Medical expert of the article
New publications
Toxic liver hepatitis: acute, chronic, drug-induced, alcoholic
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Toxic hepatitis is a pathological process in the liver that occurs as a result of toxic substances entering the body. Since their main processing and neutralization occurs in the liver, an acute or chronic inflammatory process develops. Acute toxic hepatitis occurs as a result of a high concentration of toxin entering the body, which disrupts the structural and functional disorder of the liver. In chronic hepatitis, the body is exposed to damaging agents for a long time and constantly, the pathology worsens gradually.
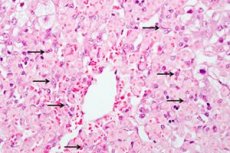
First, liver cells are damaged, then they die. The tissue is gradually transformed and replaced by connective tissue. This is associated with functional disorders, pain in the liver area. Jaundice progresses.
If you start treating the disease in time, you can slow down or stop the progression of the disease. If you do not take any efforts, you can get serious complications, including cirrhosis, severe insufficiency, which often end in death.
Epidemiology
Analyzing statistical data, it was found that women are more susceptible to liver damage than men. The earlier the therapy, the better the outcome of the disease. The occurrence of bleeding is the cause of death in approximately 30-50%. Coma has a fatal outcome in 80-100%. The occurrence of ascites ends in a fatal outcome in 80%, death occurs within 3-4 years.
Causes toxic hepatitis
Hepatitis can develop when toxic substances enter the body. Such ingestion can be accidental or intentional. For example, people often poison themselves with poisonous mushrooms, mistaking them for edible. Professional activity is often associated with accidental poisoning. When working with toxic substances, acids, vapors and dust enter the human body and have a damaging effect. Intentional poisoning is a case of suicide, in which a person ingests poison.
The main way of toxins penetration into the liver is peroral, through the digestive tract. From the stomach, absorption occurs, then transportation. In the liver tissue, they have the main damaging effect.
Poisoning can be caused by long-term use of medications or their high dosages. The greatest danger is posed by drugs that act against viruses, convulsions, and isoniazid.
Substances used in production can also poison the liver. In this case, the liver can be subject to acute or chronic pathology. All this is accompanied by the death of the liver. The greatest danger is phenolic compounds, arsenic, phosphorus elements. The cause can be alcohol abuse, especially if it is of poor quality, drugs. This is due to the fact that the main processing is assigned to the liver. The danger of toxic effects is due to a violation of fat metabolism: fatty degeneration of liver cells occurs. Narcotic elements are also neutralized. Many weeds and mushrooms have a toxic effect.
Risk factors
The risk group includes people whose professional activities are connected with toxins and caustic components. Alcoholics and drug addicts often end their lives with liver diseases. Suicides who took poison for the purpose of suicide but survived already have serious liver damage, which can progress.
People who are forced to constantly take strong medications should monitor their liver condition. This is especially true for those patients who take painkillers, anti-tuberculosis drugs. If a person already has any liver disease, viral hepatitis or is a carrier of viral hepatitis, he automatically falls into the risk group. In old age, the risk of development increases significantly, since the liver cannot cope with the load and processes everything much more slowly. Women are more at risk than men. This is due to a lower level of metabolism. Toxins are excreted from women much longer than from men.
Heredity plays an important role. There is a genetic predisposition to the development of liver diseases. Possible abnormalities in the structure of the liver and functional disorders are also taken into account. In addition, improper enzyme production can not only slow down the neutralization of toxins, but also stimulate their additional synthesis in the body. Also today, people who practice non-traditional types of intimate relationships and people with non-traditional orientation are at risk.
Pathogenesis
The pathogenesis is based on the damaging effect of toxins on the human body. Hepatocytes are damaged, structural and functional disorders occur, and they die off and are replaced by fatty tissue.
There is also a second mechanism for the development of pathology. Microcirculation of blood in the liver may be disrupted. The vascular bed is damaged, as a result of which the supply is disrupted, the organ does not receive the required amount of nutrients and oxygen. A high concentration of metabolic products and carbon dioxide accumulates. This damages the liver, has a toxic effect on it. Metabolic processes in the liver, including oxidation-reduction processes, are disrupted. Carbohydrate and protein metabolism suffers. Even the composition of the blood gradually changes. This causes irreversible processes in cell membranes: DNA replication is disrupted, enzyme activity decreases, and respiratory processes are suppressed. Hepatocytes undergo dystrophic processes and gradually die off.
The third path of disorders is associated with the disruption of normal bile acid metabolism, as a result of which bile metabolism is disrupted, the blood flow rate in the bile capillaries decreases, and the outflow of bile through the intrahepatic bile ducts decreases. The result is the same as in the first two cases: hepatocytes are damaged, they degenerate and gradually die.
How is toxic hepatitis transmitted?
Many people worry about infecting their relatives and family members with toxic hepatitis. We can confidently assure you: there is no reason to worry. Cases of hepatitis developing in families are impossible. The exception is cases of eating poisonous substances (for example, toadstools) or spoiled food products. The transmission route through contacts and household items is excluded.
Symptoms toxic hepatitis
Usually, hepatitis can be recognized by painful sensations under the right rib. Most often, pain appears on the 2nd-5th day. The liver enlarges. Muscle weakness makes itself known. The acute process is accompanied by intense bleeding, bleeding gums, fragility of blood vessels and small bruises on the surface of the skin. A person's behavior also changes significantly: he becomes overexcited, or, conversely, the pathology manifests itself in a slow reaction. Gradually, tremors in the body join in, gradual weight loss. Periodically, the stomach bloats, diarrhea appears. This is caused by a violation of the outflow of bile. Work capacity decreases sharply, fatigue increases. An important sign is itching all over the body. The skin begins to itch as a result of an increase in the amount of fatty acids in the dermis of the skin. The liver and spleen increase in size. Chronic hepatitis is indicated by alternating periods of remission and exacerbation.
As soon as you notice painful sensations in the liver area (under the right rib), you need to see a doctor as soon as possible. Early symptoms may also include loss of appetite and dyspeptic disorders.
Itchy skin in toxic hepatitis
Skin itching is caused by the accumulation of bile acids in the lower layers of the skin. To prevent this unpleasant phenomenon, you need to drink hepatoprotectors that protect the skin from harmful effects.
Exacerbation of toxic hepatitis
There is an alternation of the period of remission, during which the person feels quite well, with exacerbations. Exacerbation is accompanied by digestive disorders, an increase in the liver to such a size that it can be easily palpated under the right rib. Temperature may rise, intoxication appears.
 [ 15 ], [ 16 ], [ 17 ], [ 18 ]
[ 15 ], [ 16 ], [ 17 ], [ 18 ]
Toxic hepatitis during pregnancy
The development of hepatitis in a pregnant woman is indicated by pain in the liver area, fever, bleeding and hemorrhages. Behavior changes dramatically: inhibition or increased excitability develops. Loss of consciousness is possible. Not only the liver but also the spleen increases in size, and skin itching appears.
When the first signs appear, it is important to immediately consult a doctor to get a correct diagnosis and treatment. Self-medication is strictly prohibited. A pregnant woman must follow a strict diet. Bed rest should also be observed. Detoxification therapy is carried out, absorbents are used. Hepatoprotectors and choleretic drugs help restore liver cells. In severe cases, antidotes are used.
For prevention purposes, it is necessary to plan pregnancy in advance, to be checked in advance. It is important to treat any liver diseases, even if they are in remission or latent, and do not bother the woman at all. Otherwise, inflammation cannot be avoided. If you have a history of liver diseases, you must be checked regularly, undergo examination.
For pregnant women, toxic hepatitis is especially dangerous due to its complications. Hepatopathy develops, which results in impaired blood clotting. This is dangerous during childbirth, as it increases the risk of bleeding. When such complications develop, coagulopathic therapy is carried out in most cases, after which the pregnancy is terminated, and treatment is continued. An equally dangerous complication is hypercoagulation, in which blood clotting increases. This is fraught with the formation of blood clots. Both pathologies require termination of pregnancy. Childbirth is accompanied by hepatoprotective therapy, infusion of fresh frozen plasma, and stimulation of hemostasis. All pregnant women with liver damage of any etiology require urgent hospitalization.
Toxic hepatitis in children
Toxic liver damage in children is rare. If we analyze those rare cases of damage, we can note that neurological and cardiorespiratory symptoms predominate in such children. Circulatory disorders of the liver develop. Most often, accidental poisoning is observed in children, namely, poisoning with death cap. Less often, there is ingestion of high concentrations of drugs or toxic substances. Children use them unknowingly due to excessive curiosity, if the parents have hidden the poison not far enough from the child. The child is immediately sent to the intensive care unit, since acute necrosis develops rapidly.
In children, unlike adults, lesions may be caused by allergies, severe disorders of the immune system. They manifest themselves more severely. In addition to traditional symptoms, children may experience anaphylactic shock, intense skin rashes, and immune system disorders, including immunodeficiencies. Diuresis also increases. Necrosis develops very quickly.
Stages
First, the acute stage develops. In the absence of therapy, incomplete recovery, it becomes chronic. The final stage is ascites, often ending in death.
- Activity in toxic hepatitis
Depending on Determined by the dose, presence of concomitant pathologies, speed, degree of activity. Hepatitis with maximum toxic activity develops most rapidly. It often has a fatal outcome.
- Toxic hepatitis of minimal activity
The degree of activity is typical of toxic hepatitis. Hepatitis with a minimal degree of activity has a favorable prognosis. It develops slowly and is easily treated. Its development is mainly stimulated by a weakened immune system. This form is characterized by a mild inflammatory process that does not cause pain and does not cause discomfort to patients. It leads to an increase in size.
Forms
There are many types of hepatitis. In this regard, there are various classifications based on various factors. According to the main classification, the disease is divided into acute and chronic. The acute process is characterized by rapid progression of pathologies - due to the duration of the action of damaging factors. It develops slowly, is less severe. The consequences and complications are no less serious.
There are many types of hepatitis. The most common are drug-induced, professional, alimentary, viral, drug-induced and alcoholic cirrhosis. Toxic hepatitis with transition to liver cirrhosis is singled out separately.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ]
Acute toxic hepatitis
The distinctive feature is that hepatitis develops very quickly, at a rapid pace. The peak of the disease occurs on the 3rd day of toxin exposure. Intense pain appears, which occurs as a result of hypertrophy. The temperature rises sharply, to 38 degrees and above. Weakness, body aches, increased fragility, dyspeptic syndrome appear.
 [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ]
[ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ]
Toxic drug-induced hepatitis
Toxicosis is often a consequence of drug poisoning. The cause is an excess of dosage or long-term use of drugs. With long-term use, a chronic form most often develops, with an overdose - an acute form. The liver is often the only target organ that is exposed to toxins. The liver primarily reacts to the action of drugs, since their processing occurs in the liver. The liver also neutralizes the remains and removes them.
The dosage and duration of medication varies widely. Currently, there are several thousand drugs that can cause liver damage. Often, the cause of such complications is self-medication, since many such drugs are sold without a prescription. 50% are due to errors by doctors who incorrectly prescribe drugs or incorrectly combine them.
Some drugs have inevitable side effects on the liver, regardless of the dose. But often, taking such drugs cannot be avoided. For example, chemotherapy, antiretroviral therapy, antitumor drugs. In people with increased sensitization of the body, frequent allergic reactions, in elderly people, the risk of developing toxic hepatitis increases when taking any drug. Even seemingly harmless antibiotics and antipyretics can cause significant damage to the liver.
Hormonal agents, antidepressants, psychotropic substances and neuroleptics, diuretics, antibacterial and antiviral drugs are especially dangerous for the liver. Some combinations of drugs can have a toxic effect. Exceeding the dosage of many drugs ends in death. Thus, if you take 10 g of paracetamol, liver necrosis develops. This drug is often taken for suicidal purposes. Toxic hepatitis often develops after treatment of diseases such as leukopenia, splenomegaly.
The main condition for recovery is the abolition of drugs that have a toxic effect on the liver. It is also necessary to eliminate other causes that aggravate the inflammatory process. After this, appropriate therapy is carried out, which leads to the reverse development of the pathology. If measures are taken in a timely manner, the prognosis may be favorable. In severe cases, hemodialysis may be required, which usually has a positive effect, promotes the recovery of the body. If liver failure develops, an urgent liver transplant may be required.
To prevent drug-induced hepatitis, taking heavy medications that have side effects should be combined with hepatoprotectors. They protect against negative effects, reduce the likelihood of damage and the severity of the pathology.
Alcoholic toxic hepatitis
Alcohol, especially low-quality alcohol, has a negative effect. It is neutralized in the liver. Toxins are formed that have a damaging effect on a person. They necrosis, which ultimately contributes to cirrhosis, a fatal outcome.
 [ 37 ]
[ 37 ]
Occupational toxic hepatitis
It is a consequence of the impact of harmful production factors on the body. Most often observed in employees who have worked in the production sector or in laboratories for a long time. The risk of occupational hepatitis is especially high in employees with reduced immunity and concomitant viral hepatitis or other liver diseases.
It can develop in both acute and chronic forms. In the acute form, it develops as a result of industrial leaks, carelessness, equipment malfunction or a non-working exhaust hood. In these cases, the body receives a large dose of the drug at once.
In the chronic form, poisoning develops slowly, gradually. For example, a person inhales vapors of toxic substances for a long time. The main industrial poisons are yellow phosphorus, trichloroethylene, carbon. Biological agents, such as fungi, viruses, bacteria, which microbiologists, virologists, and bacteriologists have to work with, are also dangerous. No less dangerous are pharmaceutical and chemical preparations that are used for medical purposes or for research.
Alimentary toxic hepatitis
This form of the disease is also called fecal-oral hepatitis. The main cause of the disease is fragments of fecal matter that get from an infected person to a healthy person. Spread occurs through the mouth, during oral contact. People with a craving for non-traditional methods of sexual relations are susceptible to this form of infection.
This mechanism erroneously suggests that toxic hepatitis is contagious. But this is not the case. It is important to understand that it is not the disease itself that is transmitted, but the toxic agent that causes it. It is this that leads to the development of similar damage in the body.
 [ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ]
[ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ]
Viral toxic hepatitis
The cause of development is a virus that releases toxins and products of viral metabolism into the blood. These substances are called endotoxins. They penetrate the liver and cause pathological changes in it, including necrosis and fatty degeneration of the liver. Viral hepatitis is confirmed by virological studies. Sometimes the disease is latent, so it is important to undergo preventive examination and take tests. This will allow timely detection of pathology and take the necessary measures.
Treatment depends on which form of the virus caused the changes. This cannot be done without laboratory tests. Viral hepatitis B, C, D are transmitted sexually and through drug addiction. Infection can also occur during surgical interventions, during invasive procedures as a result of failure to comply with aseptic rules.
The most severe is hepatitis C. The disease may not always manifest itself externally. A person may feel quite well, after which a sharp crisis occurs. The liver is damaged slowly and asymptomatically. It ultimately manifests itself as cirrhosis of the liver, after which the person quickly dies. In addition, it can cause complications in other organs.
Hepatitis B is widespread among the population and is often transmitted by blood transfusion. The main preventive measure is monitoring of donor blood and regular preventive examination. If detected in time, it can be treated. However, if detected late, it often ends in death.
Hepatitis D often overlaps with hepatitis B. Together they form a dangerous disease that manifests itself in a severe form and gives serious complications. In most cases, it ends fatally.
Toxic hepatitis after chemotherapy
One of the leading causes is the impact of chemotherapy and antiviral therapy, which contributes to liver damage in both acute and chronic forms. This is due to the fact that the main breakdown of antitumor drugs occurs in the liver. As a result, all liver functions are disrupted, including detoxification. Cytostatics stop the growth and division of tumor cells, but at the same time, they have a similar effect on liver cells. Cells lose their ability to regenerate. This leads to the drug accumulating in the liver and having a toxic effect on the liver. As a result of chemotherapy, toxic hepatitis is complicated by cholestatic disorders and hepatic encephalopathy. All this is accompanied by a rash, pain. Body temperature increases significantly.
In order to minimize the negative impact of chemotherapy on the liver, it is necessary to conduct constant monitoring of the liver. The main analysis is a biochemical blood test. In accordance with modern requirements, a blood test must be taken before the start of chemotherapy, and then on the 14th day of treatment. The condition is carefully monitored from the 14th to the 21st day. During this time, tests are often taken daily. Bilirubin and transaminase levels are monitored, which are a sign of toxic liver damage. After the end of cancer therapy, the liver condition is monitored monthly for 6 months, then every 6 months.
Toxicosis during chemotherapy can be prevented by carrying out hepatoprotection. It restores the structure of damaged membranes, slows down destructive processes in hepatocytes, and prevents fibrosis.
Exogenous toxic hepatitis
Caused by exposure to environmental toxins. These are elements of any nature and origin, including heavy metals, acid vapors, alcohol, and medications. They can provoke both acute and chronic forms of the disease. The pathogenesis is mainly based on a violation of liver hemostasis.
Exogenous poisoning often occurs in agriculture when treating with insecticides and herbicides. The most severe forms are observed when poisoning with arsenic, carbon, and phosphorus. Many medications, and even hormonal contraceptives, damage the liver.
Complications and consequences
Toxic hepatitis rarely passes without consequences. The exception is cases when it occurs in a mild form and is detected in the early stages. Then it is possible to conduct therapy in a timely manner and cure the disease. Otherwise, numerous pathologies develop, including liver failure, coma. Liver failure - hepatocytes are replaced by fat cells. This manifests itself in the form of edema. Coagulation is significantly reduced, its properties change. A person loses weight sharply, since he does not have enough fats that are produced by the liver. There is also a lack of energy, which is accompanied by weakness and increased fatigue. Hepatic encephalopathy also develops. The process is constantly progressing, convulsions appear. It can end in death. The final stage can be cirrhosis of the liver. When the cells completely die and are replaced. Leads to death.
Toxic hepatitis leading to cirrhosis
The most severe complication. There are three stages of development: compensatory, subcompensatory and decompensatory. First, the disease goes into the compensatory stage, which manifests itself as a moderate inflammatory process, tissues are damaged, and scarring begins. Functional activity is sharply reduced, but at this stage the body can still compensate for lost functions.
When moving into the subcompensatory stage, symptoms of liver damage appear and connective tissue grows significantly.
The third stage is decompensation, which is the most dangerous. It often ends in death. At this stage, scar tissue occupies most of the liver. There is a huge risk of liver failure and coma. These conditions often end in death.
 [ 50 ], [ 51 ], [ 52 ], [ 53 ], [ 54 ], [ 55 ]
[ 50 ], [ 51 ], [ 52 ], [ 53 ], [ 54 ], [ 55 ]
Ascites in toxic hepatitis
Ascites is a pathological condition in which fluid accumulates in the abdominal cavity. This is due to pathological metabolism, as a result of which the normal fluid output is disrupted. Compression of internal organs occurs, concomitant pathologies and gastroenterological pathologies arise.
Ascites can develop slowly. The most severe stage compresses the diaphragm, and breathing is impaired. After ascites appears, the disease enters the terminal stage.
If severe bleeding and collapse occur, this often indicates a rupture of the portal vein, which could not withstand the pressure.
Diagnostics toxic hepatitis
Various methods are used to establish a diagnosis. An examination is performed, the patient's life history is collected. Based on this data, the necessary laboratory and instrumental studies are prescribed. Differential diagnostics with other diseases that have similar symptoms are carried out. After this, an accurate diagnosis is made.
Rationale for the diagnosis of toxic hepatitis
To select the right treatment, it is not enough to simply make a diagnosis, it is also necessary to justify it. To do this, it is necessary to confirm that it is of a toxic nature. Most often, a toxicological study is carried out, which determines which substance caused damage to the liver. After this, the most important condition for successful treatment is the cessation of the effect of this factor on the body. If the substance continues to have a toxic effect, recovery is impossible, even with complex therapy.
Laboratory findings in toxic hepatitis
The development of hepatitis is indicated by an increase in the bilirubin level to 800-850 μmol/l. When examining bilirubin by fractions, it can be noted that direct bilirubin is predominant, its indicators are approximately 1.5 times higher than the amount of indirect bilirubin.
Urine analysis shows positive results when conducting a reaction with bile pigments and urobilin. Moderate proteinuria is noted. Bilirubin in toxic hepatitis
Liver damage of various etiologies is indicated by an increase in bilirubin above 17.1 μmol/l. A mild form of hepatitis is indicated by a level of up to 86 μmol/l, and a moderate form by up to 159. A severe form can be indicated by a level above 160 μmol/l.
Instrumental diagnostics: the liver and spleen sizes remain normal. If these data are insufficient to make an accurate diagnosis, computed tomography and magnetic resonance imaging (CT and MRI), liver scintigraphy are used.
Scintigraphy is a new diagnostic method in which radioactive isotopes are injected into the human body. The substances are injected through a vein. After 15 minutes, the examination begins. The resulting radiation makes it possible to visualize the image of internal organs and display it on the screen. This method determines the functional characteristics of the organ and determines the size of the liver. The procedure lasts approximately 20 minutes.
A biopsy or laparoscopy with targeted biopsy may be required.
What do need to examine?
Differential diagnosis
The essence of differential diagnostics is to accurately separate toxic hepatitis from another disease that has similar manifestations. After the diagnosis of hepatitis is confirmed, further differentiation is carried out, the purpose of which is to determine its type. In this case, it is necessary to confirm that we are dealing with toxic hepatitis, which is caused by the effect of toxic substances on the body.
Various diagnostic methods are used for this. Instrumental diagnostic methods and laboratory tests are most often used to confirm hepatitis. Splenomegaly, leukopenia, and elevated bilirubin levels may indicate hepatitis. Ultrasound reveals a specific clinical picture characteristic of hepatitis.
In order to establish the nature of the damaging factor, serological tests are carried out. Toxicological analysis may indicate an increased level of toxin in the blood. Virological and serological studies will show the absence of a viral load in the body, which will allow excluding hepatitis of viral etiology. If hepatitis of alcoholic etiology is suspected, a consultation with a toxicologist or narcologist may be required. An immunological study is also carried out to determine the presence of antibodies in the blood that are characteristic of autoimmune hepatitis.
 [ 62 ], [ 63 ], [ 64 ], [ 65 ], [ 66 ]
[ 62 ], [ 63 ], [ 64 ], [ 65 ], [ 66 ]
Differential diagnostics of viral hepatitis with toxic hepatitis
Toxic hepatitis can be differentiated from viral hepatitis based on the results of toxicological and virological (serological) studies. In viral hepatitis, an increased concentration of antibodies to the hepatitis virus is detected, or the viruses themselves are detected. Everything depends on the diagnostic method. This is a direct confirmation or refutation of the diagnosis. Toxicological diagnostics are carried out to confirm the toxic nature of hepatitis. The amount of toxin and its type are detected.
Who to contact?
Treatment toxic hepatitis
There are many different treatment regimens for toxic hepatitis. But they are based on standard principles that must be followed. Any successful therapy must be based solely on these principles.
More information of the treatment
Prevention
Prevention comes down to careful control of the food consumed. If a person works with harmful factors at work, it is necessary to strictly observe safety regulations and personal hygiene. The room must be ventilated, and work must be done under a hood. When taking medications, it is necessary to strictly observe the dosage and follow the doctor's recommendations. If necessary, additionally take hepatoprotectors. It is necessary to give up alcohol or take only high-quality alcohol. When the first signs of the disease appear, you need to see a doctor as soon as possible.
Forecast
It all depends on the severity of the disease and how quickly the correct treatment was prescribed. At a mild stage of the disease, the prognosis can be favorable. The liver can fully recover if the disease is diagnosed in time and treatment is started. Full recovery is possible with further regular preventive examinations and maintenance therapy.
If the disease becomes chronic or severe, the risk of complications increases. Damage to hepatocytes progresses. The cells gradually die and are replaced by connective tissue. The most dangerous complications of severe hepatitis are liver failure, coma, and liver cirrhosis. The prognosis can be extremely unfavorable, even fatal. If ascites appears, one should expect a quick death. As a rule, patients with ascites die within a few days, and only 10% manage to survive a month with this pathology.
How long do you live with toxic hepatitis?
When diagnosed with toxic hepatitis, the duration and quality of life largely depend on the patient. It is necessary to conduct complete and timely treatment, fully comply with the doctor's recommendations, as well as follow a diet and bed rest. In this case, the person will recover fairly quickly. But in the future, he will need regular preventive examinations and maintenance therapy. In this case, you can live for decades. If you ignore diagnosis and treatment, the disease can develop into cirrhosis and ascites, which ends in death. With such complications, people live from several months to two years.

