Medical expert of the article
New publications
Thrombotic thrombocytopenic purpura in children
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
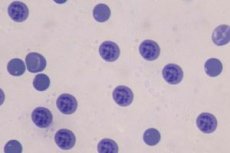
Idiopathic (autoimmune) thrombocytopenic purpura is a disease characterized by an isolated decrease in the number of platelets (less than 100,000/mm3 ) with a normal or increased number of megakaryocytes in the bone marrow and the presence of antiplatelet antibodies on the surface of platelets and in the blood serum, causing increased destruction of platelets.
Epidemiology
The incidence of idiopathic thrombocytopenic purpura in children is about 1.5-2 per 100,000 children, with no gender differences, and an equal incidence of acute and chronic forms. In adolescence, the number of sick girls becomes twice as large as that of boys.
Causes of thrombotic thrombocytopenic purpura in a child.
In children, thrombocytopenia can be caused by both hereditary and postnatal factors. Generally, the number of platelets decreases due to insufficient formation of platelets in the bone marrow from megakaryocytes, the progenitor cells; direct destruction in the bloodstream; or both.
Causes of insufficient platelet production:
- Changes in the progenitor cells (megakaryocytes) in the bone marrow in combination with a general disruption of the hematopoietic cycle and subsequent anomalies in the development of organs and systems.
- Tumors of the nervous system (neuroblastomas).
- Chromosomal diseases (Down, Edwards, Patau, Wiskott-Aldrich syndromes).
- Taking diuretics, antidiabetic, hormonal and nitrofuran drugs during pregnancy.
- Severe eclampsia and preeclampsia.
- Prematurity of the fetus.
The next cause of thrombocytopenia is the destruction of platelets.
This is caused by the following:
- Immunological pathologies.
- Changes in the structure of the vascular wall (antiphospholipid syndrome).
- Changes in the structure of platelets.
- Deficiency of blood clotting factors (hemophilia B).
- DIC syndrome.
Immunological causes are:
- direct: the production of antibodies to one's own platelets as a result of incompatibility between the mother and child in terms of the platelet index of the blood group (the mother's blood contains forms of platelets that the child does not have). These forms cause rejection of the "foreign" agent - destruction of the fetus's platelets and the development of thrombocytopenia.
- cross-linked: in cases of maternal diseases associated with autoimmune destruction of platelets, antibodies penetrating through the placenta into the fetus's body cause the same destruction of these blood cells in it.
- antigen-dependent: viral antigens interact with the surface receptors of platelets, changing their structure and causing self-destruction.
- autoimmune: production of antibodies to normal surface receptors.
Symptoms of thrombotic thrombocytopenic purpura in a child.
- Cutaneous manifestations (ecchymosis, petechiae – pinpoint hemorrhages) – always occur
- Gastrointestinal bleeding (melena, bloody diarrhea), bleeding from the umbilical cord remnant - occurs in 5% of cases
- Nosebleeds - about 30% of cases
- Hemorrhages into the eyeball membranes (prognostic probability of intracranial hemorrhages)
- Enlargement of the liver and spleen according to ultrasound data. Characteristic only of secondary thrombocytopenia (drug, viral)
Diagnostics of thrombotic thrombocytopenic purpura in a child.
- Blood
- Platelet count less than 150x10*9 g/l (normal 150-320 x 10*9 g/l)
- Duke's bleeding time
This indicator helps differentiate thrombocytopathy from hemophilia. After puncturing the fingertip with a scarifier, bleeding normally stops in 1.5-2 minutes. In thrombocytopathy, it continues for more than 4 minutes, while the coagulation function remains normal. In hemophilia, everything is the opposite.
- The formation (retraction) of a full-fledged blood clot by less than 45% (normally 45-60%) is an indicator that characterizes the number of platelets sufficient to stop bleeding.
- Myelogram: a detailed description of the number of all bone marrow cells, in particular the progenitor cells of platelets. Normally, the number of megakaryocytes is 0.3-0.5 per microliter. In thrombocytopathy, this figure increases to 114 in 1 μl of bone marrow substance. The life span of platelets is normally about 10 days. In diseases associated with their decrease in the blood, these cells live significantly less.
- Anamnesis
- Presence or tendency to autoimmune diseases in the mother
- Violation of placental functions during pregnancy (detachment, thrombosis)
- Fetal pathology (hypoxia, intrauterine growth retardation, prematurity; intrauterine infection)
- Immunological analysis
Detection of elevated levels of antibodies to one's own platelets or to certain infectious diseases (herpes virus type 1, cytomegalovirus, Epstein-Barr virus)
 [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ]
[ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ]
What tests are needed?
Who to contact?
Treatment of thrombotic thrombocytopenic purpura in a child.
Typically, 80% of children with thrombocytopenic purpura disappear within six months without any treatment. In this case, parents are required to follow several important rules in caring for the child in order to prevent the health condition from worsening:
- avoid traumatic sports (wrestling, gymnastics, cycling, skiing)
- use a soft toothbrush
- follow a diet to prevent constipation
- do not give your child blood thinners (aspirin)
During the treatment of thrombocytopenia, the child must be transferred to artificial feeding to prevent further immunization of the body with the mother's antiplatelet antibodies.
Medication or inpatient treatment is necessary in case of a critical decrease in the number of platelets to less than 20 thousand per microliter. In this case, the criterion for prescribing treatment procedures should be a pronounced clinical picture of thrombocytopenic syndrome: massive nasal, gastrointestinal bleeding, threatening the child's life.
Drug treatment
- Intravenous drip transfusion of platelet concentrate (washed platelets of the mother or antigen-compatible donor) at a dose of 10-30 ml/kg of weight. A positive effect of the transfusion will be considered to be stopping the child's bleeding, an increase in the number of platelets by 50-60x10*9/l 1 hour after the procedure and maintaining these indicators for 24 hours.
- Intravenous drip infusion of normal human immunoglobulin at a dose of 800 mcg/kg for 5 days. The following drugs are used as immunoglobulin: Immunovenin, Pentaglobin, Octagam. They give a faster but less stable effect compared to hormonal drugs (prednisolone).
- Hemostatic drugs
- intravenous drip infusion of aminocaproic acid at a dose of 50 mg/kg once a day
- Hormonal therapy
- oral prednisolone twice daily at a dose of 2 mg/kg
Surgical treatment
Surgical treatment means splenectomy – removal of the spleen. This operation is indicated only if hormonal therapy is ineffective. It is also necessary to take into account the fact that prednisolone should still lead to some increase in the number of platelets, otherwise the operation will not have a significant effect on the main cause of the disease. After splenectomy, the number of platelets may remain low, but despite this, the hemorrhagic syndrome completely disappears.
New methods in the treatment of thrombocytopenia in children
- Blood coagulation factor VIIa (Novoseven)
- Ethrombopag is a thrombopoietin receptor antagonist.
- Rituximab is a monoclonal cell-mediated agent
These substances are intensively studied in laboratories around the world. To date, their effect has been partially studied in relation to the adult organism. In clinical pediatrics, their effect on the child's organism has no evidence-based practical basis.
More information of the treatment
Forecast
As mentioned earlier, thrombocytopenic purpura often enters a stage of spontaneous long-term remission and requires only regular monitoring of blood counts. It is carried out after the improvement of the general condition and the disappearance of clinical symptoms of thrombocytopenia after 1 and 6 weeks, then after 3 and 6 months.
In the absence of severe hemorrhagic complications of thrombocytopenia in the brain, the prognosis of the disease is generally favorable.
Использованная литература

