Medical expert of the article
New publications
Thrombocytopenias and platelet dysfunction
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A disorder of the blood system in which there is an insufficient number of platelets circulating in the blood – cells that ensure hemostasis and play a key role in the blood clotting process – is defined as thrombocytopenia (ICD-10 code – D69.6).
What is the danger of thrombocytopenia? A reduced concentration of platelets (less than 150 thousand/mcl) worsens blood clotting so much that there is a risk of spontaneous bleeding with significant blood loss with the slightest damage to blood vessels.
Platelet disorders include abnormally elevated platelet levels (thrombocythemia in myeloproliferative disorders, thrombocytosis as a reactive phenomenon), decreased platelet levels (thrombocytopenia), and platelet dysfunction. Any of these conditions, including elevated platelet levels, can cause impaired hemostatic clot formation and bleeding.
Platelets are fragments of megakaryocytes that provide hemostasis of circulating blood. Thrombopoietin is synthesized by the liver in response to a decrease in the number of bone marrow megakaryocytes and circulating platelets and stimulates the bone marrow to synthesize platelets from megakaryocytes. Platelets circulate in the bloodstream for 7-10 days. About 1/3 of platelets are temporarily deposited in the spleen. The normal platelet count is 140,000-440,000/μl. However, the platelet count may vary slightly depending on the phase of the menstrual cycle, decrease in late pregnancy (gestational thrombocytopenia) and increase in response to inflammatory cytokines of the inflammatory process (secondary or reactive thrombocytosis). Platelets are ultimately destroyed in the spleen.
Causes of thrombocytopenia
Causes of thrombocytopenia include impaired platelet production, increased splenic sequestration with normal platelet survival, increased platelet destruction or consumption, platelet dilution, and a combination of these. Increased splenic sequestration suggests splenomegaly.
The risk of bleeding is inversely proportional to the platelet count. When the platelet count is less than 50,000/μl, minor bleeding is easily caused and the risk of major bleeding increases. When the platelet count is between 20,000 and 50,000/μl, bleeding may occur even with minor trauma; when the platelet count is less than 20,000/μl, spontaneous bleeding is possible; when the platelet count is less than 5000/μl, significant spontaneous bleeding is likely.
Platelet dysfunction may occur due to an intracellular defect of platelet abnormality or due to an external influence that damages the function of normal platelets. Dysfunction may be congenital or acquired. Of the congenital disorders, von Willebrand disease is the most common, and intracellular platelet defects are less common. Acquired platelet dysfunction is often caused by various diseases, taking aspirin or other medications.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ]
Other causes of thrombocytopenia
Platelet destruction may occur due to immune causes (HIV infection, drugs, connective tissue diseases, lymphoproliferative diseases, blood transfusions) or non-immune causes (gram-negative sepsis, acute respiratory distress syndrome). Clinical and laboratory signs are similar to those in idiopathic thrombocytopenic purpura. Only a medical history can confirm the diagnosis. Treatment is associated with the correction of the underlying disease.
Acute respiratory distress syndrome
Patients with acute respiratory distress syndrome may develop nonimmune thrombocytopenia, possibly due to platelet deposition in the pulmonary capillary bed.
 [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
[ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
Blood transfusions
Posttransfusion purpura is caused by immune destruction similar to ITP, except there is a history of blood transfusion within 3 to 10 days. Patients are predominantly women and lack the platelet antigen (PLA-1) that most people have. Transfusions of PLA-1-positive platelets stimulate the production of PLA-1 antibodies, which (by an unknown mechanism) can react with the patient's PLA-1-negative platelets. The result is severe thrombocytopenia, which resolves within 2 to 6 weeks.
Connective tissue and lymphoproliferative diseases
Connective tissue disorders (eg, SLE) and lymphoproliferative disorders may cause immune thrombocytopenia. Glucocorticoids and splenectomy are often effective.
 [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
[ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
Drug-induced immune destruction
Quinidine, quinine, sulfonamides, carbamazepine, methyldopa, aspirin, oral antidiabetic drugs, gold salts, and rifampin can cause thrombocytopenia, usually due to an immune reaction in which the drug binds to a platelet to form a new "foreign" antigen. This condition is indistinguishable from ITP except for the history of drug use. When the drug is stopped, platelet counts increase within 7 days. Gold-induced thrombocytopenia is an exception, as gold salts can persist in the body for many weeks.
Thrombocytopenia develops in 5% of patients receiving unfractionated heparin, which may occur even when very low doses of heparin are administered (eg, when flushing an arterial or venous catheter). The mechanism is usually immune. Bleeding may occur, but more commonly platelets form aggregates causing vascular occlusion with the development of paradoxical arterial and venous thromboses, sometimes life-threatening (eg, thrombotic occlusion of arterial vessels, stroke, acute myocardial infarction). Heparin should be discontinued in all patients who develop thrombocytopenia or a decrease in platelet count by more than 50%. Since 5 days of heparin administration is sufficient to treat venous thromboses, and most patients are started on oral anticoagulants simultaneously with heparin, discontinuation of heparin is usually safe. Low molecular weight heparin (LMWH) is less immunogenic than unfractionated heparin. However, LMWH is not used in heparin-induced thrombocytopenia because most antibodies cross-react with LMWH.
Gram-negative sepsis
Gram-negative sepsis often causes nonimmune thrombocytopenia that is proportional to the severity of the infection. Thrombocytopenia may be caused by many factors: disseminated intravascular coagulation, formation of immune complexes that can interact with platelets, activation of complement, and platelet deposition on damaged endothelial surfaces.
HIV infection
Patients infected with HIV may develop immune thrombocytopenia, similar to ITP except associated with HIV. Platelet counts can be increased by glucocorticoids, which are often withheld until platelet counts fall below 20,000/μL because these drugs may further depress immunity. Platelet counts also commonly increase after use of antiviral drugs.
Pathogenesis of thrombocytopenia
The pathogenesis of thrombocytopenia is either due to pathology of the hematopoiesis system and decreased production of platelets by myeloid cells of the bone marrow (megakaryocytes), or to impaired hemodieresis and increased destruction of platelets (phagocytosis), or to sequestration pathologies and retention of platelets in the spleen.
The bone marrow of healthy people produces an average of 10 11 platelets daily, but not all of them circulate in the systemic bloodstream: reserve platelets are stored in the spleen and released when needed.
When the patient's examination does not reveal any diseases that caused the decrease in platelet levels, a diagnosis of thrombocytopenia of unknown genesis or idiopathic thrombocytopenia is made. But this does not mean that the pathology arose "just like that."
Thrombocytopenia, associated with a decrease in platelet production, develops with a lack of vitamins B12 and B9 (folic acid) in the body and aplastic anemia.
Leukopenia and thrombocytopenia are combined in bone marrow dysfunction associated with acute leukemia, lymphosarcoma, cancer metastases from other organs. Suppression of platelet production may be due to changes in the structure of hematopoietic stem cells in the bone marrow (the so-called myelodysplastic syndrome), congenital hypoplasia of hematopoiesis (Fanconi syndrome), megakaryocytosis or myelofibrosis of the bone marrow.
Also read – Causes of Thrombocytopenia
Symptoms of thrombocytopenia
Platelet disorders result in a typical bleeding pattern in the form of multiple petechiae on the skin, usually more on the legs; scattered small ecchymoses at the sites of minor injuries; bleeding of the mucous membranes (nosebleeds, bleeding in the gastrointestinal tract and genitourinary tract; vaginal bleeding), severe bleeding after surgical interventions. Severe bleeding in the gastrointestinal tract and CNS can be life-threatening. However, manifestations of severe bleeding into tissues (eg, deep visceral hematoma or hemarthrosis) are atypical for platelet pathology and suggest the presence of secondary hemostasis disorders (eg, hemophilia).
Autoimmune thrombocytopenia
The pathogenesis of increased platelet destruction is divided into immune and non-immune. And the most common is autoimmune thrombocytopenia. The list of immune pathologies in which it manifests itself includes: idiopathic thrombocytopenia (immune thrombocytopenic purpura or Werlhof's disease ), systemic lupus erythematosus, Sharp or Sjogren's syndromes, antiphospholipid syndrome, etc. All these conditions are united by the fact that the body produces antibodies that attack its own healthy cells, including platelets.
It should be borne in mind that when antibodies from a pregnant woman with immune thrombocytopenic purpura enter the fetus's bloodstream, transient thrombocytopenia is detected in the child during the neonatal period.
According to some data, antibodies against platelets (their membrane glycoproteins) can be detected in almost 60% of cases. The antibodies have immunoglobulin G (IgG), and, as a result, platelets become more vulnerable to increased phagocytosis by splenic macrophages.
 [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
[ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
Congenital thrombocytopenia
Many abnormalities and their result – chronic thrombocytopenia – have a genetic pathogenesis. Megakaryocytes are stimulated by the protein thrombopoietin synthesized in the liver and encoded on chromosome 3p27, and the protein responsible for the effect of thrombopoietin on a specific receptor is encoded by the C-MPL gene.
Congenital thrombocytopenia (in particular, amegakaryocytic thrombocytopenia), as well as hereditary thrombocytopenia (in familial aplastic anemia, Wiskott-Aldrich syndrome, May-Hegglin syndrome, etc.) are believed to be associated with a mutation in one of these genes. For example, an inherited mutant gene forms constantly activated thrombopoietin receptors, which causes hyperproduction of abnormal megakaryocytes that are unable to form a sufficient number of platelets.
The average lifespan of circulating platelets is 7-10 days, their cell cycle is regulated by the anti-apoptotic membrane protein BCL-XL, which is encoded by the BCL2L1 gene. In principle, the function of BCL-XL is to protect cells from damage and induced apoptosis (death), but it turned out that when the gene mutates, it acts as an activator of apoptotic processes. Therefore, the destruction of platelets can occur faster than their formation.
But hereditary disaggregation thrombocytopenia, characteristic of hemorrhagic diathesis (Glanzmann thrombasthenia) and Bernard-Soulier syndrome, has a slightly different pathogenesis. Due to a gene defect, thrombocytopenia is observed in young children, associated with a violation of the structure of platelets, which deprives them of the ability to "stick together" to form a blood clot, which is necessary to stop bleeding. In addition, such defective platelets are quickly utilized in the spleen.
 [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ]
[ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ]
Secondary thrombocytopenia
By the way, about the spleen. Splenomegaly – an increase in the size of the spleen – develops for various reasons (due to liver pathologies, infections, hemolytic anemia, obstruction of the hepatic vein, infiltration by tumor cells in leukemia and lymphomas, etc.), and this leads to the fact that up to a third of the entire mass of platelets can be retained in it. As a result, a chronic disorder of the blood system occurs, which is diagnosed as symptomatic or secondary thrombocytopenia. When this organ is enlarged, splenectomy for thrombocytopenia is often indicated, or, simply put, removal of the spleen for thrombocytopenia.
Chronic thrombocytopenia can also develop due to hypersplenism syndrome, which refers to hyperfunction of the spleen, as well as premature and too rapid destruction of blood cells by its phagocytes. Hypersplenism is secondary in nature and most often occurs as a result of malaria, tuberculosis, rheumatoid arthritis or tumors. So, in fact, secondary thrombocytopenia becomes a complication of these diseases.
Secondary thrombocytopenia is associated with a bacterial or systemic viral infection: Epstein-Barr virus, HIV, cytomegavirus, parvovirus, hepatitis, varicella-zoster virus (cause of chickenpox), or rubella virus (cause of rubella).
When the body is exposed (directly to the bone marrow and its myeloid cells) to ionizing radiation and large amounts of alcohol are consumed, secondary acute thrombocytopenia may develop.
Thrombocytopenia in children
According to research, in the second trimester of pregnancy, the level of platelets in the fetus exceeds 150 thousand/mcl. Thrombocytopenia in newborns is present after 1-5% of births, and severe thrombocytopenia (when platelets are less than 50 thousand/mcl) occurs in 0.1-0.5% of cases. At the same time, a significant proportion of infants with this pathology are born prematurely or had placental insufficiency or fetal hypoxia. In 15-20% of newborns, thrombocytopenia is alloimmune - as a result of receiving antibodies to platelets from the mother.
Neonatologists believe that other causes of thrombocytopenia include genetic defects of bone marrow megakaryocytes, congenital autoimmune pathologies, the presence of infections, and DIC (disseminated intravascular coagulation) syndrome.
In most cases, thrombocytopenia in older children is symptomatic, and possible pathogens include fungi, bacteria, and viruses, such as cytomegalovirus, toxoplasma, rubella, or measles. Acute thrombocytopenia is especially common in fungal or gram-negative bacterial infections.
Vaccinations for thrombocytopenia in children are given with caution, and in severe forms of the pathology, prophylactic vaccination by injections and skin applications (with skin scarification) may be contraindicated.
For more information, see – Thrombocytopenia in Children, and also – Thrombocytopenic Purpura in Children
Thrombocytopenia in pregnancy
Thrombocytopenia during pregnancy can have many causes. However, it should be taken into account that the average number of platelets during pregnancy decreases (to 215 thousand/mcl), and this is a normal phenomenon.
Firstly, in pregnant women, the change in the number of platelets is associated with hypervolemia – a physiological increase in blood volume (on average by 45%). Secondly, the consumption of platelets during this period is increased, and bone marrow megakaryocytes produce not only platelets, but also significantly more thromboxane A2, which is necessary for platelet aggregation during blood coagulation (clotting).
In addition, in the α-granules of platelets of pregnant women, the dimeric glycoprotein PDGF is intensively synthesized - a platelet-derived growth factor that regulates the growth, division and differentiation of cells, and also plays a key role in the formation of blood vessels (including in the fetus).
As obstetricians note, asymptomatic thrombocytopenia is observed in approximately 5% of pregnant women with normal gestation; in 65-70% of cases, thrombocytopenia of unknown genesis occurs. Moderate thrombocytopenia is observed in 7.6% of pregnant women, and severe thrombocytopenia develops during pregnancy in 15-21% of women with preeclampsia and gestosis.
Classification of thrombocytopenia
Cause |
Terms and Conditions |
Impaired platelet production Decreased or absent megakaryocytes in the bone marrow. Decreased platelet production despite the presence of megakaryocytes in the bone marrow |
Leukemia, aplastic anemia, paroxysmal nocturnal hemoglobinuria (in some patients), myelosuppressive drugs. Alcohol-induced thrombocytopenia, thrombocytopenia in megaloblastic anemia, HIV-associated thrombocytopenia, myelodysplastic syndrome |
Platelet sequestration in an enlarged spleen |
Cirrhosis with congestive splenomegaly, myelofibrosis with myeloid metaplasia, Gaucher disease |
Increased platelet destruction or immune platelet destruction |
Idiopathic thrombocytopenic purpura, HIV-associated thrombocytopenia, post-transfusion purpura, drug-induced thrombocytopenia, neonatal alloimmune thrombocytopenia, connective tissue diseases, lymphoproliferative disorders |
Destruction not mediated by immune mechanisms |
Disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, thrombocytopenia in acute respiratory distress syndrome |
Breeding |
Massive blood transfusions or exchange transfusions (loss of platelet viability in stored blood) |
 [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ]
[ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ]
Thrombocytopenia due to splenic sequestration
Increased platelet sequestration in the spleen occurs in various diseases associated with splenomegaly. It occurs in patients with congestive splenomegaly due to advanced cirrhosis. The platelet count is usually greater than 30,000 μl unless the disease causing splenomegaly impairs platelet production (eg, myelofibrosis with myeloid metaplasia). During stress, platelets are released from the spleen after exposure to adrenaline. Therefore, thrombocytopenia due solely to platelet sequestration in the spleen does not result in increased bleeding. Splenectomy normalizes thrombocytopenia, but it is not indicated unless there is severe thrombocytopenia additionally caused by impaired hematopoiesis.
Drug-induced thrombocytopenia
Drug-induced or drug-induced thrombocytopenia is due to the fact that many common pharmacological drugs can affect the blood system, and some can suppress the production of megakaryocytes in the bone marrow.
The list of drugs that cause thrombocytopenia is quite extensive and includes antibiotics and sulfonamides, analgesics and NSAIDs, thiazide diuretics and antiepileptic drugs based on valproic acid. Transient, i.e. transient thrombocytopenia can be provoked by interferons, as well as proton pump inhibitors (used in the treatment of gastric and duodenal ulcers).
Thrombocytopenia after chemotherapy is also a side effect of antitumor cytostatic drugs (Methotrexate, Carboplatin, etc.) due to their suppression of the functions of hematopoietic organs and myelotoxic effects on the bone marrow.
Heparin-induced thrombocytopenia develops because heparin, used to treat and prevent deep vein thrombosis and pulmonary embolism, is a direct-acting anticoagulant, meaning it reduces platelet aggregation and prevents blood clotting. Heparin use causes an idiosyncratic autoimmune reaction that manifests itself in the activation of platelet factor-4 (protein-cytokine PF4), which is released from the α-granules of activated platelets and binds to heparin to neutralize its effect on the endothelium of blood vessels.
 [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
[ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
Degrees of thrombocytopenia
It should be remembered that the normal platelet count is from 150 thousand/mcl to 450 thousand/mcl; and there are two pathologies associated with platelets: thrombocytopenia, discussed in this publication, and thrombocytosis, in which the platelet count exceeds the physiological norm. Thrombocytosis has two forms: reactive and secondary thrombocythemia. The reactive form can develop after removal of the spleen.
The degrees of thrombocytopenia vary from mild to severe. In moderate degrees, the level of circulating platelets is 100 thousand/mcl; in moderately severe degrees – 50-100 thousand/mcl; in severe degrees – below 50 thousand/mcl.
According to hematologists, the lower the level of platelets in the blood, the more severe the symptoms of thrombocytopenia. In mild degrees, the pathology may not manifest itself in any way, and in moderate degrees, a rash with thrombocytopenia appears on the skin (especially on the legs) – these are pinpoint subcutaneous hemorrhages (petechiae) of red or purple color.
If the platelet count is below 10-20 thousand/mcl, spontaneous formation of hematomas (purpura), nosebleeds and gum bleeding occurs.
Acute thrombocytopenia is often a consequence of infectious diseases and resolves spontaneously within two months. Chronic immune thrombocytopenia persists for longer than six months, and often its specific cause remains unclear (thrombocytopenia of unknown genesis).
In extremely severe thrombocytopenia (platelet count <5000/μl), serious, fatal complications are possible: subarachnoid or intracerebral hemorrhage, gastrointestinal or other internal bleeding.
Diagnosis of thrombocytopenia
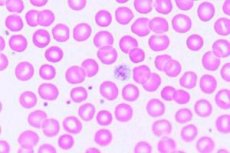
Platelet dysfunction is suspected in patients with petechiae and mucosal bleeding. A complete blood count with platelet count, hemostasis studies, and peripheral blood smear are performed. Elevated platelet count and thrombocytopenia are detected by platelet count; coagulation tests are usually normal unless there is a co-coagulopathy. A normal complete blood count, platelet count, INR, and normal or slightly prolonged PTT suggest platelet dysfunction.
In patients with thrombocytopenia, a peripheral blood smear may indicate a possible cause. If the smear shows other abnormalities besides thrombocytopenia, such as the presence of nucleated red blood cells and young forms of white blood cells, bone marrow aspiration is indicated.
Peripheral blood in thrombocytopenic diseases
Blood changes |
Terms and Conditions |
Normal red blood cells and white blood cells |
Idiopathic thrombocytopenic purpura, thrombocytopenia of pregnancy, HIV-associated thrombocytopenia, drug-induced thrombocytopenia, post-transfusion purpura |
Red blood cell fragmentation |
Thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, preeclampsia with DIC, metastatic carcinoma |
Abnormal white blood cells |
Immature cells or a large number of mature lymphocytes in leukemia. Low granulocyte count in aplastic anemia. Hypersegmented granulocytes in megaloblastic anemia |
Giant platelets (similar in size to red blood cells) |
Bernard-Soulier syndrome and other congenital thrombocytopenias |
Erythrocyte abnormalities, nucleated red blood cells, immature granulocytes |
Myelodysplasia |
Bone marrow aspirate examination can assess the number and appearance of megakaryocytes and can also identify other causes of bone marrow hematopoiesis failure. If the myelogram is normal but there is splenomegaly, the most likely cause of thrombocytopenia is platelet sequestration in the spleen; if the bone marrow and spleen size are normal, the most likely cause of thrombocytopenia is increased destruction. However, the determination of antiplatelet antibodies has no significant clinical significance. HIV testing is performed in patients with suspected HIV infection.
In patients with platelet dysfunction and a long history of increased bleeding after dental extraction, other surgical interventions, or easy formation of subcutaneous hemorrhages, there is reason to suspect a congenital pathology. In this case, it is necessary to determine the antigen and activity of the von Willebrand factor. If there is no doubt about the presence of congenital pathology, no further tests are performed.
What tests are needed?
Who to contact?
Treatment of thrombocytopenia
Patients with thrombocytopenia or platelet dysfunction should avoid medications that may impair platelet function, especially aspirin and other nonsteroidal anti-inflammatory drugs. Patients may require platelet transfusions, but only in specific situations. Prophylactic transfusions are rarely used because repeated transfusions may be ineffective due to the development of antiplatelet alloantibodies. In platelet dysfunction or thrombocytopenia due to defective platelet production, transfusions are reserved for active bleeding or severe thrombocytopenia (eg, platelet count < 10,000/μL). In thrombocytopenia due to platelet destruction, transfusions are reserved for life-threatening bleeding or CNS hemorrhage.
In modern hematology, etiological treatment of thrombocytopenia is carried out, taking into account the severity of the disease and the causes of its occurrence.
The administration of corticosteroids, which suppress the immune system and block platelet antibodies, is practiced. Prednisolone for autoimmune thrombocytopenia (orally or by injection) is used for mild to moderate thrombocytopenia; however, after dose reduction or discontinuation, relapses occur in 60-90% of patients.
Lithium carbonate or folic acid can be used in thrombocytopenia to stimulate platelet production by the bone marrow. Patients with idiopathic thrombocytopenia are given plasmapheresis and immunosuppressive drugs (Imuran, Mycophenolate mofetil, etc.).
Chronic idiopathic thrombocytopenia, especially when recurrent in splenectomized patients, is treated with the injectable drug Romiplostim, which is a thrombopoietin receptor agonist that stimulates platelet production.
Dicynone for thrombocytopenia (tablets and injection solution) can be used to treat capillary bleeding, since it is a drug of the hemostatic group. Its hemostatic effect is based on local activation of tissue coagulation factor III (thromboplastin).
Ascorutin, Curantil and Sodecor for thrombocytopenia
These three drugs are singled out separately for a reason. The complex of antioxidant vitamins - ascorbic acid and rutin - Ascorutin for thrombocytopenia is not listed in the list of recommended medications, although it has angioprotective properties, that is, it increases the impermeability of small vessels. Ascorutin is usually used in the complex therapy of varicose veins and thrombophlebitis of veins, chronic venous insufficiency, hypertensive microangiopathies, increased permeability of capillaries in hemorrhagic diathesis. Rutin provides a more complete effect of ascorbic acid, but, on the other hand, it reduces platelet aggregation, that is, prevents blood coagulation.
There is information that Curantil can be used for thrombocytopenia to "restore immunity", prevent thrombus formation and eliminate blood circulation disorders. However, this drug has nothing to do with immunity. Curantil is an angioprotective agent that is used to prevent thrombus formation and activate peripheral circulation. The antithrombotic effect of the drug is that it increases the ability of prostaglandin E1 (PgE1) to inhibit platelet aggregation. Among its side effects are thrombocytopenia and increased bleeding.
Also, some sites report that it is possible to normalize the platelet level by taking Sodekor tincture for thrombocytopenia. The composition of the water-alcohol solution contains extracts of rhizomes and roots of elecampane; dandelion roots, licorice and ginger; sea buckthorn fruits; pine nuts, as well as cinnamon bark, cardamom and coriander seeds, clove buds.
The pharmacodynamics of this herbal remedy are not presented, but according to the official description, the drug (we quote verbatim): "has an anti-inflammatory, general strengthening effect, increases the non-specific resistance of the body, helps to increase mental and physical performance." That is, there is not a word about the use of Sodekor for thrombocytopenia.
How do the tincture components work? Elecampane is used as an expectorant, antimicrobial, diuretic, choleretic and anthelmintic agent. Dandelion root is used for gastrointestinal diseases and constipation. Licorice root (licorice) is used for dry cough, as well as an antacid for gastritis and a diuretic for cystitis.
Cinnamon is useful for colds and nausea; cardamom has a tonic effect, and also increases the secretion of gastric juice and helps with flatulence. Ginger, the root of which is included in Sodekor, is very useful, but ginger will not help with thrombocytopenia, since it reduces blood clotting. Coriander seeds, containing the flavonoid rutoside, act similarly.
Folk remedies for thrombocytopenia
There are some folk remedies for thrombocytopenia. Thus, shark fat is a folk remedy for thrombocytopenia in Scandinavian countries, where it is sold in pharmacies in capsule form (take 4-5 capsules a day for a month). In our country, it can be successfully replaced by regular fish oil, which also contains polyunsaturated fatty acids (ω-3) - 1-2 capsules a day.
It is recommended to use raw pressed sesame oil for thrombocytopenia - a tablespoon twice a day. It is said that this oil has properties that increase the level of platelets. Apparently, this is possible due to the content of polyunsaturated fats (including ω-9), folic acid (25%) and vitamin K (22%), as well as amino acids such as L-arginine, leucine, alanine, valine, etc. Together, these biologically active substances contribute to normal metabolism and proliferation of bone marrow tissue and, thus, stimulate hematopoiesis.
Herbalists also recommend herbal treatment for thrombocytopenia, which you can read more about in a separate publication – Treatment of Thrombocytopenia
 [ 59 ], [ 60 ], [ 61 ], [ 62 ], [ 63 ]
[ 59 ], [ 60 ], [ 61 ], [ 62 ], [ 63 ]
Diet for thrombocytopenia
Thrombocytopenia does not require a special diet, but proper nutrition should be organized for thrombocytopenia. What does this mean?
It is enough to include more fruits and vegetables in your diet, especially green ones: cabbage, lettuce, parsley, green onions, kelp. They contain chlorophyll, and therefore a lot of vitamin K.
Useful products for thrombocytopenia: vegetable oils; low-fat dairy products (containing calcium, which works together with vitamin K); almonds and dried figs; oranges and orange juice (they contain enough vitamin B9); cereals, peas, lentils and beans (a source of vegetable protein); seafood and beets (rich in zinc).
Foods to avoid with thrombocytopenia include white rice, white sugar, and foods that are low in nutrients, fattening, and deficient in vitamins and minerals. And of course, alcohol should be avoided.
More information of the treatment
Prevention of thrombocytopenia
There are no specific methods for preventing thrombocytopenia. Do not forget about the importance of vitamins (they were discussed above).
But if this pathology is present, doctors recommend being careful at home and at work when using anything that could accidentally injure you. Men are better off shaving with an electric razor and avoiding contact sports and other activities that could lead to injuries. Children with low levels of platelets in the blood require special attention.

