Medical expert of the article
New publications
Atypical hyperplasia of the endometrium
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
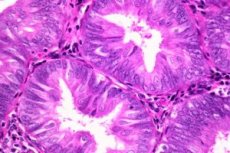
Atypical endometrial hyperplasia is a term used to describe hypertrophic changes of adenomatous nature occurring in the endometrium, in combination with atypia.
In this disease, there is a pathological spread of the mucous membrane of the uterus, and in such neoplasms there is a predominance of glands that have undergone a number of changes and differ from those tissues from which their degeneration began. In this case, there may be atypical cells, that is, those that differ in their appearance and characteristic features that are not characteristic of those cells that became the source material for their development.
Such changes in the uterine mucosa may indicate the beginning of the transformation of endometriotic hyperplasia into a malignant disease – endometrial adenocarcinoma.
Atypical endometrial hyperplasia has certain manifestations by which it can be distinguished from the initial stages of oncology development. Thus, one of the characteristic properties is the appearance of atypical changes mainly in the functional layer of the uterine mucosa, from which pathological growth occurs. If the appearance of atypical cells in the basal layer, stroma, is detected, this is one of the signs of cancer beginning in the endometrium.
Causes atypical endometrial hyperplasia
The causes of atypical endometrial hyperplasia are closely related to disorders of the hypothalamus, a part of the cerebral cortex responsible for the functioning of the endocrine system. This causes unfavorable changes in the hormonal background during menstruation. On the other hand, malfunctions of the pituitary gland, which is the main endocrine gland, affect the normal functioning of the ovaries.
As a result of such disturbances in the optimal balance of endocrine-metabolic processes, changes occur with a tendency to increase the amount of estrogens needed in the first half of the monthly cycle, and in the second half, in which the necessary hormonal background is provided by progesterone, this female sex hormone is not produced sufficiently.
The causes of atypical endometrial hyperplasia are also due to the fact that hypertrophied endometrium leads to the absence of the secretion phase, during which the uterine mucosa prepares to accept the embryo. At the same time, when the secretion phase does not occur, and the growth of the mucosa continues, after a decrease in the level of estrogens, its gradual rejection occurs. This is accompanied by prolonged and heavy menstrual bleeding, which can also occur in the intermenstrual period.
As pathological changes progress, the properties of the uterine mucosa change, which now significantly contribute to the emergence of atypical cells, which may become a sign of the development of a malignant disease.
 [ 4 ]
[ 4 ]
Symptoms atypical endometrial hyperplasia
Symptoms of atypical endometrial hyperplasia occur in the form of certain manifestations inherent to each specific character and type of development of the pathological process.
Thus, in the glandular form of the disease, which is essentially benign, there is a proliferation of the stroma and endometriotic glands. Thickening of the mucous membrane is noted, and the glands in the stroma are located incorrectly.
The severity of the glandular hyperplasia processes determines its differentiation into an active, acute stage of the disease and a dormant, chronic form.
The active form is characterized by a large number of cellular mitoses in the stroma and epithelium of the glands, which is manifested as a consequence of prolonged excessively high levels of estrogens. At the stage of chronic disease, mitoses are rarely formed, which is caused by insufficient hormonal stimulation due to the small amount of estrogens.
Symptoms of atypical endometrial hyperplasia of the glandular-cystic type are similar to manifestations of glandular hyperplasia, with the only difference being that they have a slightly greater degree of expression. One of the characteristic signs is cystic enlargement of the glands.
Forms
Atypical glandular hyperplasia of the endometrium
Atypical glandular hyperplasia of the endometrium is a process of glandular proliferation characterized by high intensity and significant pathological transformation at the structural level.
In addition to the activation of their growth and reproduction processes, endometriotic cells are subject to changes in the structure of their nuclei, which, given a certain combination of factors, can serve as a sign of the onset of malignant processes.
The foci of occurrence may be either the functional or basal layer of the uterine mucosa, or both may be involved in the development of pathology. In the case of damage to both of these layers simultaneously, the probability of the neoplasm acquiring properties and qualities of an oncological nature seems especially high.
Atypical glandular hyperplasia of the endometrium can occur not only as a result of hyperplastic endometrioid layer, but also in case of its thinning and atrophic changes.
There are two types of this disease – cellular and structural endometrial hyperplasia.
In the first case, pathological processes occur in epithelial cells and in the stroma, and the second type causes changes in the location and shape of the glands.
Complex atypical endometrial hyperplasia
Complex atypical endometrial hyperplasia is characterized by a large consolidation of the location of endometriotic glands or their individual foci.
This lesion of the uterine endometrium is characterized by a significant degree of expression of glandular proliferation. Pathological changes in structure and shape are observed in the glands affected by this process. A violation of the optimal ratio in the proliferation of glands and stroma occurs. The phenomenon of pronounced multinuclearity of the epithelium is also noted. Atypicality in the change of nuclei in this disease is not observed.
Complex atypical endometrial hyperplasia is one of the most dangerous forms of endometrial lesions in women. It can transform into uterine cancer with a high degree of risk. The probability of such a transformation into a malignant neoplasm is 22-57% of cases of the disease.
Distinctive features include the presence of pronounced proliferation of the epithelium with the appearance of atypia in cells and tissues.
When this pathology develops in the uterine mucosa, the glands acquire irregular shapes and can differ significantly in size from each other, and the polymorphic nuclei are elongated or rounded.
 [ 15 ]
[ 15 ]
Focal atypical endometrial hyperplasia
Focal atypical endometrial hyperplasia can develop according to one of the following scenarios.
In many cases, the cause of focal growth lies in fragments of tissues of the uterine mucosa that, for some reason, were not rejected. This is often caused by all sorts of endocrine disorders and hormonal imbalances.
Under normal conditions, the endometrial layer of the uterus thickens during the monthly cycle and, if fertilization does not occur, it comes out in parts along with menstrual blood. Unseparated remnants of the endometrioid layer become the cause of intermenstrual uterine bleeding, and can also subsequently cause focal proliferation of the endometrium and provoke the formation of a polyp in the internal cavity of the uterus.
Another mechanism for the appearance of endometrioid lesions is triggered by an insufficient amount of estrogen produced in the body. Due to this, the egg does not mature, which leads to prolonged irregular production of this female hormone. Ultimately, the immature egg cannot leave the ovary, and menstrual bleeding continues for a long time. In this case, the rejection of the uterine mucosa occurs gradually, and some of its particles can remain inside.
Such fragments remaining in the uterine cavity become the reason for the appearance of focal atypical endometrial hyperplasia on their basis.
The occurrence of foci of endometriotic neoplasms can be provoked by the consequences of previous inflammatory diseases of the uterus, traumatic factors, difficult births, abortions, disorders of the endocrine system, stress, problems with excess weight, etc.
 [ 16 ]
[ 16 ]
Simple atypical endometrial hyperplasia
Simple atypical endometrial hyperplasia has a number of specific characteristic features.
These include the presence of a slight predominance of glandular and stromal structures over normal ones.
There is an increase in the volume of the endometrium, as well as a change in its structure, which is manifested in the following. The stroma and glands are active, the location of the glands is uneven, some of them are subject to cystic expansion.
As for the stroma, it is necessary to note the uniform distribution of vessels in it.
Simple atypical endometrial hyperplasia also has its manifestations in the disruption of the normal order of cell arrangement, which are distinguished by their unusual, in many cases round, shape. This disease is also characterized by significant polymorphism of cell nuclei, without a tendency to atypia.
In addition, the features include the presence of cellular dyspolarity, anacytosis, hyperchromatism and an increase in the size of nuclei. Among the cellular changes, the phenomena of vacuole expansion and cytoplasmic eosinophilia are also observed.
The degree of risk of degeneration into a malignant neoplasm is determined with a probability of 8 to 20 cases out of 100.
Diagnostics atypical endometrial hyperplasia
Diagnosis of atypical endometrial hyperplasia involves a number of appropriate measures aimed at identifying characteristic changes and signs indicating the onset of development or the presence of a certain stage of this disease in a woman’s body.
The initial diagnostic action is a gynecological examination, as a result of which, if suspicions arise, the specialist can prescribe additional examinations using all possible methods and techniques.
When examining the pelvic organs using ultrasound diagnostics with intravaginal administration, it is possible to detect an increase in the thickness of the endometrium, or to determine the presence of polyps in the uterine cavity based on formations of the corresponding shape.
The hysteroscopy method involves examining the uterine cavity using a special optical device and performing separate diagnostic curettage for histological analysis to determine the type of hyperplasia.
This diagnostic method is one of the most appropriate, as it ensures high accuracy of diagnosis.
Diagnosis of atypical endometrial hyperplasia is also made by aspiration biopsy, when a fragment of endometrial tissue is separated for histological examination.
Estrogen and progesterone levels, and in some cases also adrenal and thyroid hormones, can also help to identify the disease and make a clear diagnosis.
Treatment atypical endometrial hyperplasia
Treatment of atypical endometrial hyperplasia can currently be done through surgical intervention and treatment with hormonal drugs.
Surgical treatment in one of its methods is reduced to the procedure of scraping the internal cavity of the uterus. This therapeutic and diagnostic operation, carried out both independently and accompanied by hysteroscopy, is aimed at removing from the uterus all possible endometrium subject to hyperplasia. At the same time, the data collected by hysteroscopy allow an accurate determination of the type of hyperplasia.
Another treatment option is to use electric current or laser beam during hysteroscopy.
An extremely radical method is extirpation of the uterus, which consists of the complete removal of this female organ. Indications for its use on a strictly individual basis may only be the ineffectiveness of all other types of treatment, the atypical nature of hyperplasia, and relapses of the disease.
Treatment of atypical endometrial hyperplasia may be less radical than surgical intervention.
A course of hormonal treatment is prescribed in addition to surgical treatment based on the results obtained from histological examination.
Hormonal treatment involves the use of drugs from the gestagen group, the introduction of an intrauterine levonorgestrel-containing IUD, as well as combined oral contraceptives to regulate the menstrual cycle, which helps to normalize the processes of cyclic growth and rejection of the endometrium.
Prevention
Prevention of atypical endometrial hyperplasia, as well as measures aimed at preventing the occurrence of most female diseases, comes down mainly to regular visits to a gynecologist.
There is no need to remind once again about such a significant factor influencing the health and vitality of the whole organism as the need to lead a healthy lifestyle.
Playing sports and engaging in regular physical activity significantly reduces the likelihood of falling into the risk group for developing this disease.
It is also important to adhere to a proper diet and monitor the maintenance of your body mass index within your individual optimum.
The use of combined oral contraceptives is also a relevant factor.
Prevention of atypical endometrial hyperplasia also involves timely detection of disruptions in the ovulation process with immediate initiation of treatment.
Methods of contraception using hormonal drugs, which prevent proliferation, that is, excessive enlargement of the endometrium due to the active process of cell division, are also a preventive measure.
Forecast
The prognosis of atypical endometrial hyperplasia is based primarily on the fact that special attention must be paid to the degree of probability of its transition to the category of oncological diseases.
For young women, the issue of choosing a treatment that combines the highest possible effectiveness with an unconditional possibility of preserving their reproductive function becomes relevant. In this case, a course of conservative therapy with progestins seems to be the most appropriate.
However, if cellular atypia is detected, which implies the possibility of persistent processes, progression and relapse, such cases require closer attention.
In older women who have entered menopause, in most cases, a hysterectomy is an almost unambiguous prescription. Especially if atypical hyperplasia is present.
Thus, the prognosis of atypical endometrial hyperplasia in the absence of cell atypia when using conservative treatment methods under the supervision of competent specialists in the field of gynecology is favorable, since it assumes the preservation of the ability to bear children in young women.

