Medical expert of the article
New publications
Cervical cytology
Last reviewed: 03.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
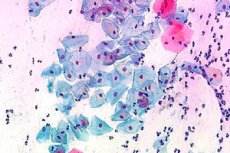
Cervical cytology is a laboratory test that determines the cellular structure of the cervix uteri (cervix of the uterus) and the cells of the cervical canal. One of the variants of cervical cytology was first used at the beginning of the 20th century by the Greek scientist Papanikolaou for the purpose of early detection and prevention of oncological diseases in gynecology.
Since then, the PAP test has been used everywhere along with the new method – ThinPrep ( liquid cytology ), which allows for the timely detection and effective treatment of hidden chronic and precancerous diseases of the cervix.
Indications for the procedure
The main task solved by cervical cytology is the prevention of the oncological process. Early detection of atypical cells allows to stop cervical cancer in time, which, according to statistics, is in third place among the most common oncopathologies in women. The danger of asymptomatic progression of the disease is great, therefore the main goal of the procedure is the timely detection of precancerous changes in cells. This makes it possible not only to increase the percentage and survival period, but also to confidently hope for a successful cure. The PAP method in gynecological practice is considered one of the fastest and most accurate for obtaining data on the presence or absence of the initial stages of oncoprocesses, cancer diseases or background pathologies of non-tumor etiology that can provoke life-threatening cancer. Many doctors call cervical cytology the "gold standard" of diagnostics and screening observation of such intraepithelial changes and conditions:
- A variety of high- or low-grade cellular abnormalities.
- The presence or absence of pathogenic microflora for diagnosing the condition of the mucous membrane of the cervix.
- Disturbances in the normal rhythm of the menstrual cycle (frequency of the cycle, its delay or absence).
- All types of diseases of viral origin - HPV (human papillomavirus) - condylomas, Herpes simplex genital (herpes).
- Infertility (sterility).
- Defects of the mucous membrane of the cervix (all types of erosion ).
- Long-term therapy with hormonal drugs.
- Abnormal vaginal discharge, including blood, especially after sexual intercourse.
Cervical cytology is necessary as a screening test if:
- Pregnancy is planned
- Births occur several times in a row (for example, 3-4 times over 4 years).
- The first birth occurred at an early age (before 18 years).
- The woman often changes sexual partners.
- Postmenopausal period (climacteric period).
- Contraception in the form of an intrauterine device is planned.
- Cytology has never been performed before, or the woman has not been examined in the last 3 years.
- The last tissue sample collected did not meet the standards or revealed changes in the cells.
- Examination of the cervix with a mirror reveals visible pathological changes (color, structure).
- The woman was diagnosed with diseases associated with immunodeficiency (HIV).
- Family history is burdened with oncological diseases (one of the immediate relatives was or is currently sick with oncological disease).
In general, annual screening cytological examination should be mandatory for every woman who has reached the age of majority. If cervical cytology shows clearly expressed clinical deviations of cellular material, the examination should be carried out more often - at least 2 times a year or in the mode of a comprehensive therapeutic plan.
Preparation
The preparation that cervical cytology involves is not complicated. The procedure itself is very quick, with virtually no discomfort or unpleasant sensations, and the preparation consists of the following steps:
- Eliminate sanitization (hygienic procedures) in the form of douching
- For several days before the procedure (2-3 days), you should adhere to a regime of abstinence in your intimate life.
- Do not use hygienic tampons, tablets, liquids, creams, suppositories and gels for the vagina
- A woman should refrain from urinating for 2 hours before the test.
In order for cervical cytology to show a reliable result, it is important to know the following information:
- Pap test and menstrual cycle are not compatible. The procedure is carried out 3-5 days before or after the onset of menstruation, it is best to do this on the 10th-12th day of the cycle.
- Cytology will not be accurate in any infectious disease, especially in the acute phase, as a rule, the analysis is carried out after basic treatment. The exception is the need to obtain a cito result, in which case, cervical cytology is carried out twice - during the disease and 2 months later for cytological control.
- A smear during intravaginal therapy will not be informative; it should be performed 5-7 days after the end of treatment.
- It is not recommended to collect tissue material in case of inflammatory processes in the vagina, which may be indicated by discharge, itching, and burning.
For more information on the conditions for preparing for the procedure, please contact your gynecologist.
Technique of implementation
Cervical cytology is considered a mandatory procedure for a comprehensive gynecological examination. This is a standard that allows for timely detection of the risks of many diseases, including cancer.
The gynecologist takes a scraping from the outer part of the cervix (exocervix), as well as from the surface of the vaginal mucosa with a special spatula (Ayre spatula). Cells of the cervical canal (cervical canal) are collected using an endobrush - a cervical probe, which allows obtaining a sufficient amount of informative material.

The doctor may also use the following instruments to collect cellular material:
- For smearing the posterior fornix of the cervix - Eyre spatula.
- Aspiration instrument - spirette, for collecting endocervical material.
- Screenet is also intended for collecting biological material from the cervical canal.
- Cervex-Brush is a sterile medical brush for taking a smear from the T-zone (the surface of the cervix and cervical canal).
- Standard tweezers.
- Gynecological speculum.
- Cervical double-sided spoon (Volkman spoon) for smearing the microflora of the cervical canal mucosa and identifying infectious diseases.
All modern instruments are sterile, most of them are used individually for each woman.
Cytology technique:
- Examination on a gynecological chair using mirrors, at the same time material is taken for cytology. The vaginal walls are expanded, the smear procedure (scraping) can cause short-term mild discomfort, but most often cytology is painless.
- Simultaneously with the scraping, material is also taken for bacteriological examination (microflora). Colposcopy can be performed together with cytology, but this is only done according to indications; usually, this procedure is prescribed separately.
- Samples of the material are applied to a special glass, fixed, secured and transferred to a laboratory technician for precise microscopic examination using staining. There is also a new method of cervical cytology - liquid (ThinPrep), in this case the material is placed in a flask and also transferred to the laboratory.
The analysis labeling is very important. The laboratory must receive a glass with the material and a special form indicating the following information:
- Glass number in accordance with the direction number of the form.
- The name of the medical facility where the procedure was performed.
- Date of analysis.
- Patient's full name.
- Age of the patient.
- Numbers, dates of the last menstrual cycle.
- Preliminary (clinical) diagnosis.
Cervical cytology does not take much time, the entire procedure lasts no more than 10-15 minutes.
What does cervical cytology show?
The main indicators of cervical cytology are summed up in two words – negative or positive result, in other words, the test shows whether there are signs of oncological disease, infectious, bacterial, viral pathology in the smear.
Let's take a closer look at what the analysis shows:
- A negative result means that the epithelial cells are not exposed to pathological processes, pathogenic flora is not detected, the cell structure is not destroyed by viruses.
- Positive results indicate that abnormal cells have been detected in the mucous membrane of the cervix, their structure and quantity are outside the standard norms. Atypical cellular elements can be varied in shape, type and size, and therefore the interpretation of the analysis is directly related to these criteria.
In modern gynecological practice, the classification of results from the author of the test, the Papanicolaou method, is considered traditional for use. The PAP-smear test method involves a detailed description of the composition, structure of cells, dividing them into 5 categories:
- Stage I – no cellular changes were detected, no atypia, which indicates a practically healthy state of the cervix. The cytological picture is within normal limits
- Stage II – the test found a certain number of cells with abnormal structure and signs of inflammation, which can be considered relatively normal, given the prevalence of inflammatory processes in the genital area. As a rule, the woman is prescribed additional diagnostic procedures to clarify the cause, nature, stage and pathogen of the inflammation.
- Stage III – the analysis shows the presence of a small number of locally grouped atypical cells with abnormalities in the structure of the nucleus or cytoplasm. This is also not a direct indication of a threatening pathology, but may be a signal of the risk of developing an oncological process. An additional procedure that clarifies the PAP test may be a morphological analysis of tissue material from the cervix (histology). A biopsy helps to exclude risks or confirm the onset of a pathological process that can be stopped with timely treatment.
- Stage IV - analysis shows a clear picture of malignant transformations of a small number of cells. As a rule, abnormal cells have too large a nuclear mass, cellular contents (cytoplasm), chromosomes also have signs of pathological changes. This stage indicates the possible onset of cancer (dysplasia). Additional examinations help to clarify the diagnosis - colposcopy, collection of material for histology, and repeated cytology is also possible.
- Stage V - the test determines a fairly large number of altered cells, which indicates the presence of an oncological process. In such cases, the results of cytology are the beginning of a comprehensive diagnostic process aimed at determining the type of oncology, its stage and the vector of treatment measures.
Decoding the results
Only the attending physician can and should interpret the test results. Any information obtained from the depths of the Internet can only be introductory and primary. The data provided below is publicly available and will help reduce the anxiety of women who are afraid of incomprehensible numbers and signs in the analysis.
Cervical cytology statistically reveals the following:
- Every ninth test out of ten determines the norm, that is, the next cytology can be safely carried out in 1-2 years for prevention and screening of the cervix. The analysis should be repeated regularly, despite the good result, since it cannot be 100% accurate and does not completely eliminate the risk of diseases.
- Every second smear out of a hundred is not informative enough due to a lack of biological or cellular material. In such cases, cervical cytology is repeated.
- Every twentieth test shows the presence of atypical changes, but this does not indicate a developed oncological process. Rather, it is a signal and a reason for a more thorough examination and subsequent treatment.
- The test result may show poor indicators, but this cannot be considered an unambiguous and final diagnosis. To clarify the nature of the pathological process and its prognosis, additional examinations are required, which are prescribed by a doctor.
The results of the cytogram can be interpreted using different methods. The Papanicolaou classifier is the classic one, but in modern gynecology it is also common to take into account other test interpretation options, for example, the American Bethesda System.
Information about the state of the epithelial tissue of the cervix can be reflected in the following table:
Presence of benign changes |
Pathological changes in epithelial tissue: dysplasia, atypia |
Invasive cancer |
|
|
Squamous cell invasive cancer |
The patient requires additional examination, observation and complex treatment. Screening cytological control is also necessary. |
Additional diagnostic procedures are required: |
A histological examination of the material is necessary, possibly clarifying the diagnosis after surgery. |
You may also be alarmed by the Latin abbreviation on the analysis form, although in fact everything is deciphered simply, according to the “territory” of the material collection:
- The urethra is the letter U.
- Endocervix, cervical canal - S.
- The vagina is the letter V.
Your doctor will provide you with further information.
 [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
[ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
Cervical cytology standards
The norm in cervical cytology is considered to be a complete absence of atypical changes in the cellular material, as well as a healthy state of the microflora. "Good" cells must meet the norms of morphological standards, that is, size, content (structure) and shape. The cytogram describes in detail the material taken from the surface layer of the cervix and from the endocervix.
The norms for cytological examination are as follows:
- Cervical cytology contains cells of a single-layer columnar epithelium. Alternatively, the test may show the presence of multilayered (metaplastic) epithelium, which is also considered normal if the smear was taken in the transitional area of the vagina.
- Multilayered epithelial cells in a smear from the vaginal portion of the cervix are also considered normal if no changes are detected in them.
- Any deviations from the norm, changes in cell morphology are described in the conclusion and may be indicators of primary inflammatory processes that are within the normal range.
- Abnormal Pap tests do not indicate cancer, with the exception of the HSIL indicator. This indicates a high risk of cancer development.
It should also be taken into account that there are indicators that indicate benign cell abnormalities. This, of course, is not the norm, but it cannot be a reason for increased concern about oncology.
List of changes within the relative norm that cytology can show:
- Atypia of inflammatory etiology.
- Atypical changes caused by the papilloma virus.
- Mixed atypical changes.
- Atypical deviations of unclear nature that require clarification.
The following diseases are among the processes in which deviations from normal boundaries may occur:
- HPV - human papillomavirus.
- Herpes.
- Candidiasis.
- Trichomoniasis.
- Pregnancy.
- Long-term use of medications, especially antibiotics.
- Vaginitis.
- Use of contraceptives (suppositories, tablets).
- Contraception with an IUD.
According to the classification of Trout and Papanicolaou, the first two classes out of five can be considered normal cervical cytology, namely:
- I – normal cytological picture
- II - ASC-US or presence of atypical cells of unspecified significance
Class III, where the degree of risk of developing pathology is designated as low, can be considered a relative norm.
Poor cervical cytology
What do bad Pap test results mean?
Poor cervical cytology does not necessarily indicate the last stage of cancer. Only a specialist, i.e. a gynecologist, can give an accurate interpretation of the study. According to the generally accepted classification, poor cytology is pathological changes in the epithelial layer of the cervix and cervical canal.
According to the generally accepted methodology, changes are designated as follows:
- 0 – the test material is unsatisfactory (poor quality, in small quantity, uninformative due to insufficient preparation of the patient).
- 1 class is normal.
- Class 2 - presence of atypical deviations.
- Class 3 - various degrees of dysplasia.
- Class 4 - precancerous condition, initial stage.
- Grade 5 - invasive cancer.
The most alarming of the above changes is considered to be class 5, however, any form of dysplasia is also a dangerous signal. Let's consider the types of dysplasia in more detail:
- A mild degree of dysplasia is a sign of the onset of an inflammatory process. It should not be ignored, since the inflammation can proceed almost asymptomatically and then develop into a more severe form.
- Moderate dysplasia is already a threatening signal, indicating that the risk of developing an oncological process is very high.
- Severe degrees of dysplasia are practically precancerous conditions.
Undiagnosed dysplasia, along with other provoking factors, can lead to a truly dangerous condition - the oncological process.
Any woman, having learned that the cytology of the cervix shows a bad result, experiences fear. Let's try to reduce its level a little by informing.
What to do if the test shows the presence of obvious atypical cells?
First of all, do not panic, but listen to and follow all the doctor's instructions. The gynecologist usually provides detailed consultation, both regarding additional diagnostic procedures, and regarding the treatment prospects and prognosis of the disease.
The following events are usually scheduled and carried out:
- Repeat cervical cytology.
- Biopsy (histological analysis of tissue from the affected area of the cervix).
- Colposcopy.
- Scraping of the cervical epithelium.
- Complete blood count.
- HPV test.
- If dysplasia is detected, it is treated (usually by cauterization).
- If a concomitant viral infection is detected, not only the woman but also her sexual partner is treated.
Timely diagnosis and adequate treatment give hope for a cure, provided that all doctor's orders are followed and the condition of the cervix is regularly monitored.
How many days does it take to do a cervical cytology?
Cervical cytology is considered a standard procedure, the technology of which has been worked out to the smallest detail. The period of material collection does not exceed 15-20 minutes, including a general gynecological examination. Then the analysis is sent to the laboratory, where a longer period of time is required for an accurate and thorough microscopic examination. If the PAP test was carried out according to all the rules, the material processing process will take about 8 days. The result can be found out from the attending physician 2 weeks after the procedure itself, sometimes this happens faster if the analysis is carried out in cito mode. It also happens that information about the test results can be received later. This is most often associated with additional samples, for example, a biochemical analysis of secretions for microflora or a biopsy according to indications.
Histological examinations and colposcopy can be scheduled on the same day as cytology, and their processing will take slightly longer than working on a single PAP test. Such complex diagnostic measures allow you to get a complete, detailed picture and make it possible to more accurately determine the course of treatment.
In conclusion, we note that cervical cytology should be a mandatory procedure for every woman. Reducing the number of cancer cases is still an unsolved problem, both for doctors and for women themselves. Timely, regular examinations, analyses and tests will allow you to be confident in your own health. Maintaining all functions of the sexual sphere in a state of harmony is a solvable problem, including with the help of preventive measures, among which cervical cytology occupies an important place.

