Medical expert of the article
New publications
Fat embolism
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
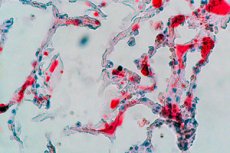
When adipose tissue cells enter the bloodstream in the form of droplets or globules of free bone marrow, visceral or subcutaneous fat, a pathological condition or clinical syndrome known as fat embolism develops, with partial or complete obstruction of blood vessels, disruption of microcirculation and homeostasis.
Epidemiology
According to clinical statistics, fat embolism is observed in 67% [ 1 ] to 95% [ 2 ] of people with severe skeletal injuries, but symptoms appear in 10-11% of cases. Quite often, mild manifestations remain unrecognized, many cases of fat embolism syndrome are not diagnosed or are diagnosed incorrectly.
Fat embolism is an almost inevitable consequence of long bone fractures. Approximately 0.9–2.2% of these cases result in the multisystem pathology of fat embolism syndrome (FES).[ 3 ],[ 4 ] The classic triad of signs described in FES is hypoxemia, neurologic impairment, and petechial rash, which typically appear 12–36 hours after injury.
The incidence of fat embolism in isolated injuries of tubular bones is estimated at 3-4%, and in fractures of long bones in children and adolescents – at 10%.
In 40% of patients, fat embolism is detected after surgical fixation of diaphyseal fractures. [ 5 ], [ 6 ]
Causes fat embolism
Most often, fat embolism is caused by fractures of long (tubular) bones and the pelvis. Thus, fat embolism in hip fractures is observed in almost a third of patients, and this condition can occur after any fracture affecting the diaphysis of the femur.
Fat embolism may develop with fractures of the bones of the leg (fibula and tibia), shoulder or forearm, as well as fat embolism with amputation of a limb.
Other possible causes are also noted, including:
- polytrauma of the skeleton with multiple fractures and damage to soft tissues;
- orthopedic surgeries, especially total hip replacement and knee replacement;
- bone marrow transplant;
- severe burns;
- diffuse changes in the pancreas in pancreatitis.
Fatal fatty embolism of the liver develops with acute necrosis of the liver against the background of dystrophy and severe alcoholic obesity.
One of the many symptoms of sickle cell anemia is fat embolism of the retinal vessels. [ 7 ]
Fat embolism is possible with injections, for example, with the introduction of the radiocontrast agent Lipiodol into a lymphatic vessel (during lymphography); glycerin-containing solutions of corticosteroids; soft tissue fillers; injections of one's own fat (autotransplantation) during lipofilling.
By the way, fat embolism syndrome can be a complication after liposuction (lipoplasty) – removal of excess fat. [ 8 ], [ 9 ]
Risk factors
In addition to the listed reasons, the following are considered risk factors for the development of fat embolism:
- insufficient immobilization of patients with fractures;
- significant blood loss;
- injuries with crushing of limb bones;
- a procedure for surgical repositioning of broken bones and displaced fragments in comminuted fractures, as well as intraosseous (intramedullary) osteosynthesis in diaphyseal fractures;
- operations on the maxillofacial bones, including plastic surgery;
- cardiac surgery with sternotomy (incision of the sternum) and transition to artificial circulation;
- decompression sickness;
- long-term use of corticosteroids.
Parenteral nutrition of patients can cause fat embolism of the vessels of the lungs and brain. [ 10 ], [ 11 ]
Pathogenesis
Explaining the pathogenesis of fat embolism, researchers have put forward many versions, but two are considered to be closest to the real mechanism of development of this syndrome: mechanical and biochemical. [ 12 ]
Mechanical trauma is associated with the release of adipocytes (fat cells) into the venous bloodstream due to post-traumatic pressure increase in the cavity of tubular bones – the medullary canal filled with bone marrow and adipose tissue – and in individual cells of spongy bone tissue. Fat cells form emboli (10-100 µm in diameter), which clog the capillary bed. [ 13 ]
Proponents of the biochemical theory argue that endogenous fat particles in the blood are converted into glycerol and fatty acids by lipase enzymatic hydrolysis and transformed into fat emboli. They first enter the pulmonary vascular system, causing deterioration of blood vessel patency and respiratory symptoms. Smaller fat globules enter the general bloodstream, causing systemic manifestations. [ 14 ]
In addition, bone marrow adipocytes produce adipocytokines and chemoattractive cytokines, which, when released into the bloodstream, can affect the functions of various organs and systems. [ 15 ]
Symptoms fat embolism
Embolized fat droplets can enter microvessels throughout the body. Thus, FES is a multi-organ disease and can affect any microcirculatory system in the body. Fat has been reported to embolize the lungs, brain, skin, retina, kidneys, liver, and even the heart.[ 16 ]
The first signs of fat embolism syndrome usually appear within 12-72 hours after the injury. Clinical symptoms include:
- shallow rapid breathing (tachypnea) and shortness of breath;
- pinpoint rash - petechiae - on the chest and shoulders, on the neck and in the armpits, on the mucous membrane of the mouth and the conjunctiva of the lower eyelids (due to the closure of skin capillaries by fat emboli);
- tachycardia;
- pulmonary edema;
- hyperthermia (as a result of cerebral circulatory disorder);
- decreased diuresis.
The intensity and range of symptoms that arise depend on the degree of fat embolism (mild, moderate or severe). There are fulminant, acute and subacute forms of fat embolism. In the subacute condition, there are three characteristic signs: respiratory distress syndrome, skin petechiae and dysfunction of the central nervous system.
Occlusion of the capillary network of the lungs by fat globules – pulmonary fat embolism – leads to hypoxemia, that is, a lack of oxygen in the blood.
And fat embolism of the brain causes numerous petechial hemorrhages in the white matter, edema and lesions of the basal ganglia, cerebellum and interlobar septa, which in more than 80% of patients is accompanied by cerebral hypoxia and CNS depression with headache, disorientation, agitation, convulsions, confusion with delirium.
Among the focal neurological symptoms, unilateral muscle paresis or increased tone of the lower extremities, associated deviation of the eyes (strabismus), and speech disorder in the form of aphasia may be observed. [ 17 ]
Complications and consequences
Neurological sequelae and complications of fat embolism may include ischemic/hemorrhagic strokes, retinal ischemia, autonomic dysfunction, diffuse brain injury, stupor, and coma. Microvascular retinal injury results in hemorrhagic retinal lesions, which are seen in 50% of patients.[ 18 ] These lesions are self-limiting and resolve within a few weeks.[ 19 ] Residual visual impairment is rare.
The development of compartment syndrome and complex regional pain syndrome is noted.
Occlusion of 80% of the pulmonary capillaries leads to increased capillary pressure and causes acute right ventricular failure, which can be fatal. Up to 10-15% of cases of fat embolism are fatal.
Diagnostics fat embolism
Currently, the diagnosis of this condition is based on clinical manifestations, and for this purpose there is a scale of major (major) and minor (minor) symptoms. [ 20 ]
Blood tests for hematocrit, platelet count, arterial blood gases and oxygen content, and detection of fat globules in peripheral plasma by infrared spectroscopy may be helpful in making the diagnosis. Patients with long bone fractures should have their blood oxygen content monitored by continuous pulse oximetry.
Early detection and verification of fat embolism is facilitated by instrumental diagnostics: general radiography of the lungs and chest; ECG; duplex ultrasound of the veins of the lower extremities; [ 21 ] CT/MRI of the brain. [ 22 ], [ 23 ], [ 24 ], [ 25 ]
Differential diagnosis
Differential diagnostics are carried out with thromboembolism and cardiogenic pulmonary edema, pneumonia, meningococcal septicemia, cerebral hemorrhage, anaphylactic reaction of various etiologies.
Who to contact?
Treatment fat embolism
In fat embolism syndrome, treatment consists of maintaining respiratory function and adequate blood oxygenation by means of artificial ventilation through a mask (with continuous positive pressure), and in cases of acute respiratory distress syndrome – endotracheal artificial ventilation. [ 26 ], [ 27 ], [ 28 ]
Infusion resuscitation – intravenous administration of fluid – is performed to avoid the development of shock, maintain circulatory volume and restore the rheological properties of the blood. [ 29 ]
Systemic corticosteroids (Methylprednisolone) are also used.[ 30 ]
In severe cases, when the cause is fatty pulmonary embolism, inotropic support of right ventricular failure with adrenergic stimulants and adrenergic agonists may be required.
In recent years, resuscitators have begun to use plasmapheresis and plasma exchange techniques. [ 31 ], [ 32 ]
Prevention
The accepted strategy for the prevention of fat embolism is aimed at early surgical stabilization of fractures, especially of the tibia and femur.

