Medical expert of the article
New publications
Intestinal adhesions
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
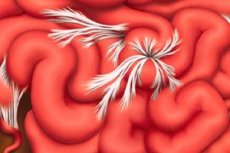
Doctors consider intestinal adhesions to be the result of a pathophysiological process that develops in the abdominal cavity and can either be asymptomatic or manifest itself with a number of signs.
Today, intestinal adhesions after surgery (postoperative peritoneal adhesions) remain a serious clinical problem for both surgeons and patients.
Epidemiology
- intestinal adhesions after surgery on abdominal organs (especially on the small and large intestines) occur in 80-85% of patients;
- after repeated laparotomy, adhesions occur in 93-96% of patients;
- intestinal adhesions after appendicitis are observed one year after appendectomy in 23% of operated patients, and after three years – in 57%;
- adhesions of the intestine and uterus, as well as adhesions of the intestine and ovary occur in 70% of cases of surgical treatment of gynecological pathologies;
- In 10-20% of cases, adhesions are accidentally detected in patients who have not undergone surgery.
Causes intestinal adhesions
The term "adhesions" refers to the process of scar tissue formation between loops of intestine, as well as between individual sections of intestine and the inner lining of the abdominal wall (peritoneal lining). These are small intestinal adhesions and large intestinal adhesions.
Other abdominal and pelvic organs may also be affected: liver, gallbladder, uterus (adhesions of the intestine and uterus), fallopian tubes, ovaries (adhesions of the intestine and ovary), bladder.
The main causes of intestinal adhesions after surgery – including intestinal adhesions after appendicitis (appendectomy) and after cesarean section (surgical method of delivery) – are related to the fact that during abdominal surgical interventions by laparotomy:
- the integrity of the tissues of the peritoneum and internal organs is disrupted;
- the mucous membranes of internal organs lose moisture (it has been proven that drying out tissues during surgery increases the formation of adhesions);
- internal tissues come into contact with foreign substances (instruments, tampons, suture materials, etc.);
- blood or blood clots remain on the tissues inside the abdominal cavity.
Much less often they are a consequence of closed abdominal injuries and inflammatory processes, i.e., they are not associated with abdominal surgery. Thus, chronic intestinal adhesions can form during long-term inflammations in the mesenteric part of the small intestine (enteritis), the cecum and sigmoid colon of the large intestine, as well as during gynecological infections and radiation damage to tissues during radiotherapy of malignant tumors in the abdominal cavity.
Intestinal adhesions in children at an early age may occur due to congenital anomalies of the intestinal structure: atresia of the small intestine, dolichosigma (elongation of the sigmoid colon), coloptosis (incorrect position of the colon), embryonic strands of the large intestine, intussusception of the intestine. Also, intestinal adhesions in children are formed, as in adults, after abdominal surgery in the abdomen or pelvis.
Risk factors
Almost everyone who undergoes laparotomy surgery is at high risk for developing adhesions; and risk factors for intestinal adhesions include problems with the body's fibrinolytic system (the functional opposite of the blood clotting system). Problems with fibrinolysis can be monitored by examining the levels of plasminogen activator inhibitor in the blood, tissue plasminogen activator, and fibrin breakdown products in the peritoneal fluid.
According to surgeons, chronic intestinal adhesions without previous surgery often occur during inflammatory processes against the background of abdominal obesity, that is, excess fatty tissue in the area of the greater omentum (a fold located behind the visceral layer of the peritoneum and covering the intestinal loops). Because the loose connective tissue of the omentum is especially susceptible to the formation of adhesions under the pressure of fatty deposits in the abdominal area.
Pathogenesis
Studies of cellular and humoral mechanisms of adhesion formation have shown that their pathogenesis lies in the disruption of the local balance between fibrin synthesis and its breakdown (fibrinolysis). During strip operations or inflammations, damage to the mesothelial layer of organ tissues and blood vessels occurs, causing a natural protective inflammatory reaction with simultaneous activation of inflammation mediators, the coagulation cascade, and deposition of fibrin, the insoluble basis for blood clot formation, on the damaged area.
As a result, the permeability of blood vessels increases, and damaged tissues secrete a serous-hemorrhagic exudate that supports the healing process. It contains leukocytes, platelets, interleukins, macrophages, blood plasma protein fibrinogen, hyaluronic acid, and proteoglycans. Under normal conditions, fibrin is lysed by tissue plasminogen activators, but during operations, fibrinolytic activity decreases, and excess fibrinogen turns into highly adhesive matrices of fibrin gel that covers the tissues. Fibroblasts begin to grow and fasten together anatomically isolated structures of the abdominal cavity, essentially turning into internal scars - intestinal adhesions in the form of fibrous connections.
Symptoms intestinal adhesions
What are the symptoms of intestinal adhesions? Most abdominal adhesions remain unnoticed, but if the existing pathology manifests itself, its first signs are a feeling of pain.
It should be noted that periodically occurring pains with intestinal adhesions are localized in the abdominal cavity or in the pelvis, depending on the location of the formation of fibrous connections between the intestinal loops and the surrounding anatomical structures.
Painful spasms or nagging pains may become more intense some time after eating and during physical activity. As doctors emphasize, pains from intestinal adhesions often imitate pains from appendicitis, endometriosis or diverticulitis.
Symptoms of intestinal adhesions also include: a feeling of discomfort in the abdominal cavity due to increased formation of intestinal gases (flatulence) and internal pressure on the abdominal wall (in the umbilical region or slightly below), loud rumbling in the abdomen and bloating.
Constipation occurs regularly with intestinal adhesions, which is associated with difficult movement of intestinal contents due to peristalsis disorders. Nausea and even vomiting may occur after eating. If there are chronic intestinal adhesions, then, in addition to the listed symptoms, weight loss is observed.
Despite the gradual increase in fibrinogen levels in pregnant women by the end of the term, new intestinal adhesions do not form during pregnancy. However, existing “internal scars” can make themselves known and create additional problems: from mild abdominal pain (30-45 minutes after eating) to intense pulling and stabbing pains.
Complications and consequences
What is the danger of intestinal adhesions? Adhesions of the small intestine in the abdominal cavity often cause such negative consequences for the functioning of the digestive system that the only solution to the problem can be a repeat operation.
According to gynecologists, adhesions of the intestines and uterus can lead to secondary dysmenorrhea, and adhesions of the intestines and ovaries or intestinal loops with the fallopian tubes can lead to the inability to become pregnant.
The presence of intestinal adhesions significantly complicates any surgical intervention in the abdominal cavity, increasing the risk of bleeding and intestinal perforation.
But the most dangerous complications of peritoneal fibrous adhesion are intestinal obstruction with adhesions, which accounts for over 40% of all cases of obstruction and 60-70% of small intestinal obstructions. The cause of intestinal obstruction in pregnant women in 55% of cases is also intestinal adhesions after surgery performed before pregnancy.
Intestinal adhesions can bend, stretch and rotate individual parts of the intestines so that their lumen is reduced or completely blocked. This causes the development of intestinal obstruction, when the contents of the gastrointestinal tract - partially or completely - stop moving through the corresponding sections of the intestine. Complete intestinal obstruction is an acute, life-threatening condition that requires immediate medical care, including surgery.
Intestinal obstruction with adhesions (or intestinal obstruction) causes severe abdominal pain and spasms, vomiting, constipation and intestinal gas retention, abdominal edema; in acute obstruction, pale skin, cold sweat, a sharp drop in blood pressure and tachycardia are also observed. Local blood supply due to twisting of intestinal loops stops, which can result in tissue necrosis and the development of peritonitis.
Infants with intestinal obstruction have bouts of crying, stretch out their legs and entire body, urinate less often, the skin above the fontanelle is drawn in, and the vomit is green.
Diagnostics intestinal adhesions
Today, only instrumental diagnostics make it possible to identify and establish the location of peritoneal fibrous adhesion.
In this pathology, diagnostic laparoscopy is considered the most informative and objective method.
Gastroenterologists also use: irrigography (X-ray of the intestine with the introduction of barium, can reveal abnormal angulation of intestinal loops); colonoscopy (endoscopic examination of the rectum); electrogastroenterography; ultrasound examination (US) and computed tomography (CT) of the intestine and abdominal organs.
Your doctor may order a complete blood count to rule out the development of inflammation.
 [ 30 ]
[ 30 ]
What do need to examine?
How to examine?
Differential diagnosis
Since abdominal pain, constipation, and other symptoms are nonspecific, differential diagnostics using ultrasound and CT are necessary, which allows excluding other causes of obstruction, such as tumors or intestinal strictures.
Who to contact?
Treatment intestinal adhesions
It should be noted right away that in modern clinical practice, including foreign, treatment of intestinal adhesions - with pronounced symptoms and the problems they cause - is carried out surgically: the drug method cannot yet "tear" the fibrous fibers that connect the intestinal structures. Especially if the adhesions formed a long time ago, and the fibrin strands have become dense and strong.
Surgical treatment for extensive adhesions is performed by laparotomy, i.e. with a fairly large incision in the peritoneum, after which the intestinal adhesions are dissected in the open surgical field. However, there is a high probability (30-40%) that new adhesions will occur after this operation.
In the presence of single adhesions, their dissection is carried out laparoscopically (with the introduction of a special endoscopic device into the abdominal cavity through small incisions). And although laparoscopic surgery is certainly the best option, tissue trauma during dissection of the fibrous cord is also fraught with a relapse of the adhesion process.
Minimally invasive treatment of intestinal adhesions with a laser is also practiced – with a small area of fibrous connection and its clear localization.
Treatment of intestinal adhesions without surgery
Domestic doctors treat intestinal adhesions without surgery using certain drugs that should prevent the conversion of fibrinogen into fibrin or activate the body's fibrinolytic system.
The most commonly used medications are:
- anticoagulant Heparin - is administered immediately after surgery into the subcutaneous fat (5000 IU twice a day); contraindicated in case of bleeding and increased bleeding, kidney or liver problems, leukemia and anemia.
- corticosteroid Hydrocortisone (2.5%) is injected into the abdominal muscle or into the cavity after surgery (100-500 mg) 4 times a day; although recent surgical interventions are listed among the contraindications to the drug (except for severe arterial hypertension, nephritis, osteoporosis, gastric ulcer and diabetes mellitus). Side effects of Hydrocortisone include inflammation of the pancreas, decreased immunity, as well as anaphylactic shock and cardiac arrest.
- The enzyme preparation Hyaluronidase (Lidase), according to the instructions, is used when it is necessary to eliminate joint contracture, remove hematomas and soften scars on the skin.
- Urokinase (fibrinolytic), used by intravenous infusions for thrombophlebitis, pulmonary embolism and other arteriovenous thromboembolism. Standard dose is 1000-2000 IU/kg/hour. Contraindications include bleeding and the risk of bleeding, open wounds, and recent surgeries are listed among relative contraindications.
- The drug Fibrinolysin has the same indications and contraindications as Urokinase, since both drugs act, respectively, on the blood coagulation system and fibrinolysis. Fibrinolysin is usually administered during surgery into the abdominal cavity (often in combination with Heparin).
In addition, for severe pain, such painkillers for intestinal adhesions as Paracetamol, Spazmalgon, No-shpa (1-2 tablets up to three times a day) are used. Vitamins are also prescribed, as a rule, these are tocopherol and folic acid.
Traditionally, treatment of intestinal adhesions without surgery includes physiotherapy treatment - in the form of electrophoresis with various drugs, paraffin applications to the abdominal area, etc. However, the advisability of physiotherapy procedures raises great doubts among many specialists, since they do not lead to the elimination of formed adhesions. For the same reason, you should not massage the intestines for adhesions that arose long before the symptoms of the pathology appeared.
Traditional medicine and homeopathy
Among the alternative methods, the most acceptable from a medical point of view is folk treatment using leeches, whose saliva contains the anticoagulant hirudin.
Of course, the advice to use olive oil for colon adhesions is also useful, since the unsaturated omega acids of this oil have a beneficial effect on the mucous membranes of the gastrointestinal tract. In addition, olive oil (which can be replaced with almost any other) prevents the formation of so-called fecal stones, which significantly complicate the process of defecation in case of colon adhesions.
But traditional healers recommend using castor oil externally - in the form of warm compresses on the stomach. They say that this oil is especially helpful for women with intestinal and uterine adhesions, as well as intestinal and ovarian adhesions. Obtained from castor oil plant seeds (Ricinus L.), castor oil contains ricinoleic acid, which is easily absorbed into the body through the skin, stimulates lymphatic drainage and enhances the removal of tissue metabolic products.
As a multifunctional symptomatic remedy, it is recommended to take an alcohol tincture of juniper bark. To prepare it, 50 g of dry bark is poured with 150 ml of vodka and infused for 20 days. The tincture should be taken 25-30 drops twice a day (before meals).
You can try herbal treatment, for example, to relieve intestinal spasms, use a decoction of chamomile flowers, crushed calamus root and peppermint leaves (in a ratio of 2:1:1) - a tablespoon of the mixture per 200 ml of water. Take a few sips three times a day.
It is recommended to prepare and take half a glass twice a day (half an hour before meals) a decoction of meadow red clover flowers, St. John's wort, peony roots, and meadowsweet bark (meadowsweet or larkspur). The decoctions are prepared at the rate of one tablespoon of raw materials per 250 ml of water. You can also prepare an aqueous infusion of safflower (Carthamus tinctorius).
Homeopathy can offer the following preparations for the treatment of intestinal adhesions: Aconitum napellus C6 (in granules), drops based on the seeds of the larkspur Staphysagria, Arnica montana (granules C3, C6), drops with an extract of the daisy Bellis perennis. The dosage is determined by a homeopathic doctor on an individual basis.
How is mustard used for intestinal adhesions? In the composition of the liquid homeopathic remedy Thiosin Aminum, which is made from mustard seed oil, containing a whole complex of biologically active substances, including polyunsaturated fatty acids, vitamins A, D, B3, B4, B6, E, etc.
 [ 31 ], [ 32 ], [ 33 ], [ 34 ]
[ 31 ], [ 32 ], [ 33 ], [ 34 ]
Diet for intestinal adhesions
Digestive problems and diet for intestinal adhesions are one of the biggest difficulties with this pathology, because in some cases food is simply not digested normally. Therefore, it is recommended to eat only moderately warm soft food. At the same time, you need to eat more often, but in small portions. Overeating is strictly contraindicated!
 [ 35 ]
[ 35 ]
What foods should not be consumed if you have intestinal adhesions?
Foods with a high content of fiber and plant fibers should be excluded from the diet so that they do not overload the intestines and increase the formation of intestinal gases (and, along with them, pain). So, bread consumption is reduced to 150 g per day, fresh vegetables and fruits can only be looked at, and porridges for intestinal adhesions, especially during periods of intense manifestation of symptoms, will have to be very strongly boiled and made semi-liquid. Read more - Diet for flatulence
Dietitians consider whole milk, all fatty, spicy, canned and fried foods to be undesirable products. You should drink enough water (non-carbonated), fresh kefir and green tea are very useful - for adhesions of the large intestine.
Although such a diet for intestinal adhesions does not meet the body's needs for nutrients, it can reduce abdominal pain while treatment is underway.
What can you eat with intestinal adhesions? Dietary recommendations
Includes soups with low-fat broth and cream soups, lean fish and chicken (boiled or steamed), soft-boiled eggs and omelettes, all fermented milk products (including cheese and cottage cheese).
Restrictions and recommendations on products may vary depending on the nature of intestinal complications, so even an approximate menu for intestinal adhesions should be made taking into account the individual characteristics of each patient.
Gymnastics for intestinal adhesions
Therapeutic exercises for intestinal adhesions are designed to provide both a sufficient (but not excessive) level of physical activity and targeted dynamic impact on the problem area – the abdominal cavity.
The most useful exercises for intestinal adhesions should activate local blood supply to intestinal tissues, strengthen the abdominal wall and increase the elasticity of internal muscle fibers.
All exercises should be performed slowly, each 8-10 times, and preferably while lying on your back on a hard surface.
- Simultaneous bending of the legs at the knees followed by straightening to the starting position.
- After the legs have been bent, placing both hands behind the head, we lift the shoulder blades (the abdominal press is tense); then we take the starting position (legs straight, arms along the body).
- With bent knees, lift your lower back and pelvis off the floor and hold in this position for a count of 1-2-3 (support on your feet and shoulder blades, arms extended along your body).
- Simultaneous bending of the legs at the knees, followed by tilting them first to the right and then to the left (without lifting the back and lower back off the floor).
- The famous “bicycle” is done with maximum amplitude of the shins towards the abdominal wall and chest.
- Alternately bend your legs (lifting them off the floor) and touch the knee with the opposite elbow, with a slight turn of the body towards the leg bent at the knee.
Yoga for intestinal adhesions consists mainly of the well-known "belly breathing". It is better to do the exercise standing. First, you need to place your right palm on the chest area, and your left palm on the stomach, below the navel. Take a deep breath through the nose, first filling the lower part of the lungs with air (the abdominal wall should rise and tense, and this is visible in the left palm, which also rises). It is very important that the palm lying on the chest remains motionless during inhalation.
Having filled the stomach with air to the limit, you should exhale it very slowly through the nose and literally "squeeze" it out of yourself, pulling the abdominal wall as deep as possible inward (towards the back). During such breathing, a natural self-massage of the intestinal structures located directly behind the peritoneum occurs. But such an exercise is contraindicated in case of heart rhythm disorders.
Prevention
Intestinal adhesions are difficult to prevent, but modern surgical technologies make it possible to reduce the risk of their occurrence using unique materials – biodegradable (do not require removal) films that protect abdominal tissue from peritoneal fibrous adhesion.
Today, during operations performed laparotomy (with large scalpel incisions and an extensive surgical area), intestinal adhesions can be prevented using the adhesive barriers Hyalobarrier, PrevAdh, Intercoat, Evicel, Surgiwrap, CoSeal, Seprafilm.
Forecast

