation inside the vessels increases.
Glomerular filtration is impaired due to changes in permeability. As a result, protein metabolism processes are impaired: protein enters the urine and leaves the body. Increased protein excretion causes hypoproteinemia, hyperlipidemia, etc.
With nephrotic syndrome, the appearance of the organ also changes: the kidney increases in volume, the medulla changes color and becomes reddish, and the cortex becomes grayish.
Pathophysiology
The excretion of protein with urine occurs as a result of disturbances affecting the endothelial cells of the capillary network, the glomerular basement membrane - that is, structures that normally filter plasma protein selectively, strictly according to a certain volume and mass.
The process of damage to the listed structures is poorly understood in primary glomerular lesions. Presumably, T-lymphocytes begin to secrete excessively the circulating permeability factor, or suppress the production of the inhibitory permeability factor, responding to the appearance of undefined immunogens and cytokines. Among other probable factors, hereditary anomalies of proteins that make up the slit glomerular diaphragm cannot be ruled out.
Symptoms nephrotic syndrome
Clinical manifestations largely depend on the underlying cause of the pathology.
The first main signs are edema, increasing anemia, general deterioration of health, and impaired diuresis towards oliguria.
The general picture of nephrotic syndrome is represented by the following symptoms:
- cloudy urine, a sharp decrease in its daily volume;
- varying degrees of swelling, from moderate to very strong;
- loss of strength, increasing feeling of fatigue;
- loss of appetite, thirst, dry skin and mucous membranes;
- rarely (for example, in the presence of ascites) – nausea, diarrhea, abdominal discomfort;
- frequent pain in the head, in the lower back;
- muscle cramps and pain (with prolonged course of nephrotic syndrome);
- dyspnea (due to ascites and/or hydropericarditis);
- apathy, lack of mobility;
- pale skin, deterioration of the condition of the skin, nails, hair;
- increased heart rate;
- the appearance of a thick coating on the surface of the tongue, an increase in the size of the abdomen;
- signs of increased blood coagulation.
Nephrotic syndrome can develop at different rates - both gradually and rapidly. In addition, a distinction is made between pure and mixed course of the disease. The difference lies in the additional presence of high blood pressure and hematuria.
- Edema in nephrotic syndrome can be expressed in different ways, but it is always present. Initially, fluid accumulates in the tissues of the face - under the eyes, on the cheeks, in the forehead and lower jaw. This symptom is called "nephrotic face". Over time, the accumulation of fluid spreads to other tissues - swelling of the extremities, lower back is observed, ascites, hydropericardium, hydrothorax develop. In severe cases, anasarca develops - swelling of the body as a whole.
The mechanism of edema in nephrotic syndrome can be different. For example, edema is often provoked by an increased content of sodium chloride in the bloodstream. With an excess volume of fluid in the body, moisture begins to penetrate through the vascular wall into adjacent tissues. In addition, nephrotic syndrome is accompanied by an increased loss of albumin with urine, which leads to an imbalance in oncotic pressure. As a result, moisture comes out into the tissues with additional force.
- Oliguria in nephrotic syndrome is dangerous because it can provoke the development of such a complication as renal failure. In patients, the daily urine volume can be 700-800 ml or even less. At the same time, it contains significantly more protein, lipids, pathogenic microorganisms, and sometimes blood is present (for example, in glomerulonephritis and systemic lupus erythematosus).
- Ascites in nephrotic syndrome is observed against the background of a severe course of pathology. Fluid accumulates not only in tissues, but also in body cavities - in particular, in the abdominal cavity. The simultaneous formation of ascites with the accumulation of moisture in the pericardial and pleural cavities indicates the imminent appearance of diffuse (widespread) edema of the body. In such a situation, they talk about the development of general dropsy, or anasarca.
- Arterial hypertension in nephrotic syndrome is not a basic or mandatory symptom. Blood pressure indicators may increase in the case of a mixed course of nephrotic syndrome - for example, in glomerulonephritis or systemic diseases.
Nephrotic syndrome in adults
Adults suffer from nephrotic syndrome mainly at the age of 30-40 years. The pathology is most often noted as a consequence of previous glomerulonephritis, pyelonephritis, primary amyloidosis, hypernephroma or nephropathy during pregnancy.
Secondary nephrotic syndrome is not directly related to kidney damage and occurs under the influence of collagenoses, rheumatic pathologies, purulent processes in the body, infectious and parasitic diseases.
Nephrotic syndrome develops with approximately the same frequency in women and men. In most cases, the disease manifests itself according to one "scenario", with the leading symptom being proteinuria over 3.0 g/day, sometimes reaching 10-15 g or even more. Up to 85% of the protein excreted in urine is albumin.
Hypercholesterolemia can also reach a maximum level of 26 mmol/liter or more. However, medicine also describes cases where cholesterol levels were within the upper normal limits.
As for swelling, this symptom is considered to be quite specific, as it is found in most patients.
Nephrotic syndrome in children
Nephrotic syndrome in the overwhelming majority of children is idiopathic. The pathogenesis of this disease state, which occurs with minimal disturbances, has not yet been fully studied. Presumably, there is an increase in glomerular permeability for plasma protein due to the influence of circulatory factors on the capillary network of glomeruli, with subsequent damage to the diaphragms between the processes of podocytes. Probably, active T-killers secrete lymphokines that affect the penetrating ability of glomeruli in relation to plasma proteins, which leads to proteinuria.
The first clinical signs in children are swelling, which can occur gradually or intensively, affecting more and more tissue.
The prognosis of nephrotic syndrome in childhood depends on the response to treatment with glucocorticosteroids and immunosuppressants. In steroid-sensitive nephrotic syndrome, remission is achieved in 95% of cases, without deterioration of renal function.
The steroid-resistant variant can progress to the terminal stage of chronic renal failure (within 5-10 years).
Stages
- Acute nephrotic syndrome is characterized by swelling, which occurs in the face in the morning and "falls" to the lower extremities in the evening. Clouding and a decrease in the amount of urine are also observed. Patients complain of weakness, apathy, headaches. If the symptoms do not appear sharply, but increase gradually, they speak of a subacute course of the disease.
- Chronic nephrotic syndrome is diagnosed when the main signs of the pathology appear and then disappear (usually with different time intervals - that is, an exacerbation can happen once every few months, or after six months). The clinical picture of the exacerbation period resembles the symptoms of acute nephrotic syndrome. With regular repetitions, they talk about the transition of the disease to a chronic relapsing form.
Forms
Nephrotic syndrome is usually divided into primary and secondary types (we have already written about this above). However, it is necessary to pay attention to other existing types of pathology in order to expand the general understanding of the disease.
- Congenital nephrotic syndrome is a pathology that develops in an infant before reaching 3 months of age. The congenital disease can be primary (genetically determined syndrome) or secondary (against the background of such congenital pathologies as cytomegalovirus, toxoplasmosis, syphilis, tuberculosis, HIV, renal vein thrombosis). Primary syndrome refers to an autosomal recessive inherited pathology that manifests itself literally from the first day of the baby's life. With severe proteinuria and the development of renal failure, there is a high risk of mortality - within a few months.
- Idiopathic nephrotic syndrome is a pathology that is diagnosed in children in 90% of cases. There are several histological forms of idiopathic pathology: minimal change disease, mesangial proliferation, and focal segmental glomerulosclerosis. Minimal change disease ends in complete recovery of patients in 95% of cases. With mesangial proliferation, diffuse proliferation of mesangial cells and matrix occurs in 5% of cases. The same is observed with focal segmental glomerulosclerosis, but the picture is also supplemented by segmental tissue scarring. Idiopathic nephrotic syndrome occurs at any age, most often at the age of 2-6 years. A minor infection or mild allergy, or even an insect bite, can be a provoking factor.
- Nephrotic syndrome in glomerulonephritis develops in approximately 75% of cases. It can be said that the development of the disease is a complication of inflammatory pathology of the glomeruli. According to the variant of the course of the disease, the following are distinguished:
- acute glomerulonephritis with nephrotic syndrome (lasts less than three months);
- subacute glomerulonephritis (lasts from three to 12 months);
- chronic glomerulonephritis with nephrotic syndrome (symptoms increase over the course of a year, there is a high risk of developing renal failure).
- Nephrotic syndrome in amyloidosis is one of the manifestations of systemic amyloidosis, in which protein-carbohydrate metabolism is disrupted, and amyloid is deposited in the kidney tissues - a complex polysaccharide-protein compound that causes a disorder in the functionality of the organ. The course of amyloidosis is always associated with the development of nephrotic syndrome with a further transition to a chronic form of renal failure.
- Nephrotic edematous syndrome is diagnosed in the presence of three mandatory components: changes in the permeability of the vessel walls, sodium retention, and a decrease in the oncotic pressure of the blood. The pathogenesis of such a syndrome is determined by the ratio of the activity of various body systems that regulate the maintenance of sodium-water homeostasis.
- Finnish-type nephrotic syndrome is an autosomal recessive type of congenital pathology that is detected from the neonatal period to three months. Histology reveals clear chain dilations of the proximal parts of the nephron and other changes, as well as many glomeruli with an increased diameter and fetal glomeruli. The cause of this pathology is a gene mutation (gene NPHS1). The use of this term is explained by the high incidence of this disease in Finland.
- The complete type of pathology is characterized by a full set of symptoms typical for this disease. Incomplete nephrotic syndrome is accompanied by the absence of any typical sign - for example, pronounced proteinuria is diagnosed with minor edema.
- Nephrotic syndrome in diabetes mellitus develops against the background of diabetic nephropathy. This pathological condition is considered very dangerous for the patient and consists of several stages: microalbuminuria, proteinuria and the terminal stage of chronic renal failure. The development of the nephrotic symptom complex in this case is due to changes and disorders that usually occur during the long-term course of diabetes mellitus.
- Infantile nephrotic syndrome is a pediatric term that means the disease occurs in a child under 1 year of age.
- Nephrotic syndrome in SLE is caused by the development of so-called lupus nephritis, one of the most dangerous and prognostically important manifestations of the disease. The mechanism of the disease's appearance refers to immune complex variants. Binding of antibodies to DNA and other autoantibodies to the basal membrane of the kidney glomeruli leads to stimulation of complement and recruitment of inflammatory structures to the glomeruli.
- Nephrotic syndrome with hematuria does not belong to the variants of the classic course of the disease. If the painful condition is accompanied by the appearance of blood in the urine, they speak of a mixed form of pathology.
Depending on the body's response to the generally accepted course of treatment with prednisolone, nephrotic syndrome is divided into steroid-sensitive and steroid-resistant forms.
Steroid-sensitive syndrome is characterized by the onset of remission within 2-4 weeks (less often - 6-8 weeks) from the start of therapy. In turn, the steroid-sensitive form is divided into subcategories:
- non-relapsing type (complete long-term remission);
- infrequently recurring type (relapses occur less often than twice in six months);
- frequently recurring type (relapses occur at least twice within six months);
- steroid-dependent nephrotic syndrome (recurrence of the disease is observed against the background of a reduction in the dosage of prednisolone, or no later than two weeks after discontinuation of the drug);
- late-sensitive variant (remission occurs 8-12 weeks after the start of steroid use.
Steroid-resistant nephrotic syndrome is a course of the disease in which the body's response in the form of remission is absent during a full 2-month course of prednisolone.
Complications and consequences
With nephrotic syndrome, various pathological changes occur in the body. With prolonged existence, they can lead to the development of negative consequences, for example:
- Infectious complications are a consequence of both weakened immunity and increased pathogenic susceptibility of the organism. The risk of disease is increased by such factors as loss of immunoglobulin with urine, protein deficiency, and taking immunosuppressants. Infectious complications can be provoked by streptococcal, pneumococcal infections, as well as other gram (-) bacteria. The most frequently recorded development of such pathologies as pneumonia, sepsis, and peritonitis.
- Disorders of fat metabolism, atherosclerotic changes, myocardial infarction – these complications are usually provoked by an increase in the level of cholesterol in the blood, acceleration of liver protein synthesis, and a decrease in the content of lipase in the blood.
- Calcium metabolism disorders, in turn, cause a decrease in bone density, changes in bone structure, which is fraught with many problems. Presumably, this complication is provoked by the loss of vitamin D-binding protein in the urine, deterioration in calcium absorption, as well as intensive treatment with steroids.
- Thrombotic complications are often diagnosed in patients with nephrotic syndrome. Increased coagulability is explained by the loss of anticoagulant proteins profibrinolysin and antithrombin III in the urine. At the same time, there is an increase in blood thickening factors. To avoid this complication, doctors recommend taking anticoagulants during the first six months from the moment of development of nephrotic pathology.
- The decrease in circulating blood volumes occurs against the background of hypoalbuminemia and a decrease in oncotic plasma pressure. The complication develops when the serum albumin content decreases to below 1.5 g/dl.
Among other, less frequent consequences of nephrotic syndrome, hypertension and iron deficiency anemia can be distinguished.
Relapse of nephrotic syndrome can develop in the steroid-dependent form of the disease. To prevent repeated episodes of the disease, patients undergo a detailed examination and carefully select treatment taking into account all available options. The frequency of relapses depends on the severity of the disease, as well as on the general condition of the patient's body.
Diagnostics nephrotic syndrome
The main diagnostic criteria for nephrotic syndrome are clinical and laboratory test data:
- presence of indicators of severe proteinuria (more than 3 g/day for adults, more than 50 mg/kg/day for children);
- hypoalbuminemia levels less than 30 g/l, as well as dysproteinemia;
- varying degrees of swelling (from relatively minor swelling to anasarca);
- presence of hyperlipidemia and dyslipidemia;
- active coagulation factors;
- Disrupted metabolism of phosphorus and calcium.
Questioning, examination and instrumental diagnostics are also mandatory and informative. Already during the examination the doctor may notice generalized swelling, dry skin, the presence of plaque on the tongue, a positive Pasternatsky symptom.
In addition to a medical examination, the next step should be diagnostic procedures - both laboratory and instrumental.
Laboratory tests include mandatory blood and urine sampling:
Complete blood count for nephrotic syndrome |
The disease is characterized by increased levels of platelets, leukocytes and ESR, and decreased levels of hemoglobin. |
Biochemical blood test for nephrotic syndrome |
The quality of protein metabolism is characterized by hypoproteinemia, hypoalbuminemia, and an increase in the amount of α-globulins. In addition, an increase in the level of cholesterol and triglycerides is noted. Indicative of impaired renal function are increased levels of urea, uric acid, and creatinine. If the underlying cause of the nephrotic symptom complex is glomerulonephritis, the doctor will pay attention to the presence of signs of an inflammatory process (increased C-reactive protein, increased seromucoid levels, hyperfibrinogenemia). |
Immunological blood test |
Allows to record the presence of T and B lymphocytes, immune complexes, and lupus cells in the bloodstream. |
Hyperlipidemia in nephrotic syndrome may be an initial sign of the development of renal failure, but not always: sometimes it simply indicates the presence of atherosclerosis, or certain problems with the patient's nutrition. Special laboratory studies allow us to detect fractions belonging to lipids. We are talking about low-density lipoproteins, high-density lipoproteins, the total cholesterol and triglyceride index.
Hypercholesterolemia in nephrotic syndrome is secondary. In a healthy person, elevated cholesterol levels are defined as values > 3.0 mmol/L (115 mg/dL). According to the ESC/EAS guidelines, there are no guidelines for the cholesterol level that determines hypercholesterolemia. Therefore, there are five specific ranges of LDL-C levels, which determine the treatment strategy.
General urine analysis |
The disease is characterized by cylindruria, hyperproteinuria. Erythrocytes may be found in the urine, the specific gravity increases. |
Bacteriological examination of urine |
Helps identify bacteria found in urine (in the presence of bacteriuria). |
Test according to Nechiporenko |
An increase in the content of cylinders, leukocytes and erythrocytes is noted. |
Zimnitsky test |
Allows to determine hyperisosthenuria and oliguria, characteristic of the nephrotic symptom complex. |
Rehberg-Tareev test |
Oliguria and impaired glomerular filtration are noted. |
Proteinuria is determined during a general urine analysis: the amount of protein usually exceeds 3.5 g/day. The urine is cloudy, which serves as additional evidence of the presence of protein, pathogenic microorganisms, fats, and mucus.
Instrumental diagnostics includes:
Kidney biopsy |
It is performed by taking organ tissue for further microscopy. This procedure allows to characterize kidney damage. |
Ultrasound of the kidneys |
Helps to examine the structure of organs, sizes, localization, shape of kidneys, determine the presence of tumor processes, cysts. Nephrotic syndrome on ultrasound is also characterized by the presence of ascites. |
X-ray of the lungs |
The disorders consist of pathological changes in the pulmonary system and mediastinum. |
Dynamic scintigraphy |
Allows you to assess the flow of urinary fluid from the kidneys through the ureters to the bladder. |
Urography |
A radiological procedure based on the kidneys' ability to excrete special contrast agents after their introduction into the body. Radiological signs of nephrotic syndrome may be expressed in polymorphism and asymmetry of disorders, which depends on the ratio of inflammatory and sclerotic processes in the organs. |
Electrocardiography |
It is performed to assess electrolyte disturbances in the body in case of nephrotic pathology. |
Differential diagnosis
Differentiation is made between various glomerulopathies, which in turn can cause the development of the disease:
- Minimal change disease (lipoid nephrosis) is the most common underlying cause of idiopathic nephrotic syndrome in pediatrics;
- focal segmental glomerulosclerosis is a rare form of steroid-resistant nephrotic syndrome;
- glomerulonephritis (including the membranoproliferative form of the disease);
- membranous and IgA nephropathy.
Acute pyelonephritis is characterized by a sudden increase in temperature to 38-39°C, sudden weakness, nausea, and edema. Cylindruria, proteinuria, and erythrocyturia are not considered symptoms specific to pyelonephritis, and are therefore among the first indicative signs for differential diagnostics.
Acute renal failure can develop as a complication of nephrotic syndrome. Therefore, it is very important to notice the deterioration in time and provide the patient with appropriate medical care. The first stage of development of ARF is characterized by increased heart rate, decreased blood pressure, chills, and increased body temperature. After 1-2 days, oligoanutria, nausea, and vomiting are observed. An ammonia smell of breath is also characteristic.
Chronic renal failure is a consequence of the acute course of the disease and is accompanied by gradual necrosis of the kidney tissue. The amount of nitrogen metabolism products in the blood increases, the skin becomes dry with a yellowish tint. The patient's immunity drops sharply: frequent acute respiratory infections, tonsillitis, pharyngitis are characteristic. The disease proceeds with periodic improvements and deteriorations of the condition.
Differences between nephrotic and nephritic syndrome
There are two symptom complexes, the names of which are often confused: however, these are two completely different diseases that develop against the background of an inflammatory process in the glomeruli of the kidneys. Nephritic syndrome is usually provoked by an autoimmune structural lesion of the glomeruli. This condition is in all cases accompanied by an increase in blood pressure, as well as signs of urinary pathology (urinary syndrome is characterized by such signs as erythrocyturia, proteinuria up to 3.0-3.5 g / liter, leukocyturia, cylindruria). The presence of edema is not mandatory, as in nephrotic syndrome, but they may be present - in the form of mild swelling of the eyelids, forearms or fingers.
In the nephritic variant, swelling occurs not as a result of protein deficiency, but as a result of sodium retention in the bloodstream.
Who to contact?
Treatment nephrotic syndrome
A nephrologist treats patients with kidney disease and nephrotic syndrome therapy. As a rule, patients are hospitalized to determine the cause of the disease, to provide emergency care, and also when complications arise.
Clinical guidelines for the management of nephrotic syndrome
Nephrotic syndrome is a complex of symptoms and clinical signs that is usually associated with kidney disease, leading to protein loss in the urine and edema. Treatment and management of nephrotic syndrome requires close medical supervision and may include the following clinical guidelines:
- Identification and treatment of the underlying disease: Nephrotic syndrome can be caused by various kidney diseases, such as minimal change kidney disease, diabetes mellitus, nephropathy with diffuse changes in the membranes of the basement membrane, and others. It is important to identify the underlying disease and treat it according to its nature.
- Blood pressure control: Most patients with nephrotic syndrome may have elevated blood pressure. Blood pressure control and, if necessary, treatment can help reduce protein loss and protect the kidneys.
- Treatment of edema: Edema is a common symptom of nephrotic syndrome. Treatment of edema may include limiting salt intake, using diuretics, and controlling dietary protein levels.
- Correction of dyslipidemia: Many patients with nephrotic syndrome have high levels of cholesterol and triglycerides in the blood. Treatment of hyperlipidemia may be needed to reduce the risk of cardiovascular disease.
- Prevention of thrombosis: Patients with nephrotic syndrome have an increased risk of developing blood clots. Your doctor may prescribe anticoagulants or antiplatelet drugs to prevent thrombosis.
- Supportive care: In some cases, supportive care may be needed, including protein (albumin) replacement therapy or immune modulators.
- Regular medical monitoring: Patients with nephrotic syndrome should be examined and monitored regularly by a doctor to monitor the condition of their kidneys and the effectiveness of treatment.
As with any medical condition, treatment for nephrotic syndrome should be under the supervision of a qualified healthcare professional who can tailor treatment to the individual needs of each patient.
Prevention
To prevent the development of nephrotic disease, you should try to follow these rules:
- It is necessary to maintain an optimal regime of fluid intake. You can drink plain clean water, green tea, dried fruit or berry compote, cranberry or lingonberry juice. Low fluid intake can lead to bacteria "fixing" in the urinary system, as well as to the formation of kidney stones.
- It is advisable to periodically drink herbal teas based on “kidney” herbs: parsley, bearberry, lingonberry leaves, bearberry.
- In the appropriate season, it is necessary to pay sufficient attention to the consumption of birch sap, berries, vegetables and fruits (apples, cucumbers, zucchini, watermelons).
- Some diets, especially strict mono-diets, can interfere with normal kidney function. The kidneys need a full and regular supply of both fluid and food.
- Hypodynamia is harmful to the kidneys. That is why you need to lead an active lifestyle whenever possible: walk, swim, dance, ride a bike, etc.
At any first signs of kidney problems, you need to see a doctor: you cannot self-medicate (especially with antibacterial and other powerful medications). Incorrect treatment can lead to the development of serious complications, which often remain with a person for life.
Forecast
The prognosis for nephrotic syndrome may vary depending on the etiology of the disease. One can hope for a complete recovery if the symptom complex was a consequence of a curable pathology (for example, an infectious disease, a tumor process, drug intoxication). This is observed in approximately every second child, but in adults - much less often.
A relatively favorable prognosis can be discussed if a specific case of nephrotic disease is amenable to hormonal therapy or in immunosuppressive conditions. In some patients, spontaneous disappearance of relapses of the pathology is observed over five years.
In autoimmune processes, palliative treatment is predominantly carried out. Diabetic nephrotic syndrome often approaches its final outcome in 4-5 years.
For any patient, the prognosis can change under the influence of infectious pathologies, against the background of increased blood pressure, and vascular thrombosis.
Nephrotic syndrome complicated by renal failure has the most unfavorable course: the final stage can occur within two years.


 [
[