Medical expert of the article
New publications
Endometrial hyperplasia in menopause
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Menopause is a natural change in the functioning of the female reproductive system associated with age-related hormonal changes in the body. A woman loses the ability to ovulate, conceive and carry a pregnancy. During this period, health care is especially important, because hormonal changes lead to decreased elasticity of blood vessels and the occurrence of diseases with dangerous complications (strokes, heart attacks). Particular attention should be paid to diagnosed pathologies related to the genitourinary system, since during menopause there is a high risk of malignancy of neoplasms or hyperplastic age-related changes.
The endometrium (mucous layer) is an internal hormone-dependent mucous layer lining the body of the uterus. It facilitates the implantation of a fertilized egg into the uterus and the onset of pregnancy progression. The blood supply system of the placenta is formed from the vessels of the endometrium. The mucous layer is subject to cyclic transformations during the period of a woman's reproductive capacity. The endometrium reacts to hormonal changes in the body and, if pregnancy does not occur, is rejected, leading to the occurrence of menstrual bleeding. Detachment occurs to the basal level of the endometrium. With the cessation of menstrual bloody discharge, the growth of the internal mucous layer of the uterus resumes from the basal cells. The cyclical onset of menstruation continues throughout the entire period of a woman's ovulatory capacity or until pregnancy. After childbirth, the regularity of menstrual bleeding is restored and lasts until menopause.
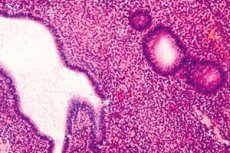
Endometrial hyperplasia is the proliferation, thickening and compaction of the mucous tissue of the uterus, which prevents the normal functioning of the reproductive system. Women of any age are susceptible to pathology. Hyperplasia is especially dangerous during menopause, because the risk of malignant neoplasms in the uterus increases significantly. Endometrial pathology is less dangerous for women in the reproductive phase. But you should not ignore the diagnosed proliferation of the uterine mucosa at any age.
A type of endometrial proliferation is adenomyosis. In the event of this pathology, the endometrium is capable of growing into the muscular and outer layers of the uterus. Gynecologists do not consider endometrial hyperplasia and adenomyosis to be synonyms or absolutely identical pathologies. These are different diagnoses in the nature of the process, although they have many similar and common features.
Causes Menopausal endometrial hyperplasia
The main underlying cause of endometrial hyperplasia (EH) is a hormonal imbalance between estrogen and progesterone. A large amount of estrogen with clearly reduced progesterone provokes EH. This pathology can occur in women of any age group. In reproductive age, endometrial proliferation often leads to infertility.
Among the factors that provoke endometrial hyperplasia in menopause, gynecologists note heredity, previous inflammatory processes of the reproductive system, abortions, the use of oral and intrauterine contraceptives, endocrine pathologies that cause changes in the hormonal background of the entire female body and the menstrual cycle, in particular.
 [ 3 ]
[ 3 ]
Risk factors
The risk group for diagnosis of endometrial hyperplasia includes women with a history of:
- diabetes mellitus,
- obesity,
- hypertension complicated by hypertensive crises,
- tumor processes in the uterus,
- polypous neoplasms in the reproductive system,
- disorders of the liver and thyroid gland,
- inflammatory gynecological diseases,
- surgical interventions on the reproductive organs.
Pathogenesis
During menopause, the height of the endometrium in the uterine cavity should not exceed 5 mm. Changes in hormonal balance can cause pathological chaotic cell division, which leads to complex morphological transformations of the structural elements of the tissue. Proliferative processes increase the thickness of the endometrium and lead to an increase in the volume of the uterus. Hormone-dependent endometrial tissue is sensitive to the level of estrogen in the body. Disruption of the normal functioning of tissue units under the influence of hormones can cause benign complications, as well as serve as the basis for the emergence and development of malignant neoplasms. Estrogens can provoke uncontrolled division of endometrial cells. Estrogens have an internal origin - pathological processes in the ovaries, as well as an external one - inadequately selected hormonal agents or a therapy regimen. Normally, if there are no hormonal disorders, progesterone in the second phase of the cycle has an estrogen-suppressing effect and protects the endometrium from pathological proliferation. Hyperplasia of the tissue of the inner layer of the uterine body is promoted by conditions of prolonged exposure to estrogen hormones. In the absence of the protective effect of progesterone (in all conditions when there is a lot of estrogen and little progesterone). For the development of endometrial hyperplasia, the duration of exposure and doses of estrogen are important.
Such violations occur when:
- ovarian dysfunction, especially before menopause;
- polycystic ovary syndrome (PCOS);
- hormonally active ovarian tumors;
- obesity.
The risk of developing EHP is high among obese women over 50 years of age, those with high blood pressure or diabetes.
Estrogens that promote endometrial hyperplasia are generated directly by the ovaries or by excess adipose tissue in obesity. Lipid tissue has the ability to produce estrogens.
A special cause of endometrial hyperplasia is the generation of large amounts of estrogen hormones in the ovary when there is a hormonally active tumor. Such a process can provoke the appearance of the most dangerous atypical type of disease, which over time, without timely adequate treatment, turns into malignant neoplasms of the uterus.
 [ 8 ]
[ 8 ]
Symptoms Menopausal endometrial hyperplasia
During menopause, endometrial hyperplasia may be asymptomatic.
The main symptoms of endometrial hyperplasia in menopause are - proliferation of the endometrium more than 5 mm in height and an increase in the body of the uterus. During menopause, any uterine bleeding or bloody vaginal discharge, regardless of its volume (heavy or scanty), duration and frequency should be perceived as an alarm signal and a possible symptom of a malignant process.
Common accompanying symptoms include rapid fatigue, weakness, lethargy, frequent headaches, hypertension, and impaired ability to work. In the case of malignancy, a sharp decrease in weight is possible.
 [ 9 ]
[ 9 ]
Forms
Diagnosed endometrial hyperplasia is classified according to the nature and type of morphology of the growths:
The glandular form is a common benign pathology of the endometrium, the characteristic feature of which is excessive progression of the growth of glandulocytes (glandular cells). As a result of the pathological division of the structural elements of the tissue, the endometrium thickens. Tubular glands turn from straight to tortuous, but their secret is freely released. The glandular form of proliferation of the endometrial layer is considered the least dangerous - malignancy occurs only in 2-4% of cases.
The glandular-cystic form is a more serious pathology, in which not only an increase in the growth of glandulocytes is observed, but also the appearance of cystic formations in the inner layer of the uterine body. Cysts appear as a result of the impossibility of free evacuation of the secretion of glandular cells. The identified glandular-cystic form of endometrial hyperplasia in 7% of cases is prone to degeneration into malignant neoplasms.
The atypical form (adenomatosis) is diffuse or focal. The most dangerous hyperplastic condition of the endometrium. Malignancy of this form of endometrial hyperplasia in childbearing age is 10% of cases, and in the period of premenopause, menopause and postmenopause it reaches 50%. Treatment of the pathology is urgent and mainly surgical.
One type of endometrial hyperplasia, classified by localization and limitation of the pathological process, is focal growths of the inner layer of the uterus - polyps. They are distinguished by morphology - glandular, fibrous and glandular-fibrous. Treatment is surgical. The prognosis is favorable. The percentage of malignancy is small. But the presence of endometrial polyps provokes favorable conditions for the development of the oncological process.
Any form of hyperplastic endometrial pathology in menopause requires close attention, since each of the described proliferative conditions of the endometrium can lead to the provocation of a serious oncological disease.
Complications and consequences
The occurrence of endometrial hyperplasia during menopause has many negative aspects. First of all, immunity weakens with age, which means that it is more difficult for the body to effectively protect itself from all sorts of diseases. Previously undergone operations and diseases affect the patient's health. Endometrial hyperplasia proceeds for a long time without any symptoms, and the consequences of adenomatosis during menopause can be its transformation into a malignant tumor. Regular examination by a gynecologist and ultrasound diagnostics allow timely detection of pathology, which significantly reduces the risk of developing oncological complications.
Complications arising from endometrial hyperplasia in the menopausal period:
- recurrent course (despite proper therapy, the disease tends to recur);
- problems with the genitourinary system (neoplasms can compress adjacent organs, resulting in acute urinary retention and disruption of its normal outflow);
- risk of malignancy of the process of hyperplastic state of endometrial tissue;
- anemic conditions (uterine bleeding can be quite heavy, resulting in a significant decrease in the level of hemoglobin in the bloodstream).
Diagnostics Menopausal endometrial hyperplasia
To prevent the progression of endometrial hyperplasia during menopause, it is necessary to undergo a preventive examination by a gynecologist twice a year.
During a routine visit to the doctor, a detailed anamnesis is collected (patient complaints, life history, gynecological anamnesis), general health assessment, examination of the patient on a gynecological chair, ultrasound diagnostics of the pelvic organs, smears for the presence of atypical cells. Bacteriological or bacterioscopic studies, a general blood test, and a study of hormonal levels may be prescribed. If necessary, a hysteroscopy is performed.
Tests
To establish an accurate diagnosis and prescribe adequate therapy, the following studies are carried out:
- Complete blood count.
- General urine analysis.
- Smear diagnostics for the presence of urogenital sexually transmitted infections.
- Examination of a smear for the presence of atypical cells.
- Diagnostic biopsy.
- Hysteroscopy and separate diagnostic curettage. These procedures are quite complex and traumatic. They simultaneously play the role of research and treatment.
- Examination of the body's hormonal background using blood. Usually, the levels of FSH, LH, estradiol, testosterone, progesterone, prolactin, adrenal and thyroid hormones are determined. Examination of the level of hormones is also used if metabolic syndrome or polycystic ovary syndrome is suspected.
 [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ]
Instrumental diagnostics
For instrumental diagnostics of endometrial hyperplasia during menopause, hysteroscopy, curettage, and aspiration biopsy may be prescribed.
Hysteroscopy with diagnostic curettage is a complex procedure performed using special optical equipment - a hysteroscope. It is used for diagnostic and therapeutic (surgical) purposes. It allows for a visual inspection of the internal walls of the uterine cavity to identify general and focal pathological processes. Curettage is performed to clarify the diagnosis. The obtained material is examined in the laboratory with mandatory histological diagnostics. Hysteroscopy is a simple surgical intervention and is performed under general anesthesia.
Curettage and histological diagnostics of the obtained tissues is the main method for determining the morphological type of endometrial hyperplasia. Curettage is an instrumental expansion of the cervix, and subsequent diagnostic curettage makes it possible to distinguish hyperplasia from malignant neoplasms in the uterine cavity. The curettage procedure is performed under one of the types of anesthesia - local, epidural or general. The decision regarding anesthesia during curettage and curettage is made by the doctor, taking into account all contraindications and possible complications.
Aspiration biopsy of the endometrium (Pipel diagnostics) is performed using the Pipel aspirator. The method is based on the device drawing in a section of endometrial tissue. This type of examination is widely used in the diagnosis of endometrial hyperplasia and is uninformative in the presence of focal pathological processes. The tissue obtained by aspiration is examined in laboratory conditions. The method has a number of significant advantages: it is performed on an outpatient basis, is minimally invasive and virtually painless (it all depends on the individual pain threshold).
These diagnostic methods are used during menopause to confirm or refute a diagnosis associated with pathological processes in the endometrium.
Ultrasound diagnostics helps to determine the height and echostructure of the endometrium, the presence and exact location of cystic formations.
Transvaginal ultrasound helps to diagnose thickening of the uterine walls and heterogeneous tissue structures.
Mammography is an X-ray examination of the mammary glands to exclude proliferative processes. It is prescribed by a gynecologist in combination with other diagnostic procedures.
In ambiguous situations, magnetic resonance imaging may be prescribed.
Very rarely, research using radioactive phosphorus is used.
What do need to examine?
Differential diagnosis
For differential diagnosis, the doctor should make sure that there are no general systemic diseases, the symptom complex of which is accompanied by uterine bleeding: hematological diseases, liver pathologies, thyroid gland, adrenal glands. It is necessary to exclude organic lesions of the ovaries - hormone-active neoplasms (thecoma, hormone-producing granulosa cell tumors of the ovaries, fibroma, Brenner tumor). In old age, it is necessary to differentiate endometrial hyperplasia from malignant lesions of the uterus, hormone-producing ovarian tumor, uterine myoma.
Treatment Menopausal endometrial hyperplasia
Therapeutic tactics for GPE depend on the diagnosed endometrial pathology, the patient’s age, the etiology and pathogenesis of the disease, and concomitant gynecological and extragenital pathology.
Treatment for endometrial hyperplasia can be carried out in several ways.
Medicines used for conservative treatment of endometrial hyperplasia in menopause are hormone-containing drugs.
Progesterone (a female sex hormone produced in the second half of the menstrual cycle) has a restraining effect on the growth of the endometrium. Due to this, drugs containing a substance similar to progesterone (progestins or gestagens) are the main method of drug therapy for hyperplasia of the uterine mucosa. The range of modern hormonal drugs for the treatment of proliferative conditions of the endometrium contains the necessary doses of hormones and prevents malignancy of pathological processes in the uterus.
Progestins (medroxyprogesterone acetate, levonorgestrel, megestrol acetate) have a positive effect and lead to the complete disappearance of hyperplasia in the vast majority of women within 3-6 months of treatment.
There is currently no single treatment regimen for gestagens. Based on the diagnostic conclusion about the type of proliferative growths of endometrioid tissue, the doctor (gynecologist-endocrinologist) prescribes a hormonal drug, determines the dosage and duration of the course of therapy, taking into account the individual characteristics of the patient (the woman's age, her weight, concomitant diseases, side effects of the drug, cost of treatment, etc.).
Hormonal agents are prescribed exclusively by a doctor strictly according to indications. The specialist takes into account possible risks and contraindications associated with taking hormonal agents. The presence of chronic systemic diseases (rheumatism, thrombophlebitis, hypertension, diabetes, diseases of the biliary tract and liver), bad habits (smoking) and systematic alcohol consumption are taken into account. The presence of these pathologies significantly increases the possibility of developing side effects. Before and during therapy, the state of the immune and vascular systems, endocrine glands, and liver should be monitored. Blood tests (coagulogram, general blood test) and urine tests are prescribed on a planned basis.
Surgical treatment
If conservative therapy is ineffective for the treatment of endometrial hyperplasia and there is a high risk of malignancy, radical surgical methods are used.
Removal of endometrial sections (functional and basal layers) using a resectoscope. Doctors consider this method controversial, since after its use there is no stable remission and relapses of the disease are not uncommon. It is contraindicated in the presence of atypical cells and the risk of malignancy of the process.
Surgical removal of the uterus (with or without the ovaries).
Indications for surgical treatment:
- ineffectiveness of conservative treatment of hyperplastic growths of endometrial tissue;
- recurrent cases of hyperplasia;
- contraindications to hormone treatment,
- atypical hyperplasia.
In cases where histological examination of the morphology of tissue samples obtained during curettage shows a high risk of developing a malignant process in the uterus (the presence of atypia), surgical extirpation of the uterus is recommended. Only such an operation can protect a woman from developing malignant neoplasms of the uterus in the future.
Folk remedies
Nowadays, there are no really effective folk methods or recipes for treating hyperplasia. In this regard, the use of folk methods for treating endometrial tissue pathologies is permissible only in combination with or after the main treatment. The use of folk medicine must be agreed upon with the attending physician.
The vast majority of currently known folk methods of treating endometrial hyperplasia include vaginal douching or inserting tampons soaked in medicinal infusions into the vagina. It should be noted that folk methods can worsen a woman's condition, lead to a loss of time for the start of effective treatment and provoke the development of dangerous complications.
Although traditional medicine denies the positive effect of treating hyperplasia with folk methods, there are isolated cases of complete recovery.
 [ 24 ], [ 25 ], [ 26 ], [ 27 ]
[ 24 ], [ 25 ], [ 26 ], [ 27 ]
Herbal treatment
Herbalists recommend using both individual plants and herbal infusions to treat endometrial hyperplasia during menopause. Many plants contain so-called phytohormones, which can normalize and stabilize the hormonal background in women during menopause. Here are some recipes:
Decoction of one-sided ortilia (borovaya uterus). To prepare this remedy, pour 1 tablespoon of the plant with 0.5 liters of boiling water and keep in a water bath for a quarter of an hour. Then cool the decoction and strain. Take before meals 3 times. A decoction of the meadowsweet herb is prepared in a similar way, which must be consumed after meals.
Tincture of one-sided wintergreen leaves. To prepare, you will need a dried plant, which must be placed in a hermetically sealed container made of dark glass. Pour in 0.5 liters of alcohol (40%), vodka or cognac. After this, leave the product in a dark place for 2 weeks, shaking it daily. It is recommended to drink the medicine three times a day, 1 teaspoon, with water. The course of therapy is three months.
Treatment of hyperplastic endometrial condition should be complex, so several medications should be taken at the same time. Traditional medicine claims that this treatment complex will help to cope with this dangerous disease.
The course and treatment regimen are designed for sixteen weeks:
- For the first four weeks, it is necessary to take freshly squeezed beetroot and carrot juice (50-100 ml per day), before meals, take a tablespoon of flaxseed oil twice a day, washing it down with cool water. Twice a month, traditional doctors recommend douching with celandine infusion (30 g of raw material per 3 liters of boiling water).
- A medicinal tincture should be prepared (used from the fifth week of treatment), consisting of: aloe juice (400 g), flower honey (400 g) and red wine - Cahors (0.7 l). All ingredients are thoroughly mixed and the mixture is left to infuse for two weeks.
- In the fifth week of treatment, Cahors tincture and aloe juice are added to all previous procedures. The treatment procedures are continued until the end of the course of treatment.
Homeopathy
Treatment of hyperplastic conditions of the endometrium with homeopathic preparations has a number of advantages: there are no side effects, complications, allergic reactions and contraindications. Homeopathic treatment of endometrial pathology has shown positive results.
The main focus when selecting a homeopathic remedy for the treatment of hyperplasia should be on restoring hormonal balance, stabilizing the nervous system, and improving liver function. According to homeopathic doctors, failure of these organs and systems is the most common cause of endometrial hyperplasia during menopause.
The most popular homeopathic remedies for the treatment of hyperplastic conditions of the endometrium are:
- Kalium carbonicum;
- Nitricum acidum;
- Genikoheel.
Many homeopathic preparations are available in the form of granules or solutions. The standard treatment regimen is 10 drops dissolved in 30 ml of water, 3 times a day orally. The duration of therapy is 2-3 weeks. If the product is available in granules, then 6-10 granules sublingually twice a day.
The range of homeopathic preparations is huge, it is impossible to make the right choice on your own. Great importance is given to the dosage of preparations in each individual case. Therefore, the right decision is to select a homeopathic preparation from a homeopathic doctor.
Prevention
Knowing the dangers of endometrial hyperplasia during menopause, you can make a plan for preventive measures, since the pathological process can be asymptomatic. The only way to detect endometrial hyperplasia is a routine systematic examination by a gynecologist (twice a year). An ultrasound examination of the pelvic organs should be performed annually. During a visit to the gynecologist, you should feel free to ask questions of interest. Sometimes, during a conversation, deviations are revealed.
It is recommended to monitor weight indicators, lead a healthy and active lifestyle, choose the right diet and not delay visiting a doctor if inflammatory pathologies of the genitals occur. Hormonal therapy adequately selected by a specialist will help stabilize the general condition during the difficult period of menopause.
Forecast
The prognosis for diagnosed endometrial hyperplasia in menopause depends on the condition and structural morphology of the endometrioid tissue.
The risk of malignancy of the hyperplastic state of the endometrium depends on the histological picture of the inner lining of the uterus and is: with simple HE - 1-3%; with complex (adenomatous) HE - 3-10%; with simple atypical HE - 10-20%; with complex atypical HE - 22-57%.
Unfortunately, no one is immune from cancer. Modern equipment and progressive diagnostic methods help to determine endometrial pathology at the earliest stages of development. Timely visit to a doctor and prescription of competent adequate complex treatment contribute to the rapid recovery of patients with the initial stage of endometrial proliferation.

