Surgery to remove the fallopian tube: consequences and rehabilitation
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

The frequency of ectomy in gynecology is dominated by the appendages of the uterus, and the removal of the fallopian tube (tubectomy or salpingectomy) is in second place after removal of the ovaries.
For the first time such radical surgical intervention that saved the life of the patient with bleeding during ectopic pregnancy was conducted in 1883 by Scottish surgeon Robert Lawson Tate.
 [1],
[1],
Indications for the procedure
The main indications for the removal of the fallopian tube include the removal of the tube in ectopic pregnancy: when there is bleeding after salpingolotomy (surgery to remove tubal pregnancy with the preservation of the tube); with perforation of the uterine tube due to a violation of pathological pregnancy (tubal abortion); when the size of the fetal egg in the tube is more than 3.5-4 cm; in cases of repeated ectopic pregnancy in the same tube.
If conservative therapy does not give positive results, the removal of the fallopian tubes can be performed in the inflammation of their tissues - salpingitis, and in cases of purulent salpingitis, the fallopian tube where purulent exudate accumulates is removed in most patients, as in the pioalpinx and tubo-ovarian abscess.
Salpingitis can provoke an inflammatory process in the ovary, and then gynecologists diagnose an inflammation of the appendages - adnexitis or salpingo-oophoritis, threatening or ectopic pregnancy, or irreversible, infertility dysfunction of the appendages. And an exit from the situation can be laparotomy or laparoscopic removal of the ovary and the fallopian tube.
With spikes between the ovary and the tube, it is often enough to stretch the tube, and a liquid secreted by the mucous membrane accumulates in this place with the development of a chronic pathology - hydrosalpinx. The fluid often contains pus, and if this cavity is ruptured, the woman is really threatened with peritonitis. In addition, due to hydrosalpinx, obstruction of the fallopian tubes develops , which is one of the most frequent causes of female infertility. The removal of the tube with hydrosalpinks in such situations increases the frequency of pregnancy after in vitro fertilization and reduces the risk of developing pregnancy outside the uterine cavity. Therefore, a protocol was developed for IVF after removing the tubes (both).
By the way, and the removal of adhesions in the fallopian tubes, making women infertile, can be carried out by means of a tubectomy - provided that all other methods of dividing the overgrown fibrous cords have been unsuccessful.
Among the indications for carrying out this operation by laparotomy, tuberculosis of the appendages, myoma of the uterus, ovarian cancer and intraepithelial cancer of the fallopian tubes should be noted.
Removal of the hydatidinum of the fallopian tube - the subserous cyst - is performed in cases of twisting of its pedicle, and removal of the entire tube may be necessary only if the size of these cysts is large and the multiple adhesions localized around them.
In recent years, evidence has been obtained of the relationship between the development of most ovarian serous carcinomas and fallopian tubes. As a result, there were recommendations on the use of preventive salpingectomy (patients with hereditary mutations of BRCA1 and BRCA2 genes) in order to prevent the development of ovarian cancer. According to the International Journal of Obstetrics & Gynaecolog, unilateral tube removal reduces the risk of ovarian cancer in this category of women by 29%, and the removal of both fallopian tubes by 65%.
Technique of the removal of the fallopian tube
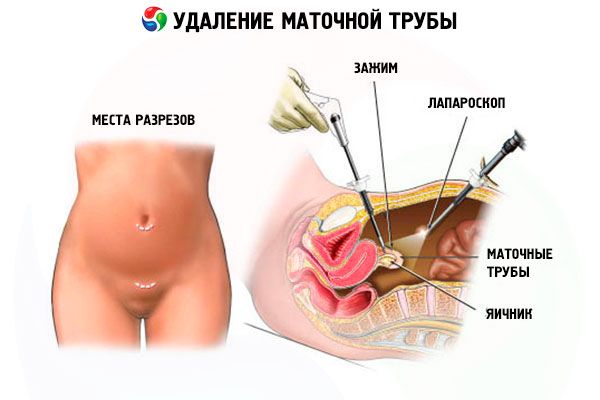
Many sources describe the technique of removing the uterine tube in a laparoscopic way.
This operation is performed under general anesthesia, and with contraindications to endotracheal anesthesia, regional epidural anesthesia is used.
In the outer wall of the abdominal cavity - around the navel, above the pubis and at the bottom (from the side opposite to the tube being removed) - three punctures (apertures) are made to install the trocars, through which the surgeon will introduce the necessary laparoscopic instruments and the actual endoscope on the monitor). To provide space for manipulation in the abdominal cavity, carbon dioxide or oxygen (this is called superimposing pneumoperitoneum) is injected, and the blood is removed by aspiration.
On the operating table, the operated patient lies on the back, but after sucking the blood, the lower part of the body, in particular, the pelvis is raised by 45 °, giving the so-called Trendelenburg position optimal for surgical intervention on the pelvic organs. The tube that is to be excised is clamped as close as possible to the cut-off site (near the connection with the uterus), stretched and cut off by a bipolar coagulator, forceps or laparoscopic scissors with simultaneous monopolar coagulation. Then coagulation and clipping of the upper part of the wide uterine ligament (mesosalpinx) and the isthmus of the tube with the application of ligatures is performed. After that the cut off fallopian tube is extracted outside through the largest trocar.
If a tube is removed during an ectopic pregnancy, the upper abdominal cavity is inspected and the entire cavity thoroughly sanitized with antiseptics.
After removing trocar, small seams are applied after removal of the pipe.
Contraindications to the procedure
To date, surgery to remove the fallopian tube is performed either by laparotomy - with access through axial stratified dissection of the abdominal wall (with a cut length up to 12 cm) and an open surgical field, or laparoscopically - through three small incisions using endoscopes inserted into the cavity and electrosurgical instruments. The choice of type of surgery depends on many factors, but the use of laparoscopy - despite its clear advantages in terms of the degree of trauma, complications, postoperative scars and the rate of recovery of patients - has certain medical contraindications.
Contraindicated laparoscopic removal of the uterine tube in the development of peritonitis; in case of rupture of the fallopian tube with large bleeding; in acute conditions of cardiovascular order (stroke, infarction) and circulatory hypoxia; with diagnosed cancer of the appendages or uterus; with obesity of the second-third degree and decompensated diabetes mellitus.
Thus, patients with the listed medical contraindications are laparotomically removed from the uterine tube.
Regardless of the procedure of the operation, preparation for it consists in ultrasound examination of the uterus, fallopian tubes and ovaries (and also all organs located in the pelvic area); general and biochemical blood tests (including platelet levels); blood testing for the presence of viral hepatitis and HIV; electrocardiography (ECG).
Consequences after the procedure
Since recovery of the fallopian tubes after removal is impossible, the main consequence of such surgery is to reduce fertility: with the removal of one tube, the possibility of becoming pregnant is reduced by half, and in the case of bilateral tu- bectomy, the possibility of natural pregnancy is excluded completely, and the only way to give birth to a child is IVF technology.
In addition, if one fallopian tube is left and the second is removed due to an ectopic pregnancy, the risk that the pregnancy will again be ectopic (outside the uterus) is significantly increased.
It should be borne in mind that regular monthly ones after removal of the tube are restored in all patients in different ways, and menstrual irregularity is often noted due to problems with ovulation and ovarian function from the side of the remote tube.
As gynecologists note, the most tangible consequences of removal of the fallopian tube are in women who have suffered the removal of both fallopian tubes. Possible headaches, tachycardia, hot flashes and hyperhidrosis, an increase in the thyroid and mammary glands.
 [7]
[7]
Complications after the procedure
Surgery to remove the fallopian tube can have complications in the form of secondary infection and the development of inflammation, as evidenced by the elevated temperature after removal of the tube.
In the subcutaneous tissue, interstitial hematomas may appear, and as a result of damage to mesenteric vessels and their insufficient coagulation during surgery, concealed intra-abdominal bleeding may occur after removal of the tubes.
Because of anesthesia, patients can vomit, and two or three days there are vomit. And among the complications of pneumoperitoneum surgeons called the accumulation in the tissues of gas (emphysema), hematoma of the abdominal wall, bleeding.
Also for a few days there are minor bleeding after removal of the fallopian tube, especially when it is ruptured due to tubal pregnancy. And this is attributed to the ingress of blood into the uterine cavity during surgery.
Postoperative adhesions after removal of the tube occur not only with laparotomy, but also with laparoscopic method. And often a sign of the formation of adhesions are pain after removal of the tubes, but they can cause and cystic formation of the ovary, disturbed during surgery. As doctors say, over time, spikes in the small pelvis can expand and appear intestinal adhesions, which can adversely affect its patency. In addition, they may be implicated in the fact that women have a lower abdominal pain after removing the tube.
Care after the procedure
The rehabilitation period after tubeccosis can last up to two to three months, although the hospital after the removal of the fallopian tubes is given from the day of admission to the medical institution (the hospital stay usually does not exceed one week) for not more than a month (depending on the cause of the operation, its complexity and the patient's condition).
Typically, a course of antibiotics, subcutaneous injections of an extract of aloe (1 ml per day for two weeks), the use of Longinazai vaginal suppositories (one suppository every three days) is prescribed.
Physiotherapy after removal of the tube includes sessions of electrophoresis with iodine and zinc (standard course - 20 procedures). Moderate physical activity (quiet walking) is mandatory - so as not to form spikes.
Seam care after laparoscopic surgery is to prevent their infection, so the doctor's recommendations after the removal of the fallopian tube: observe the rules of hygiene, but refuse baths and take a shower (closing the seams from water ingress). Also, doctors advise not less than a month after the operation to wear compression underwear.
Also for a month, the sex life stops after removing the tube, and then (after removing one tube) it takes about six months (after the first full-fledged menstruation) to take birth control pills.
Some special diet after removal of the tube is not required, but you must avoid constipation and bloating (flatulence). In this connection it is necessary to temporarily exclude the use of carbonated beverages, legumes, cabbage, dishes from cereals, red meat, fresh yeast bread and baking, sweet fruits, whole milk.
 [11],
[11],

