Medical expert of the article
New publications
Vestibular ataxia
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Impaired motor coordination and inability to maintain body position are often associated with pathology of the vestibular system at one level or another. Vestibular ataxia reveals itself by the patient's instability in standing or sitting, and especially during walking. The problem is also manifested by systemic vertigo, nystagmus. The patient is often bothered by nausea (sometimes - up to vomiting), autonomic disorders. Additionally, there are symptoms of the root cause of the development of vestibular ataxia, to which the main therapeutic measures are directed. [1]
Vestibular ataxia syndrome.
The spatial orientation of the body in the human body is maintained thanks to the vestibular analyzer, which is responsible for assessing the position and motor actions of the trunk and limbs, and helps interpret the force of gravity. The vestibular system reacts to any change in body position thanks to special hair cells localized in the labyrinthine mechanism of the inner ear. From these structures, nerve vibrations pass through the vestibular nerve: it and the auditory nerve are part of the eighth pair of cranial nerves. Further signals go to the vestibular nuclei of the medulla oblongata. There the information is synthesized, a response is formed, providing further control of motor activity. From the vestibular nuclei regulatory nerve oscillations are transported to numerous parts of the central nervous system, including cerebellum, autonomic nervous system, reticular formation, spinal structures, cerebral cortex, oculomotor nuclei. Thanks to this, there is a distribution of muscle tone and reflex response to maintain balance. If one or another stage of this pathway is affected, vestibular ataxia may develop. The causes of such a disorder are different. [2], [3]
Ataxia can also be divided into sporadic (patients have no family history of ataxia and manifest in adulthood), hereditary (caused by a gene defect and manifest in childhood), and acquired (due to structural or demyelinating conditions, toxicity, paraneoplastic, inflammatory diseases). Or infections and autoimmune conditions). Or infections and autoimmune conditions). [4]
Epidemiology
The term "ataxia" translates from Greek as "devoid of purpose". It is used to define disorganized, uncoordinated motor activity, unrelated to paresis, muscle tone disorders, or violent movements.
Vestibular ataxia is most often manifested by disorders of balance retention, impaired walking, and improper motor coordination.
There are no clear statistics on ataxia, as it is not an independent nosological unit, but only a syndrome, or symptom complex.
The most common symptom of vestibular ataxia is systemic vertigo. It is this manifestation that most often becomes the reason for referral to neurologists (about 10% of cases) and otolaryngologists (about 4% of cases).
Vestibular ataxia is considered the most common cause of falls and increased injury in the elderly and seniors.
The overall prevalence of ataxia is 26 cases per 100,000 children. The overall prevalence of hereditary ataxias is 10 cases per 100,000 people. [5] Dominant cerebellar ataxia occurs in 2.7 cases per 100,000 people and recessive hereditary cerebellar ataxia in 3.3 cases per 100,000 people. [6] The increased prevalence is seen in countries where consanguinity is common. [7] The worldwide prevalence of spinocerebellar ataxia ranges from 3 to 5.6 cases per 100,000 people. [8] The most common spinocerebellar ataxia is spinocerebellar ataxia type 3. [9]
Causes of the vestibular ataxia
The development of vestibular ataxia is caused by damage to any of the stages of the vestibular analyzer. In most cases, hair cells are affected - for example, in the process of such an inflammatory reaction as labyrinthitis, which occurs due to trauma, spread of infection from the middle ear region. The latter often occurs in patients with acute otitis media, purulent otitis media, aeritis. Hair cells may die against the background of tumor invasion or intoxication in auricular cholesteatoma. Recurrent vestibular ataxia is characteristic of meniere's disease.
In some cases, vestibular ataxia occurs when the vestibular nerve is affected. Such a disorder may have infectious, toxic (ototoxic), tumor etiology. Often due to viral infection (herpes, influenza, acute respiratory viral infections) vestibular neuronitis develops.
Ataxia sometimes results from damage to the vestibular nuclei localized in the medulla oblongata - for example, this is characteristic of compression of the medulla oblongata in craniovertebral anomalies (platybasia, Chiari anomaly, atlanto-assimilation), tumor processes in the brain stem, encephalitis, arachnoiditis of the posterior fossa, demyelinating pathologies (encephalomyelitis, multiple sclerosis ).
Vestibular ataxia can be one of the signs of chronic ischemic processes in the brain stem, which, in turn, is caused by a disorder of vertebrobasilar blood flow in vertebral artery syndrome, atherosclerosis, hypertension, cerebral vascular aneurysm. The development of ataxia is also characteristic of transient ischemic attack, hemorrhagic or ischemic stroke.
Vestibular ataxia is a common consequence of craniocerebral trauma due to the direct effect of the injury on the nuclei and endings of the vestibular nerve, or concomitant circulatory disorders (in particular, we can talk about vascular post-traumatic spasm). [10]
Risk factors
Vestibular ataxia often develops in people with encephalitis, acute encephalomyelitis, posterior fossa arachnoiditis, and multiple sclerosis. Other risk factors include:
- Ear injuries in which the labyrinth is damaged;
- Inflammatory diseases of the middle ear, with spread of the infectious process to the labyrinth;
- Tumor processes characterized by tumor tissue sprouting into the auditory structures;
- Meniere's disease;
- Vestibular nerve lesions;
- Head injuries;
- Lesions of the craniovertebral zone (platybasia, Arnold-Chiari anomaly, atlas assimilation);
- Circulatory disorders due to atherosclerotic changes, hypertension, cerebral vascular aneurysms, vertebral artery syndrome.
Vestibular ataxia can be caused by any lesion of the hair cells located in the inner ear (inside the membranous labyrinth), as well as damage or compression of the vestibular nerve (VIII pair), vestibular analyzer cortical center, nucleus with localization in the brain stem.
Pathogenesis
The vestibular analyzer is responsible for spatial orientation of a human being, which is capable of determining and perceiving the force of gravity, location and type of motor activity of body parts, interpreting the movement of the torso and limbs in space.
Any change of body position is evaluated by hair cells, which are vestibular receptor mechanisms located on the thinnest basilar film in the receptor section of the auditory analyzer with localization in the anterior zone of the membranous labyrinth.
From the hair cells, signals are transmitted via the vestibular nerve (belongs to the eighth pair of cranial nerves) to the vestibular nuclei responsible for interpreting the incoming information.
Motor reactions are realized as a result of transportation of regulatory nerve signals from the vestibular nuclei to different parts of the central nervous system, which ensures proper balancing and distribution of muscle tone due to appropriate reflex responses.
When any segment of the vestibular analyzing pathway is affected or damaged, balance and motor coordination are impaired.
Depending on the localization of the lesion, the characteristic findings are as follows:
- Lateral cerebellar lesions cause symptoms on the same side as the lesion (ipsilateral), whereas diffuse lesions cause generalized symptoms.
- Lesions of the cerebellar hemispheres cause limb ataxia.
- Worm lesions cause trunk ataxia, gait with limb preservation.
- Lesions of the vestibulo-cerebellar regions cause balance disorders, vertigo, and gait ataxia.
Symptoms of the vestibular ataxia
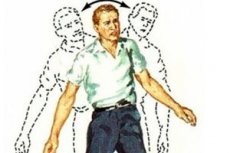
Signs of vestibular ataxia are noted both when walking (movements) and just standing. Depending on this, dynamic and static ataxia are distinguished. A distinctive feature of vestibular ataxia from other types of this pathology is the existence of dependence of the intensity of manifestations on the turn of the head and body. The problem is aggravated when turning the head, body or eyes, so patients try to avoid such movements, or make them carefully, gradually. By visually monitoring the movements, it is possible to compensate a little for the incorrect vestibular function. For this reason, the patient with closed eyes is less confident and ataxia is more pronounced.
The vestibular analyzer is usually affected unilaterally. Among the most frequent manifestations are:
- Shaky gait with body leaning to one particular side (the side of the lesion);
- Deviation of the torso to the affected side when standing or sitting;
- Unsatisfactory tests of walking with eyes closed as well as Romberg posture.
Typical first signs of vestibular ataxia include systemic vertigo, a sensation of rotation of the surroundings and torso. Dizziness occurs in any body position, even lying down. As a consequence, sleep is disturbed, the vestibular-visceral apparatus reacts - there is nausea, sometimes to vomiting. Over time, autonomic reactions are attached:
- The facial area turns pale or red;
- There's a sense of dread;
- Heart rate increases;
- Pulse is becoming labile;
- Increased sweating.
Most patients have horizontal nystagmus directed in the opposite direction from the lesion. Bilateral nystagmus may also occur. If the vestibular nuclei are affected, vertical nystagmus with rotation appears. If the pathology affects the peripheral part of the vestibular analyzer, there is an increase in nystagmus during initial head turns (further nystagmus, as a rule, decreases). In patients with craniovertebral anomalies, nystagmus increases with head tilts.
Stages
Ataxia is differentiated by the time of onset of this disorder:
- Acute ataxia lasts from hours to days and results from ischemia or hemorrhagic stroke, inflammatory processes or multiple sclerosis, vestibular neuronitis, or toxic encephalopathy.
- Subacute ataxia lasts for several weeks and develops as a result of tumor processes of the posterior cranial fossa, hypothyroidism and avitaminosis, alcoholism, etc.
- Chronic ataxia lasts for months or even years, which is characteristic of meningiomas, craniovertebral junction defects, and neurodegenerations.
Forms
In general, ataxia is subdivided into such types of pathology:
- Sensory ataxia (caused by a disorder of the conductive system of deep muscle sensitivity);
- Cerebellar ataxia (associated with cerebellar lesions);
- Cortical ataxia (involves lesions in the frontal or occipitotemporal cortex);
- Vestibular ataxia (caused by a lesion of a part of the vestibular apparatus).
Direct vestibular ataxia happens:
- Static (manifests itself when the patient is in a standing position);
- Dynamic (signs occur during movements).
In addition, vestibular ataxia can be unilateral (only the left or right side is affected) and bilateral.
Complications and consequences
Patients suffering from vestibular ataxia often fall and get injured. They lose their ability to work early, and are not always able to take good care of themselves, such as dressing, cooking and eating, etc.
As vestibular ataxia progresses, the person initially gets around with the use of a support, crutch, walker, or stroller, but may soon require constant assistance.
Bed rest and improper care can lead to the development of pressure sores.
Other possible complications:
- Tendency to recurrent infectious diseases, weakened immunity;
- Development of chronic heart and respiratory failure;
- Disability.
Lack of treatment, inability to eliminate the root cause of vestibular ataxia usually leads to steady progression and worsening of the patient's condition. Nevertheless, timely diagnosis and the use of modern methods of treatment and rehabilitation can stop or slow down the pathological process and improve the patient's quality of life.
Diagnostics of the vestibular ataxia
Vestibular ataxia is diagnosed based on the patient's complaints and the results of neurological examination. In order to clarify the diagnosis, to determine the degree and type of pathological process, instrumental diagnostics is prescribed - in particular, reoencephalography, echo-encephalography, electroencephalography, computer and magnetic resonance imaging of the brain, as well as X-ray. Since vestibular ataxia can accompany many pathologies of the central nervous system, it is important to identify the underlying causes of this disorder as early as possible.
Blood and urine tests in ataxia are nonspecific, but may be prescribed to assess the general condition of the body, to detect inflammatory processes and anemia. Laboratory diagnostics may be used if chemical, drug or alcohol intoxication is suspected, as well as if vitamin deficiency conditions (primarily B avitaminosis) are suspected.
Some patients are indicated to have tests for thyroid hormone status, HIV, syphilis, toxoplasmosis, Lyme disease, and anti-Yo antibodies (antibodies to Purkinje cells that lead to dysarthria and nystagmus).
Instrumental diagnosis is usually represented by the following methods:
- Rheoencephalography (helps to get general information about the quality of blood flow in the brain);
- Angiography, MR angiography of cerebral vessels (as an adjunct to rheoencephalography);
- Echoencephalography (used to assess the liquor system in the brain; changes on echo-EEG suggest the presence of a volumetric neoplasm such as a tumor or abscess, which may be associated with the development of vestibular ataxia);
- Electroencephalography (prescribed to examine bioelectrical brain activity);
- Computer and magnetic resonance imaging (help to detect volumetric neoplasms, foci of demyelination);
- X-ray of the cervical spine and skull (prescribed if craniovertebral defects are suspected).
Assessment of the vestibular apparatus in ataxia is performed by a neurologist, less often by an otorhinolaryngologist. Diagnosis may include vestibulometry, electronystagmography, stabilography, caloric test. If the patient is simultaneously diagnosed with hearing loss, it is possible to perform threshold audiometry, chamber tone testing, electrocochleography, promontory test and so on. [12]
Differential diagnosis
Ataxia is not only vestibular ataxia. It is a syndrome that can be observed not only when the vestibular apparatus is affected, but also other brain structures.
- Sensory ataxia occurs when deep sensory pathways are affected, starting from the peripheral nerves and ending with the posterior central gyrus. This disorder is characterized by a peculiar "stamping" gait: a person puts his feet wide while walking, each step is heavy, heavy, with a landing on the heel. The problem is aggravated if the patient is in the dark, or closes his eyes, or sharply raises his head. A false athetosis is noted. Pathology often accompanies polyradiculoneuritis, spinal disorders with lesions of the posterior canals.
- Frontal ataxia is the result of damage to the cortex of the large hemispheres of the frontal lobe and disruption of afferent connections with the cerebellum. Symptomatology is non-intense, the patient staggers while walking to the opposite side of the lesion. Intentionality, "misses" are noted.
Vestibular and cerebellar ataxia are particularly difficult to differentiate in patients with stroke and intoxication, when the magnitude of symptoms is such that the patient cannot walk or stand.
- Temporal ataxia is caused by a lesion of the temporal lobe cortex: its cerebellar connections are affected at the same time. Temporal ataxia is one of the components of the Schwab triad. The patient staggers while walking and deviates to the opposite side, misses when conducting the palpebral test. Hemiparkinsonism on the opposite side of the focal point is noted. If Schwab's triad is diagnosed, it indicates the presence of a tumor process in the temporal lobe.
- Functional ataxia is one of the symptoms of hysterical neurosis. The gait is peculiar and variable, not like other types of ataxia.
- Mixed ataxia is a combination of several types of this disorder - for example, both cerebellar and sensory ataxia are present at the same time. Such a combination can be observed in patients with demyelinating pathologies.
In the course of differential diagnosis, it is important to take into account the multiplicity of ataxia symptomatology. Practicing physicians point out the presence of rudimentary types of this disorder, transitional forms of the syndrome, in which the clinical picture is similar to that of multiple sclerosis, spastic paraplegia, neural amyotrophy.
If hereditary ataxia is suspected, DNA diagnosis is prescribed to determine the likelihood of inheriting an ataxic pathogen.
Treatment of the vestibular ataxia
Treatment for vestibular ataxia is directed at the underlying cause of the disorder. Currently, there is no treatment for hereditary ataxia. Depending on the cause, if ataxia results from stroke, toxic substances, hypothyroidism, or any modifiable risk factors, treatment is directed at the specific condition causing the ataxia. [13]
If an infectious process in the hearing organs is detected, antibiotic therapy, rinses, sanitation, labyrinthotomy, etc. Are prescribed. If vascular disorders are detected, drug therapy is used, which can improve cerebral blood circulation. In complex cases, patients with craniovertebral defects are prescribed their surgical correction. Volumetric neoplasms, inflammatory processes in the form of arachnoiditis or encephalitis require appropriate complex treatment.
After acting on the cause of vestibular ataxia, symptomatic therapy is started. Relevant drugs that accelerate metabolism, improve the nervous system:
- Piracetam - taken in a daily dose of 30 to 160 mg per kilogram of weight, with the frequency of intake twice a day. Duration of treatment is 1-6 months.
- γ-aminobutyric acid - administered orally before meals 0.5-1.25 g three times a day (daily dose - from 1.5 to 3 g).
- Ginkgo biloba - take tincture 15-20 drops before meals, or in tablets 60-240 mg. The duration of treatment is determined by a doctor and can be several months.
- B-group vitamins - administered orally or by injection, depending on the indication.
For the fastest rehabilitation, therapeutic exercise is indicated, including exercises to train motor coordination and strengthen the muscular framework and individual muscle groups. [14]
Prevention
There is no specific prevention of such a disorder as vestibular ataxia. To maintain health in general, and in particular, to support the normal state of the vestibular apparatus, it is necessary to direct efforts to prevent the development of acute infectious and inflammatory processes that can damage this mechanism. First of all, prevention concerns prevention of sinusitis, otitis media, inflammation of the lungs, etc.
Basic preventive recommendations include:
- Timely referral to a doctor for any infectious and inflammatory diseases;
- Timely consultation with a doctor in case of dizziness;
- Regular monitoring of blood pressure indicators (especially in people prone to the development of hypertension and vascular pathologies);
- Leading a healthy lifestyle, avoiding bad habits, nutritious diet with quality products, etc.
Forecast
Vestibular ataxia cannot be cured on its own, without the involvement of a medical specialist. Only quality diagnosis with determination of the root cause of the pathology and further prescription of adequate treatment can eliminate the primary disease and level the manifestations of pathology. To improve prognosis, it is important to take an individualized approach, since no two cases of vestibular ataxia are the same: the causes and signs of the disorder are always different.
Often, especially if the primary focus of pathology cannot be identified, disability and loss of ability to work occur. In some cases, including hereditary diseases, vestibular ataxia is poorly amenable to treatment, and its manifestations often persist for many years. The most optimistic prognosis is characterized by ataxia in patients with vestibular neuronitis: the problem is successfully cured and there are no relapses.
List of studies related to the study of vestibular ataxia
-
Vestibular Ataxia and its Measurement in Man
- Authors: A. R. Fregly
- Year of release: 1975
-
Case report: Acute vestibular syndrome and cerebellitis in anti-Yo paraneoplastic syndrome
- Authors: Bassil Kherallah, E. Samaha, S.E. Bach, Cynthia I. Guede, J. Kattah. Bach, Cynthia I. Guede, J. Kattah
- Year of release: 2022
-
Ocular Motility in North Carolina Autosomal Dominant Ataxia
- Authors: K. Small, S. Pollock, J. Vance, J. Stajich, M. Pericak-Vance
- Year of release: 1996
-
General vestibular testing
- Authors: T. Brandt, M. Strupp
- Year of release: 2005
-
Genetics of vestibular disorders: pathophysiological insights
- Authors: L. Frejo, I. Giegling, R. Teggi, J. Lopez-Escamez, D. Rujescu
- Year of release: 2016
Literature
Palchun, V. T. Otorhinolaryngology. National manual. Brief edition / Edited by V. V. Т. Palchun. - Moscow: GEOTAR-Media, 2012.

