Medical expert of the article
New publications
Pulmonary thickening syndrome
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
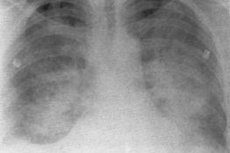
Pulmonary consolidation syndrome is one of the most pronounced manifestations of pulmonary diseases. Its essence consists in a significant decrease or complete disappearance of the airiness of the lung tissue in a more or less widespread area (segment, lobe, several lobes at the same time). The foci of consolidation differ in localization (lower areas, apices of the lungs, middle lobe, etc.), which also has differential diagnostic significance; subpleural localization of the consolidation focus with the involvement of the visceral and concomitantly parietal pleural layers is specially distinguished, which is accompanied by the addition of signs of pleural syndrome. The development of consolidation can occur quite quickly ( acute pneumonia, pulmonary infarction ) or gradually ( tumor, atelectasis ).
There are several types of pulmonary consolidation: infiltrate (pneumonic focus) with the release of a tuberculous infiltrate prone to caseous decay; pulmonary infarction due to thromboembolism or local vascular thrombosis; obstructive (segmental or lobar) and compression atelectasis (collapse of the lung) and hypoventilation; a variant of atelectasis is hypoventilation of the middle lobe due to obstruction of the middle lobe bronchus (bronchopulmonary lymph nodes, fibrous tissue), which, as is known, does not adequately ventilate the lobe even under normal conditions - middle lobe syndrome; lung tumor; congestive heart failure.
Subjective manifestations of pulmonary consolidation syndrome vary depending on the nature of the consolidation and are considered when describing the corresponding diseases.
A common objective sign of a developing decrease in the airiness of the corresponding compacted area of lung tissue is the asymmetry of the chest, revealed during examination and palpation.
Regardless of the nature of this syndrome, with large foci of compaction and their superficial location, bulging and lagging during breathing of this area of the chest can be detected (and only with large obstructive atelectasis is its retraction possible), vocal fremitus is increased. Percussion reveals dullness (or absolute dullness) in the area of compaction, and in the presence of an infiltrate (pneumonia), at the initial stage and during the period of resorption, when the alveoli are partially free of exudate, and the draining bronchi retain complete patency (and therefore contain air), dullness is combined with a tympanic shade of percussion sound. The same dull-tympanic shade during percussion is noted at the initial stage of atelectasis development, when there is still air in the alveoli and communication with the afferent bronchus is preserved. Later, with complete resorption of air, a dull percussion sound appears. A dull percussion sound is also noted above the tumor node.
During auscultation in the infiltrate zone at the initial and final stages of inflammation, when there is little exudate in the alveoli and they straighten out when air enters, weakened vesicular breathing and crepitation are heard. At the height of pneumonia, due to the filling of the alveoli with exudate, vesicular breathing disappears and is replaced by bronchial breathing. The same auscultatory picture is noted in pulmonary infarction. With any atelectasis at the initial stage (hypoventilation), when there is still slight ventilation of the alveoli in the collapse zone, weakening of vesicular breathing is noted. Then, after the air is absorbed in the case of compression atelectasis (compression of the lung from the outside by liquid or gas in the pleural cavity, a tumor, with a high position of the diaphragm), bronchial breathing is heard: the bronchus that remains passable for air conducts bronchial breathing, which spreads to the periphery by a compacted compressed area of the lung. In case of obstructive atelectasis (reduction of the lumen of the afferent bronchus by an endobronchial tumor, foreign body, its compression from the outside) at the stage of complete blockage of the bronchus above the airless zone, no breathing will be heard. Breathing will also not be heard above the tumor area. Bronchophony in all types of compactions repeats the patterns revealed by determining vocal fremitus.
During auscultation, pleural friction noise is detected over subpleurally located infiltrates and tumors, as well as in pulmonary infarction.
Since bronchi are often involved in the process with various types of compaction, moist rales of different calibers can be detected. Of particular diagnostic importance is listening to fine-bubble sonorous rales, indicating the presence of an infiltration zone around the small bronchi, which amplifies the sound vibrations arising in the bronchi.
In case of heart failure, a decrease in the airiness of the lung tissue is revealed, primarily in the lower parts of the lungs on both sides, which is associated with blood stagnation in the pulmonary circulation. This is accompanied by a shortening of the percussion sound, sometimes with a tympanic tint, a decrease in the excursion of the lower edge of the lungs, weakening of vesicular breathing, the appearance of moist fine-bubble wheezing, and sometimes crepitations.

