Medical expert of the article
New publications
Synovial chondromatosis of the joints
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
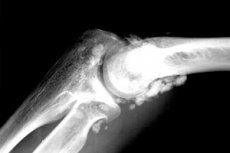
There are many diseases of the musculoskeletal system and connective tissue, and these include synovial chondromatosis, which is a lesion of the inner synovial membrane of the fibrous capsule of the joints (joint bag) in the form of benign chondrogenic metaplasia. [ 1 ]
Synovial chondromatosis (from the Greek chondros – cartilage) is also called synovial osteochondromatosis, coral joint or Lotsch syndrome, Henderson-Jones syndrome and Reichel's disease. [ 2 ]
Epidemiology
As already noted, this pathology is rarely detected, and in comparison with other joint diseases, its frequency, according to some data, does not exceed 6.5%. The ratio of men and women among patients is 3:1.
Secondary synovial chondromatosis is more common than primary. It mainly affects large joints and, as a rule, the articulations of the right limbs.
The most common (up to 65-70% of cases) is chondromatosis of the knee joint; in second place is chondromatosis of the elbow joint (which is often bilateral); the third most common is chondromatosis of the hip joint, followed by chondromatosis of the shoulder joint.
Chondromatosis of the ankle joint is very rare. But synovial chondromatosis of the TMJ (temporomandibular joint) is detected least often, in isolated cases.
Causes synovial chondromatosis
This disease is considered to be quite rare, and its causes have not yet been determined. But they are associated with both genetically determined disorders of intra-articular cartilage formation and with local pathological changes in cartilage tissue during natural regeneration - with joint injuries (especially osteochondral fractures), inflammatory damage, chronic joint diseases of a degenerative-dystrophic nature, as well as with constant excessive loads on synovial joints (leading to deformation of their structures and destruction of the articular surface). [ 3 ]
There is a correlation between damage to the synovial membrane of the joint and pronounced age-related features of the metabolism of hyaline cartilage tissue, since the pathology is most often detected in adults, starting from 40 years of age and older. [ 4 ]
Read - Development and age-related features of bone connection in ontogenesis
In addition, possible risk factors for the development of this pathology may be of an endocrine nature, since, as is known, the condition of cartilaginous tissue is affected by a number of human hormones (steroid, thyroid-stimulating, pituitary). [ 5 ]
Pathogenesis
Explaining the pathogenesis of synovial chondromatosis, specialists emphasize the key importance of structural changes in cartilage tissue: focal metaplastic transformation, as well as proliferation (growth) of connective tissue, that is, increased mitosis of its cells.
As a result, at the initial stage, spherical cartilaginous (chondral) nodules are formed in the synovial membrane of the joint or in the connective tissue tendon sheath, which are called cartilaginous intra-articular bodies. They consist of larger and more densely grouped hyaline cartilage cells (fibroblasts and chondroblasts). [ 6 ]
At the next stage, the nodules separate from the inner lining of the joint capsule, freely moving in the synovial fluid and receiving nutrients from it by diffusion. In fact, this is a type of free inclusions in the joint cavity - the so-called "joint mice" (as they were previously called because of their rapid movement, reminiscent of a running mouse).
Over time, the cartilaginous bodies increase in size, and in 75-95% of cases, their endochondral calcification and ossification (ossification) occur. As it turned out, in synovial chondromatosis, the level of chondrocalcin in the intra-articular fluid is significantly increased - a polypeptide produced by cartilaginous tissue cells (chondrocytes), which binds calcium and participates both in the formation of the epiphyseal plate of hyaline cartilage and in its destruction. [ 7 ]
In particularly severe cases, the entire joint space can be filled with bone-cartilaginous bodies, which can penetrate into the surrounding tissues.
Symptoms synovial chondromatosis
At the initial stage, the pathological process is asymptomatic, and the first signs - in the form of pain in the joint when palpated - appear when ossification of the cartilaginous bodies occurs.
Further clinical symptoms are manifested by dull pain in the joint (at first only during movement, and then also at rest), its swelling and hyperthermia of the skin over the affected joint. Its mobility is significantly reduced (patients complain of joint stiffness), and movements may be accompanied by crepitus (crunching). [ 8 ]
Forms
Clinicians divide synovial chondromatosis into primary and secondary. Primary is considered idiopathic - of unknown origin, and secondary is the result of trauma or degenerative changes in articular cartilage in osteoarthrosis. According to many orthopedists and rheumatologists, secondary synovial osteochondromatosis is a late complication of the primary form of pathology, for example, it is usually present in arthritis.
Synovial chondromatosis of the tendon sheath or bursa, identical to the primary form of pathology, can be defined as tenosynovial or bursal. Extra-articular localization of pathology is usually observed in the upper limbs, in particular, in the wrist. In this case, cartilaginous nodules are painful only on palpation and very rarely affect movement.
Multiple chondromatosis means multiple intra-articular or periarticular cartilaginous bodies.
Complications and consequences
Possible complications include complete blocking of the affected joint with the development of its contracture and a gradual decrease in the tone of the periarticular muscles.
The consequence of primary synovial osteochondromatosis may be inflammation of the synovial membrane of the joint - reactive synovitis or secondary deforming arthrosis (osteoarthrosis) with intense joint pain.
There is a risk of primary synovial chondromatosis degenerating into chondrosarcoma. However, as experts note, it is possible to misdiagnose malignant transformation due to the presence of atypical cells, which is characteristic of benign chondrogenic metaplasia.
Diagnostics synovial chondromatosis
Standard diagnostics of joints is carried out, where visualization plays a key role, since clinical symptoms are non-specific, and laboratory tests - except for a general clinical analysis of synovial fluid and a biopsy of the synovial membrane tissue of the joint capsule - are absent. [ 9 ]
Only instrumental diagnostics can visualize cartilaginous nodules in the joint capsule: ultrasound of the joints, contrast radiography - arthrography of the joints, magnetic resonance imaging (MRI). [ 10 ]
Conventional X-rays can only show calcified chondral bodies, and when they ossify, the radiographic signs consist of displaying a certain number of oval/round bodies with clear outlines in the bursa or joint. Narrowing of the intra-articular space and degenerative changes in the articular surfaces (in the form of subchondral sclerosis, the presence of osteophytes, erosion of the articular surface in the form of a depression) can also be displayed. [ 11 ], [ 12 ]
More information in the article – X-ray signs of bone and joint diseases
Differential diagnosis
Differential diagnostics of synovial chondromatosis should include: synovitis, including pigmented villonodular (villous-nodular); tendosynovitis; synovial hemangioma; osteoarthrosis; periarticular tumor calcinosis and periarticular melorheostosis (Lery's disease). And, of course, chondrosarcoma, since, according to clinical observations, the degree of cellular atypia in synovial chondromatosis may be higher than in chondrosarcoma.
In addition, it is necessary to differentiate between cartilaginous nodes in synovial chondromatosis and smaller fibrinous rice bodies that form in the joint capsule in rheumatoid arthritis, tuberculosis of the joints or chronic bursitis.
Who to contact?
Treatment synovial chondromatosis
Only surgical treatment, which is performed using arthroscopy or arthrotomy (opening of the joint cavity), can free the capsule surrounding the joint from the bone-cartilaginous bodies. But postoperative relapses are observed in almost 23% of cases.
Partial or total synovectomy – surgical excision of the synovial membrane by open means – is most often resorted to if chondrogenic metaplasia of the synovial membrane is recurrent and persistent. [ 13 ]
After surgical interventions, physiotherapy treatment is prescribed for the functional restoration of the joint. [ 14 ] More details in the publication - Physiotherapy for joint diseases
Prevention
There are no specific measures for the prevention of focal metaplastic transformation of cartilage tissue.
Doctors advise avoiding injuries, metering the load on synovial joints and eating foods to restore cartilage, joints and ligaments.
Forecast
The long-term prognosis for patients with synovial chondromatosis depends directly on the affected joint, the extent of its damage, and recurrence of the disease after surgical treatment. Periodic examinations will be required to prevent recurrence of cartilaginous metaplasia or the development of osteoarthritis.

