Sialadenitis: causes, symptoms, treatment
Last reviewed: 12.03.2022

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
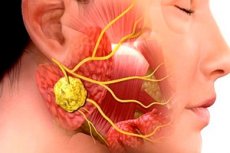
Inflammatory pathologies in surgical dentistry are very common. Even the use of antibiotic therapy does not reduce the incidence of maxillofacial inflammation and its complications. This situation is due to the late appeal of patients to doctors, frequent self-treatment of patients, etc. One of the typical infectious and inflammatory diseases of this kind is sialadenitis, or sialoadenitis, an inflammation of the salivary gland, often provoked by viruses or bacteria. Pathology is accompanied by a number of characteristic clinical signs, and the diagnosis is established based on the results of bacteriological and cytological studies, as well as instrumental diagnostics.
Epidemiology
The exact prevalence of submandibular sialadenitis is not clear. Submandibular sialadenitis accounts for about 10% of all cases of sialadenitis. It accounts for 0.001 to 0.002% of all hospital admissions. There are no age or gender differences. [1]
Bacterial and viral sialadenitis affects mainly elderly and senile people.
Epidemic parotitis mainly affects children, less often adults (women more often). To date, mumps occurs as a sporadic disease, due to early vaccination of children.
A purulent form of sialadenitis is often recorded, which is due to the late treatment of patients for medical help.
Causes of the sialadenitis
The development of sialadenitis is due to viral or microbial lesions of the salivary glands. The microbial inflammatory process can be triggered by bacteria present in the oral cavity, or released from various infectious foci in the body. Adjacent phlegmon, acute respiratory diseases (tonsillitis, pneumonia, bronchitis), maxillofacial and dental pathologies often become sources of infection.
Perhaps the appearance of the disease due to injuries and operations in the maxillofacial zone, the ingress of foreign bodies into the salivary canal (fish bones, food particles, hairs, etc.), canal stone formation.
Sialadenitis of a viral nature is most often provoked by cytomegaloviruses, influenza virus, adenoviruses, paramyxoviruses, Coxsackie viruses, herpes simplex, etc. Fungal sialadenitis, syphilitic, and tuberculous also occur.
The spread of infection can occur through the canal mouth, through the blood or lymphatic fluid.
Risk factors
Risk factors for the development of sialadenitis are:
- weakened immune defenses, recent diseases;
- congestion in the salivary canals;
- disorders of salivation caused by infectious and inflammatory pathologies;
- surgical operations;
- tuberculosis;[2]
- syphilis;
- maxillofacial trauma.
The risk group includes the elderly, people suffering from eating disorders, pathological dry mouth, as well as undergoing radiation treatment, or regularly practicing antibiotic therapy without strong indications, postoperative condition, [3] intubation, the use of anticholinergics. [4]
Additional (indirect) predisposing factors can be:
- violations of oral hygiene;
- wrong way of life, the presence of a number of bad habits;
- ignoring visits to doctors, the practice of self-treatment.
Pathogenesis
The salivary glands are divided into paired large and unpaired small. Large glands include parotid, submandibular, sublingual. Small glands are represented by the labial, buccal, lingual, palatine, and oral floor glands. Each of these glands has a parenchyma, an interstitium, and a duct system.
The causative agent of mumps, one of the variants of acute sialadenitis, is a filterable virus. A person becomes infected by its direct transmission from the patient, the route of transmission is airborne (but infection through objects used by the patient is not excluded).
Bacterial sialadenitis can develop with any severe pathologies. The way the infection spreads is stomatogenic, as well as through the blood and lymphatic fluid. The microflora is usually of a mixed type: streptococcal, pneumococcal, staphylococcal, etc., which enters through the excretory glandular duct.
In patients with lymphogenous infection, the lymphoid network of the parotid gland often occurs: this process is a consequence of nasopharyngeal or mandibular inflammation, pathologies of the teeth or tongue.
The etiology and pathogenesis of chronic sialadenitis are unclear and poorly understood. Doctors suggest that the development of the disease is associated with common pathologies in the body - in particular, with hypertension, atherosclerosis, deforming spondylosis, diseases of the digestive tract.
Symptoms of the sialadenitis
Acute sialadenitis can occur with different intensity. With a mild course, the clinical picture is mild, without an increase in body temperature and without pain in the parotid glands, which swell only slightly. With a moderate course, there is a general malaise, pain in the head and muscles, chills, dryness of the oral mucosa, pain and swelling of the parotid gland. The secretion of saliva is slightly reduced. Symptoms last about 4 days, after which there is a gradual relief. In severe cases of acute sialadenitis, the parotid gland is greatly enlarged, and the submandibular and sublingual glands may be involved in the process. Salivation increases, the temperature reaches high rates (up to 40 ° C), the development of purulent-necrotic complications is possible. Under favorable circumstances, after about a week, the temperature begins to drop, signs of an inflammatory reaction gradually subside. However, the risk of abscess formation remains, as well as the risk of developing meningitis, encephalitis, paralysis of the cranial and spinal nerves, etc.
Viral sialadenitis of the parotid glands is manifested by pain at the moment of opening the oral cavity and when trying to turn the head to the side. There is swelling of the buccal, mandibular, maxillary zone and the upper part of the neck. When probing, a painful induration with a smooth surface is detected, which does not go beyond the borders of the parotid gland. The spread of pathology to the surrounding tissues occurs with the development of a purulent process.
When the submandibular gland is affected, patients complain of swallowing pain. Edema extends to the sublingual and submandibular zone, chin and upper neck. With the defeat of the sublingual glands, pain appears when moving the tongue, the sublingual folds increase. Involvement of the minor salivary glands occurs in multiple pathologies.
The first signs of chronic sialadenitis may go unnoticed and are detected by chance. Patients notice discomfort in the area of the parotid gland (or two glands), less often - occipital pain. A soft swelling in the affected area is visually determined, without obvious pain. There are no changes in the skin, the oral cavity opens painlessly, mucous tissues are without pathologies, salivation is not disturbed (may decrease during a relapse). At the advanced stage of chronic sialadenitis, patients have general weakness, fatigue, hearing impairment, and sometimes dryness of the oral mucosa. Swelling in the area of the affected glands is constant, without pain.
Interstitial sialadenitis is characterized by seasonal exacerbations (in the cold season), in which painful seals form, body temperature rises.
Sialadenitis in children
Sialadenitis can develop in childhood, even in newborn babies. True, the etiology of the onset of the disease in infants has not yet been determined. It is known that inflammation of the mammary gland in the mother contributes to the development of the disease. Sialadenitis of newborns is differentiated from osteomyelitis of the condylar mandibular process, indicating the development of septicopyemia.
In general, the main causes of sialadenitis in children are mumps and cytomegalovirus. In addition, it is important to know about the possible development of Herzenberg's false parotitis, which does not apply to sialadenitis and is an inflammation of the lymph nodes located near the parotid salivary gland. The clinic of diseases is very similar.
Tuberculosis and syphilitic etiology of the disease are uncharacteristic for childhood. The clinical picture is characterized by more serious intoxication than in adults, as well as a large percentage of the development of purulent or purulent-necrotic tissue fusion.
Stages
Sialadenitis develops with the passage of the corresponding three stages: initial, clinically pronounced and late.
The initial stage is not accompanied by severe clinical symptoms. However, swelling increases, lymphatic congestion is noted in the affected area, the connective tissue loosens, and blood vessels dilate. The terminal glandular segments are preserved, but they accumulate mucin and mucopolysaccharides, inflammatory markers. Interlobar ducts become wider, collagen fibers become denser.
The second stage is characterized by the following picture:
- there is atrophy of the terminal glandular segments;
- infiltrates are formed on the basis of plasma structures, lymphocytes and histiocytes in the connective tissue base;
- the mouths are surrounded by fibrous tissue;
- inside the channels there is an accumulation of desquamated epithelium and lymphocytes.
The third stage is accompanied by almost complete atrophy of the glandular parenchyma, its connective tissue replacement, proliferation of the blood supply network, expansion of the intralobar ducts (or narrowing due to compression by connective tissue and fibrous structures).
Forms
The classification of the disease is quite extensive. So, according to the course of the inflammatory reaction, acute and chronic sialadenitis are distinguished.
Acute sialadenitis of the parotid gland proceeds according to the type of mumps, or the well-known "mumps". In general, the parotid glands are most often affected, less often the submandibular and sublingual salivary glands. An acute process is easier to treat than a chronic one.
Depending on the state of the parenchyma, the following types of chronic disease are distinguished:
- chronic parenchymal sialadenitis - accompanied by damage only to the glandular stroma (as in patients with epidparotitis);
- chronic interstitial sialadenitis - in addition to the stroma, it is accompanied by lesions of the glandular parenchyma (as in patients with cytomegalovirus sialadenitis).
- Chronic sclerosing sialadenitis (Küttner's tumor) is an IgG4-associated sclerosing disease and has distinct histopathological features such as dense lymphoplasmacytic infiltrate, sclerosis, and phlebitis obliterans. [5]
Interstitial sialadenitis is otherwise called chronic productive sialadenitis, chronic sclerosing parotitis, Kuttner's inflammatory tumor, chronic atrophic sialadenitis, fibroproduc- tive sialadenitis, symptomatic sialopathy, hormonal sialosis. The etiology of the disease is poorly understood.
Influenza sialadenitis develops during periods of influenza epidemic, which occur mainly in winter. Patients show signs of acute sialadenitis of one or more salivary glands. Most often, the parotid gland suffers, inflammation grows rapidly and spreads to the paired gland.
Depending on the location of the lesion, they distinguish:
- mumps, sialadenitis of the parotid glands;
- submaxillitis - damage to the submandibular gland;
- sublinguitis sialadenitis of the sublingual gland.
According to inflammatory characteristics, sialadenitis of the salivary gland is:
- serous;
- hemorrhagic;
- purulent;
- connective tissue;
- granulomatous;
- fibroplastic;
- destructive;
- undeformed;
- cirrhotic.
Depending on the etiology, there are:
- traumatic inflammatory process;
- toxic;
- autoimmune;
- allergic;
- obstructive (with blockage or cicatricial contraction).
Calculous sialadenitis is a type of obstructive pathology caused by blockage of the duct by a salivary gland stone.
If the inflammatory disease progresses, then purulent-necrotic or gangrenous sialadenitis develops in the future. At the same time, there is a picture of severe phlegmon with severe edema, infiltration, hyperemia, fluctuation, etc.
Ductal sialadenitis (or sialodochitis) is a consequence of congenital defects of the salivary glands (strictures and ectasias) in combination with weak immunity and hyposalivation, stagnation of saliva inside the ducts.
Complications and consequences
The acute course of sialadenitis can be complicated by damage to the oculomotor, optic, abducent, facial, vestibulo-cochlear nerves, as well as mastitis, pancreatitis, and nephritis. Often, boys and men develop orchitis.
If acute sialadenitis occurs against the background of general pathologies, it can be complicated by the divergence of the pathological process into the peripharyngeal space, into the tissues surrounding the carotid artery and the internal jugular vein. In some patients, purulent contents erupt into the external auditory canal. Rarely, damage to the walls of large vessels is observed, which entails bleeding. It is also possible venous thrombosis and blockage of the sinuses of the meninges.
A late complication of advanced purulent sialadenitis is the formation of fistulas and parotid hyperhidrosis.
If bacterial sialadenitis is not treated, it is possible to develop massive swelling of the tissues of the neck, which can provoke respiratory obstruction, septicemia, bone cranial osteomyelitis, and trigeminal neuritis.
Diagnostics of the sialadenitis
Common clinical diagnostic methods include questioning the patient, examining him, and palpation. Additionally, a laboratory study of blood and urine is prescribed. If we are talking about a child, then it is necessary to check with the parents whether he had previously had epidemiological parotitis, whether he had contact with patients.
If chronic sialadenitis is suspected, then the annual frequency of relapses, the size of the gland in different periods of the inflammatory process are specified. Attention is drawn to the condition of the skin over the site of the lesion, the volume and nature of the salivary fluid, the condition of the excretory salivary canals.
Mandatory appointment:
- assessment of secretory function;
- cytology, microbiology, salivary secretion immunology;
- contrast sialography;
- computed tomography;
- radiosialography;
- ultrasound;
- punch biopsy.
Many pediatric patients are indicated for electroencephalography, which is necessary to assess disorders of brain bioactivity.
Mandatory instrumental diagnostics includes sialometry, during which a polyethylene catheter is used, which, after preliminary bougienage, is inserted into the salivary duct. Manipulation is performed on an empty stomach, and the procedure itself lasts about 20 minutes. It provides information on the volume of salivary production and on the physical characteristics of the secretion. [6]
Contrast sialography is performed at the stage of remission of the disease, as it can provoke a relapse. Radiopaque solutions are injected into the salivary gland using a syringe and a polyethylene catheter.
Special instrumental diagnostics is represented by the following procedures:
- cytology of smears of salivary secretion;
- electroradiography with contrast;
- salivary gland scanning method;
- puncture with biopsy and subsequent histology.
Ultrasound is most often performed in the form of sialosonography - a study that allows you to consider the full picture of the glandular structure. The doctor has the ability to detect sclerotic disorders in tissues, blockages, tumor processes, stones, determine their number, size.
With bacterial sialadenitis, nonspecific changes are determined during ultrasound. At an early stage of development, there is an increase in echogenicity and expansion of the duct, and the presence of anechoic foci indicates a possible abscess. [7]
Magnetic resonance and computed tomography can exclude the presence of stones in the ducts and clarify the depth of the pathological process.
Laboratory tests include a general examination of blood and urine, as well as salivary fluid. A high level of leukocytes can be found in the blood, which is one of the signs of an inflammatory process. In a biochemical blood test, sugar indicators are important, and in a urine test, salt composition. In the salivary secretion, it is often possible to identify leukocytes, pus, and bacterial flora. It is necessary to investigate the physico-chemical characteristics of the secret.
Differential diagnosis
First of all, it is important to determine the root cause of the pathological condition, to find out whether the disease belongs to an atherogenic, infectious, neoplastic, autoimmune, metabolic nature. Rheumatological and autoimmune pathology should be excluded.
Interstitial sialadenitis is differentiated from chronic parenchymal sialadenitis, sialodochitis, tumor processes, mumps. For diagnosis, an assessment of typical symptoms, a cytological and sialographic picture in accordance with the diseases is used.
In general, sialadenitis should be distinguished from salivary stone disease, salivary gland cysts, tumor processes. Diagnosis is performed based on clinical symptoms, sialometry data, cytological examination of salivary secretions, radiography and sialography, puncture and excisional biopsy.
It is important for patients to understand that sialadenitis or sialoadenitis are two equivalent concepts that are completely interchangeable.
In some cases, the features of the clinical picture of the disease and laboratory parameters may require a wider diagnostic search: in such a situation, a biopsy of the salivary glands is recommended to make an accurate diagnosis.
Who to contact?
Treatment of the sialadenitis
A patient with acute sialadenitis is prescribed treatment aimed at inhibiting the inflammatory response and normalizing salivation. Assign bed rest at the time of the rise in temperature. According to indications, warming compresses, ointment dressings are applied to the areas of compaction, physiotherapy is carried out (light therapy, heat therapy - sollux lamp, UHF, UV irradiation). Provide high-quality care for the oral cavity, using rinses, irrigations.
With viral sialadenitis, irrigation with interferon 5 times a day has a good effect (with early practice - for 1-2 days). If the salivary function decreases, then 0.5 ml of antibiotic solutions of 50,000-100,000 ED of penicillin and streptomycin are injected intraductally with 1 ml of novocaine 0.5%. In addition, blockade with novocaine and penicillin or streptomycin is performed. If purulent inflammation progresses, foci of tissue fusion are found, then a surgical operation is prescribed.
Pilocarpine with sialadenitis is taken orally, up to four times a day, 6 drops of a 1% solution. Such treatment is appropriate for a serous inflammatory process. A good effect is noted when setting compresses with dimethyl sulfoxide, dimexide, which provides analgesic, anti-inflammatory, anti-edematous and bactericidal effects. The compress is placed on the area of inflammation for about half an hour a day. The course of treatment consists of ten procedures, or until relief occurs.
With gangrenous sialadenitis and a severe course of the disease, surgical treatment is prescribed, which consists in opening the glandular capsule: intervention on the parotid gland is carried out according to the Kovtunovich technique.
In chronic sialadenitis, treatment is directed mainly to increasing immunity, optimizing salivary function, preventing relapse, improving tissue trophism, eliminating congestion, and inhibiting sclerotic and degenerative processes.
The complex therapy includes such drugs:
- sodium nucleinate 0.2 g three times a day for two weeks (for chronic sialadenitis, such courses should be carried out up to three times annually);
- potassium iodide 10% 1 tbsp. L. Three times a day for 8-12 weeks (you should take into account the iodine susceptibility of the patient's body).
During treatment with sodium nucleinate, minor side effects may occur in the form of epigastric pain, dyspepsia. Such phenomena completely disappear upon completion of the drug.
Potassium iodide is contraindicated in case of hypersensitivity to iodine, pregnancy, pyoderma.
Blockade with novocaine is performed once every 3 days, with a course of 10 blockades. Do intramuscular injections of Pyrogenal (a course of 25 injections, once every three days), subcutaneous injections of 0.5% Galantamine (a course of 30 injections of 1 ml).
Patients with narrowing of the ducts are prescribed preparations of proteolytic enzymes (Chymotrypsin, Trypsin), as well as injection of Ribonuclease 10 mg / m in combination with deoxyribonuclease electrophoresis (up to 10 procedures for 20 minutes).
Galvanization in chronic sialadenitis is indicated in the form of daily procedures for 4 weeks, in combination with radiotherapy.
Surgical treatment is practiced infrequently, only in the absence of the effect of drug therapy, as well as with regular relapses of the inflammatory disease (more than ten times a year), accompanied by a purulent process, severe functional disorders, strictures and atresia. According to the indications, the method of flow bougienage, total plastic surgery of the mouth, glandular resection with the preservation of the branches of the facial nerve, and blocking of the parotid canal are used.
Antibiotics
Antibiotic therapy is appropriate for bacterial sialadenitis and depends on the severity of the infectious process. [8]
The drugs of choice are often protected penicillin antibiotics and cephalosporins that inhibit the activity of β-lactamase:
|
Amoxiclav |
The preparation of amoxicillin and clavulanic acid is prescribed to adults orally at a daily dosage of 1500 mg (divided into two doses). Side effects in the form of nausea or diarrhea are mild and pass quickly. To prevent these reactions, the drug is recommended to be taken with food. |
|
Sulbactomax |
Sulbactam and ceftriaxone preparation for intramuscular injections. Daily dosage - 1-2 g, administration - every 24 hours. The duration of therapy is determined by the doctor. Possible side effects are more typical for long-term use. We are talking about candidiasis, mycosis, secondary fungal infections, enterocolitis, dyspepsia. |
|
Piperacillin-Tazobactam |
A combined antibacterial drug that is administered to patients in the form of intravenous infusions every 8 hours for 4.5 g. The daily dose can be changed by the doctor depending on the severity of the infection. Possible side effects: diarrhea, nausea, vomiting, skin rashes. |
If gram-negative microorganisms are detected, fluoroquinolone preparations are prescribed. In difficult cases, combined therapy is used - for example, Carbapenem, Metronidazole and Vancomycin.
Physiotherapy treatment
At the initial stage of the inflammatory process at elevated body temperature, physiotherapy is not used. The patient is recommended to drink alkaline mineral waters (such as Borjomi) against the background of drug treatment. From about 3-4 days, it is possible to use UHF therapy in a non-thermal dose, electrophoresis of anti-inflammatory drugs.
Further, for the treatment of acute sialadenitis, the doctor may prescribe:
- Ultraviolet irradiation of the affected area begins with two biodoses, then increases by 1 biodose, bringing up to 6 biodoses. Procedures are performed every two days.
- Fluctuorization on the infiltrate zone is carried out in sessions of 8-10 minutes. The course of therapy includes 10 sessions.
- After eliminating the signs of an acute inflammatory process, in order to accelerate the resorption of the infiltrate, the following are used:
- Infrared irradiation in sessions of 20 minutes, a course of 10-12 sessions.
- Ultrasound therapy with an intensity of 0.05-0.2 W / cm², up to 5 minutes, a course of 10 sessions.
- Electrophoresis 3% potassium iodide, lasting 20 minutes, a course of 10-12 sessions.
To alleviate the pain syndrome, laser therapy is recommended for a duration of 2-3 minutes, a course of 8 to 10 sessions.
Salivary gland massage for sialadenitis
Intraoral (intrabuccal) massage improves blood and lymph flow, stimulates bioactive points, improves the function of the salivary gland. The procedure is carried out in several stages, including general warming up of soft tissues, work with the salivary glands and muscles, and impact on the exit points of the cranial nerves.
Massage movements such as stroking, point pressure, and myoextensive kneading are used. The procedure is carried out with clean hands, you can use sterile surgical gloves.
The salivary glands are massaged with gentle movements, starting from the periphery to the area of the excretory ducts.
After the session, the patient should rinse the mouth with an antiseptic solution.
Massage is performed not only to improve trophism in the tissues of the gland, but also to assess the amount of saliva, its color, consistency, taste characteristics.
Herbal treatment
Alternative methods of treatment are allowed to be used only at an early stage of the development of sialadenitis, or only for the prevention of this disease. To alleviate symptoms, doctors recommend drinking plenty of fluids against the background of drug therapy, including infusions and decoctions of herbs that have anti-inflammatory activity.
- Peppermint tea stimulates the secretion of saliva, relieves pain, refreshes, eliminates an unpleasant aftertaste in the mouth.
- Infusion of chamomile officinalis has anti-inflammatory and anti-edematous action.
- Raspberry leaf tea accelerates wound healing, demonstrates an anti-inflammatory effect.
For daily rinsing of the mouth, you can use infusions of the following herbal preparations:
- raspberry leaves, immortelle flowers, horsetail;
- peppermint leaves, plantain arrows, elder flowers;
- chamomile flowers, eucalyptus and sage leaves.
A good effect is given by rinsing with coniferous water. To prepare the product, boil 0.5 liters of water, add 2 tbsp. L. (with a slide) coniferous needles (spruce or pine), cover with a lid, stand until completely cooled, filter. Use for rinsing 2-3 times a day, or after each meal.
You should not self-medicate if the disease is manifested by severe pain, stone formation, suppuration.
Surgery
In some cases, drug treatment does not allow to achieve elimination of sialadenitis. In such situations, the help of a surgeon may be required.
Obstruction of the excretory duct of the salivary gland requires surgical intervention. Under local anesthesia, the doctor removes the cause of the blockage, performs antiseptic treatment. In the postoperative period, antibacterial and symptomatic therapy is prescribed, and if necessary, bougienage of the excretory canal is additionally performed with its subsequent washing.
Chronic sialadenitis is characterized by frequent recurrence, which over time can lead to complete or partial sclerosis of the gland tissue and the formation of connective tissue structures. If this happens, then the affected gland is removed.
With sialadenitis, it is preferable to perform endoscopic minimally invasive procedures. To date, surgeons have special elastic endoscopes, with which they manage to penetrate into the smallest glandular canals. During endoscopy, the doctor can fully examine the duct, take biomaterial for research, fragment and remove the cause of obstruction.
In the case of sialolithiasis, it is necessary to remove the salivary gland stone using interventional sialendoscopy or direct surgical removal. [9], [10]
Several types of minimally invasive therapies have been proposed for the treatment of salivary gland stones, including interventional sialendoscopy (iSGE), extracorporeal shock wave lithotripsy (ESWL) [11] , and combined endoscopic surgical procedures. [12] The selection of the correct treatment should include criteria such as the affected gland, the number and size of the stones, and the location and relationship to the duct. The least damaging method is always the preferred method of treatment. [13]
Postoperative complications such as pain, scarring, and nerve damage often occur. In operated patients, disorders such as xerostomia (up to 31%), taste changes (16.3%), hematomas (up to 14%), damage to the facial nerve (8%) and damage to the lingual nerve (12%) were observed. [14]. [15]. [16]. [17]
Prevention
Preventive measures to prevent the development of sialadenitis are not specific. The essence of prevention lies in a full, high-quality and balanced diet, a healthy and active lifestyle, and the eradication of bad habits. Compliance with such simple but important rules reduces the likelihood of many pathologies.
The appearance of sialadenitis can be directly related to other diseases of the oral cavity and ENT organs. Violation of the ratio of microflora in the mouth, the ingress of pathogenic microorganisms with blood or lymph can provoke the development of an inflammatory process. Almost any chronic infectious and inflammatory focus can be considered as a predisposition to the appearance of sialadenitis. Moreover, any infectious diseases negatively affect the body's immune defenses as a whole. Therefore, for the prevention of many diseases, it is important to support the immune system in every possible way, treat all diseases (including chronic ones) in a timely manner, exclude hypothermia and stress, and take additional multivitamin preparations recommended by the attending physician in the winter-spring period.
Other mandatory preventive measures:
- regular hygiene procedures, high-quality cleaning of the oral cavity and teeth;
- refusal to eat rough foods that can damage the oral mucosa;
- to give up smoking;
- strengthening the immune defense;
- choosing the right toothbrush and oral care products.
If, however, there are violations, such as dryness of the oral mucosa, swelling, pain in the area of the salivary glands, then you need to visit a doctor without delay. Timely medical care will help prevent the development of inflammation and prevent the occurrence of adverse effects.
Forecast
Acute sialadenitis in the vast majority of patients ends in recovery. However, lethal cases are also described: this can happen if a purulent-necrotic process develops in the gland, as well as when the pathology spreads to the nervous system.
The prognosis of chronic disease is relatively favorable. In this situation, the concept of "conditional" recovery is used: it is used if the patient's remission period lasts more than three years.
Patients are observed for several years, exacerbations are prevented, which usually occur 1-2 times a year, more often in cold weather. Due to properly prescribed therapy, a long remission can occur. In some cases, the formation of a salivary stone in the glandular canal is noted.
Subject to the normal state of immunity, oral hygiene, treatment of comorbidities and elimination of existing infectious foci, sialadenitis completely disappears within 14 days.

