Medical expert of the article
New publications
A cerebral embolism
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
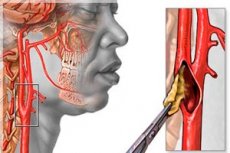
The pathology of cerebral circulation, in which emboli carried by the blood flow get stuck in the vessel, causing narrowing of the internal lumen (stenosis) or its occlusion and complete closure (occlusion and obliteration), is defined as cerebral embolism.
Epidemiology
Almost 20,000 cases of air embolism of arterial and venous vessels of the brain are reported annually.
About 15-20% of all strokes and about 25% of all ischemic strokes are the result of cerebral thromboembolism. [1]
The incidence of fat embolism of cerebral arteries is estimated to be in the range of 1-11%, and in multiple fractures of tubular bones it is 15%.
Causes of the cerebral embolism
An embolus (from Greek embolo - wedge or plug) moving along blood vessels can be an air bubble, fat cells from bone marrow, a detached thrombus (a blood clot formed in a vessel), particles of destroyed atherosclerotic plaques on the vascular walls, tumor cells or a cluster of bacteria.
Any emboli can get into blood vessels in the brain and the causes of cerebral embolism are different. [2]
Gas or air embolism of cerebral vessels - their stenosis or occlusion by air or other gas bubbles entering the bloodstream - can be caused by both brain injury, and iatrogenic causes, in particular as a complication of intravenous infusions, central venous catheter use, invasive and laparoscopic surgical interventions.
The so-called paradoxical gas embolism of cerebral vessels is determined when air emboli pass into the left atrium (atrium sinistrum) from the right atrium (atrium dextrum) filled with venous blood - due to the existing anatomical deviation of the interatrial septum in the form of open oval window in the heart (intracardiac junction of the great and small circulatory circles in the area of fosa ovalis) or in the presence of other defects of the heart septum. And such a way of air emboli entering the arteries is called paradoxical.
In addition, a pulmonary arteriovenous fistula may be a paradoxical route for air bubbles from the venous circulation into the arterial circulation and then into the left atrium and cerebral vessels. Such an anomalous fistula occurs in congenital hemorrhagic telangiectasia.
Embolism by bone marrow components (in the form of fat globules and cellular debris) entering the great circulation through the venous sinus is defined as bone marrow embolism or fat embolism of the cerebral vessels. It develops 12-36 hours after closed or multiple fractures of the tubular - long bones (femur, tibia and fibula), within which there is yellow bone marrow composed of adipocytes (fat cells). Fat emboli can also appear in the bloodstream after orthopedic surgeries.
Embolism of a cerebral vessel by a blood clot that has broken off - a blood clot formed in any other vessel - is called thromboembolism. It occurs most often in patients with atrial fibrillation and persistent atrial fibrillation, heart valve abnormalities and myocardial infarction, which lead to blood stasis and clot formation in the main chambers of the heart. Part of the clot can dislodge and get into the great circle of blood circulation, and through the aorta and carotid artery to penetrate into the cerebral vessels. And thromboembolism of small vessels of the brain can be a complication of aortic valve prosthesis.
As for the occlusion of cerebral vessels by atheromatous plaque fragments in patients with atherosclerosis, atheromatosis of the aorta and its arch, as well as plaques at the branching point of the common carotid artery into the external and internal carotid arteries are considered particularly dangerous: The internal carotid artery, which has nearly three dozen branches, supplies blood to the brain, and fragments of calcified plaque that have entered the cerebral circulation can block its distal branches.
An embolism can be septic - when a vessel is occluded by an infected thrombus that travels with the bloodstream from a distant focus of infectious inflammation. In most cases, septic cerebral vascular embolism results from right-sided infective endocarditis or infections associated with implantable cardiac devices. In addition, bacterial emboli are formed in septic thrombophlebitis (with purulent melting of a thrombus in a vein), periodontal abscess, and infection from the use of a central venous catheter.
Embolism of cerebral vessels by tumor cells is rare and is mostly caused by the primary tumor, myxoma of the heart.
Risk factors
Experts attribute the increased likelihood of cerebral embolism or predisposition to this type of cerebral circulation disorder to such factors as surgical interventions; fractures of tubular bones; atherosclerosis; heart disease; presence of foci of infection and bacteremia.
The risk of embolism is higher with arterial hypertension, obesity, diabetes mellitus, as well as smoking and chronic alcohol abuse.
Pathogenesis
Once in the arterial system, air bubbles can lead to vascular occlusion, causing ischemic infarction; direct damage to the endothelium of the inner vessel wall is also possible, with the release of inflammatory mediators, activation of the complement cascade and thrombus formation, which aggravates cerebral circulatory failure. On the mechanism of development of air embolism of vessels also read in the publication - air embolism.
The pathogenesis of fat embolism is explained by the fact that when the integrity of large bones is broken, adipocytes of the yellow bone marrow leak into the venous system, forming clots - fat emboli, which through the pulmonary blood flow into the aorta and the general blood flow, and then - into the vessels of the brain. See material - fat embolism
In septic embolism, bacteria accumulate on a damaged heart or aortic valve, pacemaker, or blood clot (formed by a permanent vascular catheter); the blood current separates the colony into pieces that travel through the bloodstream (i.e., bacteremia) until they become lodged in a brain vessel, narrowing or completely blocking its internal lumen. [3]
Symptoms of the cerebral embolism
In cerebral embolism, the first signs - their nature, duration and severity - depend on the type of embolus, its size and localization.
Small emboli can temporarily occlude small vessels in the brain and cause transient ischemic attack, a sudden loss of neurologic function that usually resolves within minutes to hours. Large emboli that result in occlusion of cerebral arteries can cause neurologic symptoms such as seizures, confusion, unilateral paralysis, slurred speech, bilateral partial loss of vision (hemianopsia), and others.
In patients with limb fractures, cerebral fat embolism is manifested by a pitting, so-called petechial rash (on the chest, head, and neck); fever; respiratory failure; and impairment and loss of consciousness progressing to coma.
The clinical presentation of septic cerebral embolism in a patient with infective endocarditis (right-sided) includes dizziness, increased fatigue, fever with chills, acute chest or back pain, paresthesias, and dyspnea.
Complications and consequences
Any cerebral embolism has the potential to cause life-threatening complications and consequences.
Thus, obliteration of cerebral vessels in air embolism leads to an acute reduction in blood flow (ischemia), oxygen starvation of the brain and brain edema - with a high risk of obstructive hydrocephalus. This develops ischemic stroke, defined as an infarction of the brain caused by cerebral artery embolism. [4]
Embolism of a brain vessel by a blood clot is complicated by embolic stroke, whose symptoms include headaches and seizures, sudden hemiplegia, (unilateral paralysis), loss of sensation and weakness of facial muscles, cognitive deficits or speech impairment.
Septic emboli in cerebral vessels in infective endocarditis threaten the development of ischemic or hemorrhagic stroke, cerebral hemorrhage and brain abscess. In addition, also emboli can infect and weaken the wall of the affected vessel, leading to the formation of a cerebral artery aneurysm.
Diagnostics of the cerebral embolism
Diagnosis of cerebral vascular embolism begins with examination of the patient, determination of pulse rate, BP measurement and history taking. In cases of fractures, the diagnosis of fat embolism is considered clinical.
Blood tests are taken: general, biochemical, for clotting factors - coagulogram, for the content of gases in arterial blood, bacteriological examination.
Instrumental diagnostics is performed using CT and MRI of the brain and its vessels, echoencephaloscopy, dopplerography of cerebral vessels, electrocardiography.
And differential diagnosis should determine the specific cause of the embolism and distinguish it from intracerebral hemorrhage.
Treatment of the cerebral embolism
Treatment of cerebral vascular embolism depends on the cause of formation and the composition of the embolus.
The mainstay of therapy for air embolism is hyperbaric oxygenation (to accelerate reduction in air bubble size and minimize ischemia), as well as anticonvulsant medications.
In cases of thromboembolism, antifibrinolytics (Alteplase, tranexamic acid preparations); anticoagulants warfarin and low molecular weight Heparin; medications of the group of vasodilators (Pentoxifylline, Pentotren) are used.
In cerebral fat embolism, symptomatic and supportive therapy is considered the mainstay of treatment. However, corticosteroids (Methylprednisolone or Dexamethasone) may be used to support cell membrane stability, reduce capillary permeability and brain tissue edema, Heparin, Meldonium (Mildronate) may be used to improve local blood circulation, aminocaproic acid preparations (Piracetam); Cerebrolysin, Citicoline (Ceraxon) may be used to protect brain cells from ischemia.
Treatment of septic embolism is prolonged use of antibacterial drugs used to treat pericarditis of infectious origin.
Prevention
Early (within the first 24 hours after injury) fracture fixation is required to reduce the incidence of cerebral fat embolism.
Preventive measures for other types of embolism consist of preventing and reducing the risk of atherosclerosis, arterial hypertension and cardiac diseases, as well as combating obesity and bad habits.
Forecast
When determining the prognosis of cerebral embolism, its etiology, nature, general condition of the patient's body and severity of concomitant disease should be taken into account. And, of course, the adequacy of medical care.
Thus, if earlier the mortality rate as a result of cerebral air embolism was up to 85%, with the use of hyperbaric oxygenation it has decreased to 21%. (although neurological symptoms remain for life in 43-75% of patients).
In thrombus embolism, 5-10% of patients die in the acute phase, from stroke, but nearly 80% of patients recover without functional disability.
Up to 10% of cases of fat embolism and 15-25% of cases of septic cerebral embolism are fatal.

