Temporal epilepsy in adults and children
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Among the numerous varieties of epilepsy - a chronic CNS disorder with a paroxysmal manifestation of symptoms - temporal epilepsy is distinguished in which epileptogenic zones or areas of local attachment of epileptic activity are found in the temporal lobes of the brain.
Temporal epilepsy and genius: reality or fiction?
The fact that temporal epilepsy and the ingenious mind are somehow interrelated does not have strictly scientific justifications. Only certain facts are known and their coincidence ...
Some researchers explain the visions and voices that Jeanne d'Arc saw and heard in her epilepsy, although her contemporaries had not noticed strangeness in her behavior for 20 years, except that she managed to reverse the course of the history of France.
But a similar diagnosis of Frederic Chopin, who, as we know, had serious health problems, is being pushed by his visual hallucinations. His genius composer perfectly remembered and described his correspondence with his friends.
He suffered from epilepsy and the Dutch painter Vincent van Gogh, and at the end of 1888 - at the age of 35 and already with a severed ear - he went to a psychiatric hospital where he was diagnosed with temporal epilepsy. After that he lived only two years, having decided on a suicide.
Seizures of epilepsy of the temporal lobes in childhood were in Alfred Nobel, Gustav Flaubert, and, of course, in F.M. Dostoevsky, in whose works many heroes were epileptics, beginning with Prince Myshkin.
Epidemiology
Information on the prevalence of temporal lobe epilepsy, unfortunately, is absent, because to confirm the diagnosis, you need to see a doctor and pre-visualize the brain with an appropriate examination.
Although, according to the statistics of specialized clinics, among focal (partial or focal) epilepsy, the temporal is diagnosed more often than other types of this disease.
About half of all patients are children, because this type of chronic psychoneurological disorder is usually diagnosed in childhood or adolescence.
Causes of the temporal epilepsy
Clinically proven and scientifically proven causes of temporal epilepsy correlate with structural lesions in the temporal lobes of the brain (Lobus temporalis).
First of all, this refers to the most common type of neuropathological damage - hippocampal sclerosis or mesial temporal sclerosis, in which loss of neurons occurs in certain structures of the hippocampus, which controls the processing of information and forms episodic and long-term memory.
The newest studies using MRI imaging showed that temporal epilepsy in children in 37-40 cases is associated with mesial temporal sclerosis. Having the same etiology of temporal epilepsy in adults, it is noted in approximately 65% of patients.
In addition, this type of epilepsy can provoke the dispersion of a layer of granular cells in the dentate gyrus of the hippocampus (Gyrus dentatus), which is associated with a decrease in the production of reelin, a protein that ensures the compactness of these cells, regulating the migration of neurons during embryonic development of the brain and subsequent neurogenesis.
Often, the cause of epileptic activity of the temporal lobes are cerebral cavernous malformations, in particular, cavernous angioma or angioma of the brain - a congenital benign tumor formed by abnormally dilated blood vessels. Because of it, not only the blood circulation of brain cells is violated, but also the passage of nerve impulses. According to some reports, the prevalence of this pathology is 0.5% of the population, in children it is 0.2-0.6%. In 17% of cases, tumors are multiple; in 10-12% of cases they are in the genus, which, perhaps, is responsible for family temporal epilepsy.
Sometimes damage to the structure of Lobus temporalis is caused by a heterotopy of gray matter - a type of cortical dysplasia (a violation of the localization of neurons), which is congenital and can be either a chromosomal abnormality or the result of exposure to embryos of toxins.
Risk factors
Neurophysiologists see the main risk factors for the appearance of functional disturbances in the temporal lobe of the brain in the presence of congenital anomalies and brain injuries affecting babies during labor (including asphyxia and hypoxia) that affect neuronal function.
In both adults and children, the risk of developing secondary temporal epilepsy increases craniocerebral trauma, infectious brain damage in meningitis or encephalitis, and parasitic infestations (Toxoplasma gondii, Taenia solium), as well as cerebral neoplasms of various origins.
Among the toxins that adversely affect the fetal brain, unconditional "leadership" is held by alcohol: a future child whose father abuses alcohol, there is a deficiency of gamma-aminobutyric acid (GABA), the endogenous neurotransmitter of the central nervous system, which inhibits excessive brain stimulation and provides a balance of adrenaline and monoamine neurotransmitters.
Pathogenesis
Millions of neurons that control all the functions of the body continuously change electric charge on their membranes and send receptors nerve impulses - action potentials. Synchronized transmission of these bioelectric signals through nerve fibers and is a brain electrical activity.
In violation of its synchronization and the appearance of local zones with abnormally high - paroxysmal - activity of neurons, the pathogenesis of temporal epilepsy lies. Considering this disease, it should be borne in mind that attacks of electrical hyperactivity are initiated by several zones in the temporal lobes, namely:
- hippocampus and amygdala (amygdala), located in the medial temporal lobe and entering the limbic system of the brain;
- centers of the vestibular analyzer (located closer to the parietal lobe);
- the center of the auditory analyzer (Hirschl's convolution), with anomalous activation of which auditory hallucinations appear;
- the Wernicke area (near the upper temporal gyrus), responsible for understanding speech;
- poles of temporal lobes, when overexcited, self-consciousness changes and the perception of the environment is distorted.
Thus, in the presence of hippocampal or mesial temporal sclerosis, a part of the pyramidal neurons in the fields CA (cornu ammonis) and the subiculum region are lost, which receive the action potential for the transmission of nerve impulses further. Violation of the structural organization of cells in this part of the temporal lobe leads to the expansion of extracellular space, anomalous diffusion of the fluid and the growth of neuroglycerous cells (astrocytes), as a result of which the dynamics of synaptic impulse transmission changes.
In addition, it turned out that disabling the control of the rate of transfer of action potentials to target cells may depend on the lack of hippocampal and neocortical structures of fast-growing interneurons-the multipolar GABAergic insertion neurons needed to create inhibitory synapses. Also, studies of biochemical mechanisms of epilepsy have led to the conclusion that two more types of neurons are present in the hippocampus, subiculum and neocortex: temporal (stellate) non-pyramidal and pyramidal interneurons and smooth non-pyramidal neurons to the pathogenesis of temporal epilepsy. Striatal interneurons are excitatory - cholinergic, and smooth - GABAergic, that is, inhibitory. It is believed that with their genetically determined imbalance, both idiopathic temporal epilepsy in children and predisposition to its development can be associated.
A dispersion or damage to granular cells in the dentate gyrus of the hippocampus entails a pathological change in the density of the dendritic layer. Because of the loss of the cells of the neuron outgrowth, synaptic reorganization begins: the axons and mossy fibers grow to connect with other dendrites, which increases the exciting postsynaptic potential and causes hyperexcitability of the neurons.
Symptoms of the temporal epilepsy
Doctors-epileptologists call the first signs of sudden attacks of aura, which, in fact, is a harbinger of the subsequent short-term focal paroxysm (from the Greek - excitement, irritation). However, not all patients have auras, many simply do not remember them, and in some cases everything is limited by the first signs (which is considered a small partial attack).
Among the first signs of the approaching attack is the appearance of an unjustified feeling of fear and anxiety, which is explained by a sharp increase in the electrical activity of the hippocampus and amygdala (entering the emotive limbic system of the brain).
Attacks of temporal epilepsy often refer to the category of simple partial, that is, not accompanied by loss of consciousness, and usually manifest no more than two or three minutes only abnormal sensations:
- mnesticheskimi (for example, a sense of what is happening, as has happened before, as well as a short-term "failure" of memory);
- sensory hallucinations - auditory, visual, olfactory and taste;
- visual distortions in the size of objects, distances, parts of their bodies (macro and microposs);
- unilateral paresthesias (tingling and numbness);
- weakened reaction to others - a stagnant absent look, a loss of sense of reality and a short dissociative disorder.
Motor (motor) paroxysms or automatisms can include: one-sided rhythmic contraction of the muscles of the face or body; repeated swallowing or chewing movements, smacking lips, licking lips; imperative head or eye movement; small stereotyped hand movements.
Vegetative-visceral symptoms of temporal epilepsy are manifested by nausea, excessive sweating, rapid breathing and palpitations, as well as uncomfortable sensations in the stomach and abdominal cavity.
Patients with this type of disease can have complex partial seizures - if the electrical activity of neurons in other cerebral regions increases dramatically. Then, against a background of complete disorientation, all the above symptoms are accompanied by a disorder of coordination of movements and transient aphasia (loss of the ability to speak or understand the speech of others). In extreme cases, what starts as an attack of temporal epilepsy leads to the development of a generalized tonic-clonic seizure - with convulsions and loss of consciousness.
After the cessation of the attack, during the postictal period, the patients are inhibited, feel brief confusion, do not realize and most often can not remember what happened to them.
Read also - Symptoms of affecting temporal lobes
Forms
Among the problems of modern epileptology, which numbers more than four dozen types of this disease, their terminological designation remains relevant.
The definition of temporal epilepsy was included in the International Classification of Epilepsy ILAE (International Antiepileptic League) in 1989 - in the group of symptomatic epilepsy.
In some sources, temporal epilepsy is divided into posterovemporal lateral and hippocampal-amygdal (or neocortical). In others, such species (types) are classified as amygdala, opercular, hippocampal and lateral posterior-temporal.
According to Russian specialists, secondary or symptomatic temporal lobe epilepsy can be diagnosed when its cause is clearly established. In order to unify the terminology, ILAE experts (in the classification revised in 2010) suggested removing the term "symptomatic" and leaving the definition - focal temporal epilepsy, that is, focal epilepsy, in the sense that it is precisely known which part of the brain causes damage to the brain.
The last variant of the international classification (2017) recognizes two main types of temporal epilepsy:
- mesial temporal epilepsy with local attachment of foci of epileptic activity to the hippocampus, its dentate gyrus and amygdala (i.e., to the zones located in the middle part of the temporal lobe); previously it was called focal symptomatic epilepsy.
- lateral temporal epilepsy (a more rare type that occurs in the neocortex on the lateral surface of the temporal lobe). Attacks of lateral temporal epilepsy are accompanied by auditory or visual hallucinations.
Cryptogenic temporal epilepsy (from the Greek - "cache") implies attacks of unknown or unknown origin during the survey. Although doctors in such cases use the term "idiopathic", and most often such diseases have a genetically determined etiology, the detection of which causes difficulties.
The classification does not include partial temporal epilepsy, that is, limited (partial) or focal, and a term such as focal temporal epilepsy is used. And partial focal seizures or attacks of temporal epilepsy are called partial, reflecting aberrations of brain electrical activity.
With simultaneous disorders in other structures of the brain adjacent to temporal lobes, temporal parietal epilepsy or frontotemporal epilepsy (frontal-temporal) can be defined, although in domestic clinical practice this combination is often called multifocal epilepsy.
Complications and consequences
Periodically repeated manifestations of functional disorders of the temporal lobe of the brain have certain consequences and complications.
In people with this type of epilepsy, there is an unstable emotional state and a predisposition to the development of depression is increased. Over time, repeated seizures can lead to deeper damage to the pyramidal neurons of the hippocampus and the dentate gyrus, which entails learning and memory problems. If these lesions are located in the left lobe, the common memory suffers (forgetfulness and slowing of thinking appear), in the right one - only the visual memory.
Diagnostics of the temporal epilepsy
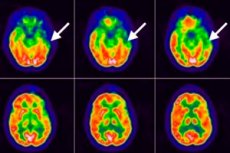
Surveying patients does little to help diagnose this disease, the doctor is left to listen to their complaints and description of the sensations, and then be sure to be sent to a survey in which instrumental diagnostics is performed using:
- Electroencephalography (EEG), which determines electrical activity of the brain;
- MRI of the brain;
- PET of the brain (positron emission tomography);
- polysomnography.
Differential diagnosis
Differential diagnosis presupposes the delimitation of conditions with similar symptoms, including panic attacks, psychotic disorders, crisis manifestations of vegetative-vascular dystonia, transient ischemic attack (microinsult), multiple sclerosis, tardive dyskinesia, occipital epilepsy.
More information in the material - Epilepsy - Diagnosis
Who to contact?
Treatment of the temporal epilepsy
It is customary to treat temporal epilepsy with anticonvulsants, although many of them are now called antiepileptic, since not all seizures are accompanied by convulsions.
Almost all antiepileptic drugs work by reducing the excitability of neurons due to the effect on sodium and calcium presynaptic channels or enhancing the inhibitory effects of neurotransmitters, primarily GABA.
The most commonly used medicines of the older generation are: Phenytoin, carbamazepine, valproic acid preparations (Apelexin, Convoolex, Valprokom), Phenobarbital. More information - Tablets from epilepsy
Now more often refer to more new antiepileptic drugs, which include:
- Lamotrigine (other trade names - Latrigine, Lamitril, Convulsan, Seizar) is a dichlorophenyl derivative, can be used in children over two years of age; contraindicated in case of liver failure and pregnancy. Possible side effects include: skin reactions (up to necrosis of the skin), severe headaches, diplopia, nausea, bowel disturbances, decreased platelets in the blood, sleep disturbances and increased irritability.
- Gabapentin (synonyms - Gabalept, Gabantin, Gabagama, Neuralgin, Tebantin) - an analogue of gamma-aminobutyric acid.
- Lacosamide (Wimpat) is used after 16 years in doses determined by a doctor. The list of side effects of this drug indicates: dizziness and headache; nausea and vomiting; tremor and muscle spasms; sleep, memory and coordination of movements; depressive state and mental disorders.
In partial seizures, seizures in adults and children older than six years are prescribed Zonisamide (Zonegran), among which frequent side effects are noted: dizziness and rashes on the skin; decreased appetite and memory; impairment of sight, speech, coordination of movements and sleep; depression and the formation of kidney stones.
Antiepileptic drug Levetiracetam and its generics Levetinol, Comviron, Zenicetam and Keppra for temporal epilepsy are prescribed for patients over 16 years old with tonic-clonic seizures. They contain pyrrolidine-acetamide (lactam gamma-aminobutyric acid), the active GABA receptors. Since Keppra is available as a solution, it is administered by infusion in an individually determined dosage. Its synonym for levetiracetam is a tablet for oral administration (250-500 mg twice a day). The use of this drug, like many of the above, may be accompanied by general weakness, dizziness, increased drowsiness.
In addition, it is necessary to take magnesium preparations and vitamins such as B-6 (pyridoxine), vitamin E (tocopherol), vitamins H (biotin) and vitamin D (calciferol).
Apply and physiotherapy treatment (deep stimulation of the brain and vagus nerve) - read the article Epilepsy - Treatment
If temporal epilepsy in children causes seizures, a low-carbohydrate ketogenic diet with a high fat content is recommended. When assigning this diet, a child or adolescent needs to provide adequate nutrition and to control height and weight.
Surgery
According to statistics, up to 30% of patients with mesial temporal lobe epilepsy can not control seizures while taking medications.
For some patients, surgical treatment can be considered - selective amygdalo-hippocampentomy, that is, the removal of the amygdala, the anterior part of the hippocampus, and part of the dentate gyrus.
Such a radical measure is justified only in the presence of sclerosis of the hippocampus, but there is no guarantee of the effectiveness of this operation. Surgical intervention by lobectomy, stereotactic radiosurgery or laser ablation can lead to a significant reduction in cognitive function of the brain.
Alternative treatment
Scientific evidence that herbal therapy helps with some type of epilepsy does not exist. Nevertheless, herbalists are advised to drink decoctions and infusions of the ragwort (Senecio vulgaris), ordinary herb (Hydrocotyle vulgaris) of the Aralia family, soothing tinctures of the Baikal skullcap (Scutellaria baicalensis) or medicinal peony (Paeonia officinalis) roots. But the most valuable plant for the treatment of temporal epilepsy - reducing the frequency of focal paroxysms - is considered to contain gamma-aminobutyric acid mistletoe white (Viscum album).
In addition, the folk treatment of this pathology is the use of fish oil, which contains omega-3 fatty acid (docosahexaenoic acid), which contributes to the improvement of cerebral circulation, and, therefore, nutrition of the brain cells.
Forecast
Pathologies such as mesial temporal sclerosis, cortical dysplasia or swelling, predetermine a prediction about the undecidability of epileptic seizures associated with temporal lobes, and even possible dementia.
Clinical data show that after long-term treatment, complete remission in temporal epilepsy occurs in just over 10% of cases, and in almost 30% of cases there is a persistent improvement in symptoms with the occurrence of seizures caused by stressful situations. However, temporal epilepsy in children - with its manifestation at the age of 9-10 years - approximately to 20 years gives a long-term remission in three cases out of ten.


 [
[