Medical expert of the article
New publications
T-cell lymphomas of the skin
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Most often, T-cell lymphomas are registered in elderly people, although isolated cases of the disease are noted even in children. Men are sick twice as often as women. T-cell lymphomas are epidermotropic in nature.
Causes T-cell lymphomas of the skin
The causes and pathogenesis of cutaneous T-cell lymphomas are not fully understood. Currently, most researchers consider human T-cell leukemia virus type 1 (HTLV-1) I as the main etiologic factor initiating the development of malignant T-cell lymphomas of the skin. Along with this, the role of other viruses in the development of T-cell lymphoma is discussed: Epstein-Barr virus, herpes simplex type 6. In patients with T-cell lymphoma, viruses are found in the skin, peripheral blood, and Langerhans cells. Antibodies to HTLV-I are detected in many patients with mycosis fungoides.
An important place in the pathogenesis of T-cell lymphomas is played by immunopathological processes in the skin, the main one of which is the uncontrolled proliferation of clonal lymphocytes.
Cytokines produced by lymphocytes, epithelial cells and cells of the macrophage system have proinflammatory and proliferative effects (IL-1, responsible for lymphocyte differentiation; IL-2 - T-cell growth factor; IL-4 and IL-5, increasing the influx of eosinophils into the lesion and their activation, etc.). As a result of the influx of T-lymphocytes into the lesion, Pautrier microabscesses are formed. Simultaneously with the increase in lymphocyte proliferation, the activity of antitumor defense cells is suppressed: natural killers, lymphocytotoxic lymphocytes, dendritic cells, in particular, Langerhans cells, as well as cytokines (IL-7, IL-15, etc.) - tumor growth inhibitors. The role of hereditary factors cannot be ruled out. The presence of familial cases, frequent detection of some histocompatibility antigens (HLA B-5 and HLA B-35 - in highly malignant skin lymphomas, HLA A-10 - in less aggressive lymphomas, HLA B-8 - in the erythrodermic form of mycosis fungoides) confirm the hereditary nature of the dermatosis.
Clinical observations indicate a possible transformation of long-term chronic dermatoses (neurodermatitis, atopic dermatitis, psoriasis, etc.) into mycosis fungoides. The key factor is the long-term persistence of lymphocytes in the inflammation focus, which disrupt immune surveillance and promote the emergence of a clone of malignant lymphocytes and, thus, the development of a malignant proliferative process.
The impact of physical factors on the body, such as insolation, ionizing radiation, and chemical substances, can lead to the emergence of a clone of “genotraumatic” lymphocytes that have a mutagenic effect on lymphoid cells and the development of lymphocyte malignancy.
Therefore, T-cell lymphomas can be considered as a multifactorial disease that begins with the activation of lymphocytes under the influence of various carcinogenic, "genotraumatizing" factors and the emergence of a dominant T-cell clone. The severity of the immune surveillance disorder, the clone of malignant lymphocytes determines the clinical manifestations (spotted, plaque or tumor elements) of T-cell lymphomas.
Pathogenesis
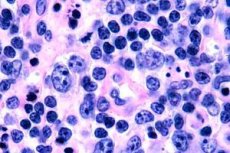
In the early stage of mycosis fungoides, acanthosis with wide processes, hyperplasia and compaction of basal keratinocytes, vacuolar degeneration of some basal cells, atypical mitoses in different layers of the epidermis, epidermotropism of the infiltrate with penetration of lymphocytes into the epidermis are observed. In the dermis, small infiltrates are observed around the vessels, consisting of single mononuclear cells with hyperchromic nuclei - "mycotic" cells. In the second stage, an increase in the severity of the dermal infiltrate and epidermotropism of the infiltrate cells are observed, as a result of which malignant lymphocytes penetrate the epidermis, forming clusters in the form of Potrier's microabscesses. In the third, tumor stage, massive acanthosis and minor atrophy of the epidermis are observed, as well as increased infiltration of the epidermis by tumor lymphocytes, which form multiple Potrier microabscesses. The massive infiltrate is located throughout the entire thickness of the dermis and covers part of the hypodermis. Blast forms of lymphocytes are observed.
Cutaneous large anaplastic T-cell lymphoma
It is represented by a group of lymphoproliferative processes characterized by the presence of proliferates from atypical clonal large anaplastic CD30+ T cells. As a rule, it develops secondarily in the tumor stage of mycosis fungoides or in Sezary syndrome, but can develop independently or with dissemination of systemic lymphomas of this type. Clinically, such lymphomas correspond to the so-called decapitated form of mycosis fungoides in the form of single or multiple nodes, usually grouped.
Histologically, the proliferate occupies almost the entire dermis with or without epidermotropism in the case of epidermal atrophy.
Cytologically, tumor cells may vary in size and shape. Based on these properties, a distinction is made between medium- and large-cell pleomorphic T-cell lymphoma with nuclei of various irregular configurations - convoluted, multilobed, with dense chromatin, a well-defined nucleolus, and fairly abundant cytoplasm; immunoblastic - with large round or oval nuclei with clear karyoplasm and one centrally located nucleolus; anaplastic - with ugly very large cells with nuclei of irregular configuration and abundant cytoplasm. Phenotypically, this entire group belongs to T-helper lymphomas and can be CD30+ or CD30-.
R. Willemze et al. (1994) showed that the course of CD30+ lymphoma is more favorable. Genotypically, clonal rearrangement of the T-lymphocyte receptor is detected.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
Symptoms T-cell lymphomas of the skin
The most common disease in the group of T-cell lymphomas of the skin is mycosis fungoides, which accounts for about 70% of cases. There are three clinical forms of the disease: classical, erythrodermic and beheaded. T-cell lymphomas are characterized by polymorphism of rashes in the form of spots, plaques, tumors.
The erythrodermic form of mycosis fungoides usually begins with uncontrollable itching, swelling, universal hyperemia, the appearance of erythematous-squamous lesions on the skin of the trunk and extremities, which tend to merge and develop erythroderma within 1-2 months. Almost all patients have palmar-plantar hyperkeratosis and diffuse thinning of hair over the entire skin. All groups of lymph nodes are greatly enlarged. Enlarged inguinal, femoral, axillary, cubital lymph nodes are palpated as "packets" of dense elastic consistency, not fused with surrounding tissues, painless. The general condition deteriorates sharply: fever with a body temperature of up to 38-39 ° C, night sweats, weakness and weight loss occur. Currently, Sezary syndrome is considered by many dermatologists to be the rarest leukemic variant of the erythrodermic form of mycosis fungoides,
A pronounced leukocytosis is noted in lymphocytograms - Sezary cells. Sezary cells are malignant T-helpers, the nuclei of which have a folded cerebriform surface with deep invaginations of the nuclear membrane. A fatal outcome is noted after 2-5 years, the frequent cause of which is cardiovascular pathology and intoxication.
The decapitated form of mycosis fungoides is characterized by the rapid development of tumor-like lesions on apparently healthy skin without previous long-term plaque formation. This form is characterized by a high degree of malignancy, which is considered a manifestation of lymphosarcoma. A fatal outcome is observed within a year.
Stages
The classic form of mycosis fungoides is characterized by three stages of development: erythematous-squamous, plaque and tumor.
The first stage resembles the clinical picture of some benign inflammatory dermatoses - eczema, seborrheic dermatitis, plaque parapsoriasis. At this stage of the disease, spots of various sizes are observed, intensely pink, pink-red with a purple tint, round or oval outlines, with relatively clear boundaries, superficial bran-like or fine-plate peeling. The elements are often located on different areas of the skin, most often on the trunk and face. Gradually, their number increases. Over time, the process can take on the character of erythroderma (erythrodermic stage). The rash can exist for years or spontaneously disappear. Unlike benign inflammatory dermatoses, the elements of the rash and itching at this stage are resistant to the therapy.
The infiltrative-plaque stage develops over several years. In place of previously existing spotted rashes, plaques of round or irregular outlines appear, intensely purple in color, clearly demarcated from healthy skin, dense, with a flaky surface. Their consistency resembles "thick cardboard". Some of them spontaneously resolve, leaving areas of dark-brown hyperpigmentation and/or atrophy (poikiloderma). Itching at this stage is even more intense and painful, fever and weight loss are observed. Lymphadenopathy may be observed at this stage.
In the third, tumor stage, painless tumors of a dense, elastic consistency, yellow-red color, developing from plaques or arising on apparently healthy skin, appear. The shape of the tumors is spherical or flattened, often resembling a mushroom cap. Tumors can appear anywhere. Their number varies widely from single to dozens, sizes - from 1 to 20 cm in diameter. When long-existing tumors disintegrate, ulcers with uneven edges and a deep bottom are formed, reaching the fascia or bone. The lymph nodes, spleen, liver and lungs are most often affected. The general condition worsens, intoxication symptoms appear and increase, weakness develops. The average life expectancy of patients with the classic form of mycosis fungoides from the moment of diagnosis is from 5 to 10 years. Mortality is usually observed from intercurrent diseases: pneumonia, cardiovascular failure, amyloidosis. Subjectively, itching is felt, and when tumors disintegrate, pain in the affected areas.
What do need to examine?
How to examine?
Treatment T-cell lymphomas of the skin
At the erythematous-squamous stage, patients do not need antitumor therapy; they are prescribed topical corticosteroids (prednisolone, betamethasone, dexamethasone derivatives), interferon alpha (3 million IU daily, then 3 times a week for 3-6 months depending on clinical manifestations or treatment effectiveness), interferon gamma (100,000 IU per day for 10 days, the cycle is repeated 12-3 times with a 10-day break), PUVA therapy or Re-PUVA therapy. The effectiveness of PUVA therapy is based on the selective formation of covalent cross-links of psoralens with DNA in proliferating T-helper cells, which inhibits their division. In the second stage, in addition to the above-mentioned agents, systemic corticosteroids (30-40 mg per day of prednisolone for 1.5-2 months) and cytostatics (prospedin 100 mg per day daily, 4-5 injections in total) are used. Combining interferons with other methods of therapy has a more pronounced therapeutic effect (interferons + PUVA, interferons + cytostatics, interferons + aromatic retinoids).
In the tumor stage, the main method is polychemotherapy. A combination of vincristine (0.5-1 mg intravenously once a day, a total of 4-5 injections) with prednisolone (40-60 mg per day orally during chemotherapy), prospidin (100 mg per day, a total of 3 g), and interferons is used. Photodynamic, electron beam therapy, and photopheresis (extracorporeal photochemotherapy) are recommended.

