Medical expert of the article
New publications
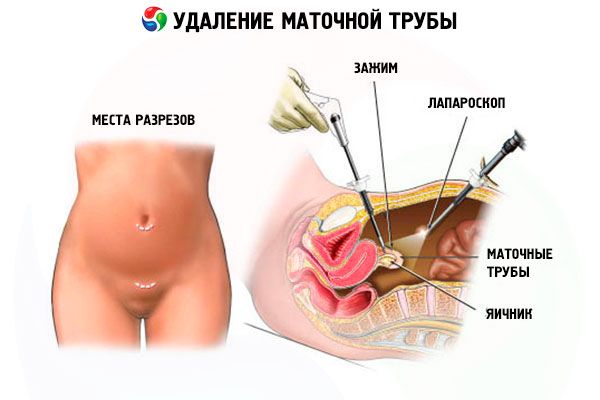
Surgery to remove the fallopian tube: consequences and rehabilitation
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

In terms of frequency of ectomies in gynecology, the uterine appendages are in the lead, and removal of the fallopian tube (tubectomy or salpingectomy) is in second place after removal of the ovaries.
The first such radical surgical intervention, which saved the life of a patient with bleeding during an ectopic pregnancy, was performed in 1883 by the Scottish surgeon Robert Lawson Tate.
 [ 1 ]
[ 1 ]
Indications for the procedure
The main indications for performing a fallopian tube removal include removal of the tube in case of an ectopic pregnancy: when bleeding occurs after salpingotomy (surgery to remove a tubal pregnancy while preserving the tube); in case of perforation of the fallopian tube due to a violation of a pathological pregnancy (tubal abortion); when the size of the ovum in the tube is more than 3.5-4 cm; in cases of repeated ectopic pregnancy in the same tube.
If conservative therapy does not give positive results, removal of the fallopian tubes may be performed in case of inflammation of their tissues - salpingitis, and in cases of purulent salpingitis, the fallopian tube where purulent exudate has accumulated is removed in most patients, as in the case of pyosalpinx and tubo-ovarian abscess.
Salpingitis can provoke an inflammatory process in the ovary, and then gynecologists diagnose inflammation of the appendages - adnexitis or salpingo-oophoritis, threatening either an ectopic pregnancy or irreversible dysfunction of the appendages leading to infertility. And the way out of the situation can be laparotomic or laparoscopic removal of the ovary and fallopian tube.
With adhesions between the ovary and the tube, the tube is often stretched, and the fluid secreted by the mucous membrane accumulates in this place, developing a chronic pathology - hydrosalpinx. The fluid often contains pus, and if this cavity ruptures, the woman is really at risk of peritonitis. In addition, as a result of hydrosalpinx, obstruction of the fallopian tubes develops, which is one of the most common causes of female infertility. Removal of the tube with hydrosalpinx, undertaken in such situations, increases the frequency of pregnancy after in vitro fertilization and reduces the risk of pregnancy outside the uterine cavity. Therefore, a protocol for IVF after removal of the tubes (both) has been developed.
By the way, the removal of adhesions in the fallopian tubes, which make women infertile, can be carried out by tubectomy - provided that all other methods of separating the overgrown fibrous strands have been unsuccessful.
Among the indications for performing this operation by laparotomy, it is necessary to note tuberculosis of the appendages, uterine fibroids, ovarian cancer and intraepithelial cancer of the fallopian tubes.
Removal of the hydatid of the fallopian tube - a subserous cyst - is performed in cases of twisting of its stalk, and removal of the entire tube may be necessary only if these cysts are of significant size and there are multiple adhesions localized around them.
In recent years, evidence has been obtained linking the development of most serous ovarian carcinomas with the fallopian tubes. As a result, recommendations have emerged for the use of prophylactic salpingectomy (opportunistic salpingectomy) in patients with hereditary mutations of the BRCA1 and BRCA2 genes – in order to prevent the development of ovarian cancer. According to the International Journal of Obstetrics & Gynaecolog, unilateral removal of the tube reduces the risk of ovarian cancer in this category of women by 29%, and removal of both fallopian tubes – by 65%.
Technique fallopian tube removal
Many sources describe the technique of performing laparoscopic removal of the fallopian tube.
This operation is performed under general anesthesia, and if endotracheal anesthesia is contraindicated, regional epidural anesthesia is used.
In the outer wall of the abdominal cavity - near the navel, above the pubis and at the bottom (on the side opposite the tube being removed) - three punctures (apertures) are made to install trocars through which the surgeon will insert the necessary laparoscopic instruments and the endoscope itself (which displays an image of the internal organs on the monitor). To provide space for manipulation, carbon dioxide or oxygen is pumped into the abdominal cavity (this is called pneumoperitoneum), and the blood is removed by suction.
On the operating table, the patient lies on her back, but after the blood is aspirated, the lower part of the body, in particular the pelvis, is raised by 45°, giving the so-called Trendelenburg position, which is optimal for surgical interventions on the pelvic organs. The tube to be excised is clamped as close as possible to the place of cutting (near the junction with the uterus), stretched and cut off with a bipolar coagulator, forceps or laparoscopic scissors with simultaneous monopolar coagulation. Then coagulation and cutting off of the upper part of the broad ligament of the uterus (mesosalpinx) and the isthmus of the tube are performed with the application of ligatures. After which the cut fallopian tube is removed through the largest trocar.
If a tube is removed due to an ectopic pregnancy, an examination of the upper abdominal cavity and thorough sanitization of the entire cavity with antiseptics is performed.
After the trocars are removed, small sutures are placed after the tube is removed.
Contraindications to the procedure
Today, fallopian tube removal surgery is performed either by laparotomy – with access through axial layer-by-layer dissection of the abdominal wall (with an incision length of up to 12 cm) and an open surgical field, or by the laparoscopic method – through three small incisions using an endoscope and electrosurgical instruments inserted into the cavity. The choice of the type of surgical intervention depends on many factors, but the use of laparoscopy – despite its obvious advantages in terms of the degree of trauma, complications, postoperative scars and the speed of recovery of patients – has certain medical contraindications.
Laparoscopic removal of the fallopian tube is contraindicated in the development of peritonitis; in case of rupture of the fallopian tube with severe bleeding; in acute cardiovascular conditions (stroke, heart attack) and circulatory hypoxia; in case of diagnosed cancer of the appendages or uterus; in case of second-third degree obesity and decompensated diabetes mellitus.
Thus, patients with the listed medical contraindications undergo laparotomic removal of the fallopian tube.
Regardless of the surgical technique, preparation for it includes an ultrasound examination of the uterus, fallopian tubes and ovaries (as well as all organs located in the pelvic area); general and biochemical blood tests (including platelet levels); blood testing for viral hepatitis and HIV; electrocardiography (ECG).
Consequences after the procedure
Since restoration of the fallopian tubes after removal is impossible, the main consequence of such surgical intervention is a decrease in fertility: when one tube is removed, the possibility of becoming pregnant is reduced by half, and with bilateral tubectomy, the possibility of natural pregnancy is completely excluded, and the only way to have a child is IVF technology.
Additionally, if one fallopian tube remains and the other is removed due to an ectopic pregnancy, the risk that the pregnancy after the tube is removed will again be ectopic (outside the uterus) is significantly increased.
It should be borne in mind that regular menstruation after tube removal is restored differently in each patient, and menstrual cycle irregularities are often noted due to problems with ovulation and the functioning of the ovary on the side of the removed tube.
As gynecologists note, the most noticeable consequences of fallopian tube removal occur in women who have had both fallopian tubes removed. Headaches, tachycardia, hot flashes and hyperhidrosis, enlargement of the thyroid and mammary glands are possible.
 [ 7 ]
[ 7 ]
Complications after the procedure
Surgery to remove the fallopian tube may have complications in the form of secondary infection and the development of inflammation, as evidenced by an elevated temperature after removal of the tube.
Intra-tissue hematomas may appear in the subcutaneous tissue, and as a result of damage to the mesenteric vessels and their insufficient coagulation during surgery, hidden intra-abdominal bleeding may occur after removal of the tubes.
Because of anesthesia, patients may feel sick, and there may be vomiting for two or three days. And among the complications of pneumoperitoneum, surgeons name gas accumulation in tissues (emphysema), hematoma of the abdominal wall, and bleeding.
There may also be minor bloody discharge for several days after the fallopian tube has been removed, especially if it has ruptured due to a tubal pregnancy. This is associated with blood entering the uterine cavity during surgery.
Postoperative adhesions after tube removal occur not only during laparotomy, but also during laparoscopic method. And often a sign of adhesion formation is pain after tube removal, however, they can also be caused by cystic formation of the ovary, disturbed during surgery. As doctors note, over time, adhesions in the small pelvis can grow and intestinal adhesions appear, which can negatively affect its patency. In addition, they can be involved in the fact that women have pain in the lower abdomen after tube removal.
Care after the procedure
The rehabilitation period after tubectomy can last up to two to three months, although sick leave after removal of the fallopian tubes is given from the day of admission to a medical institution (the length of stay in the hospital usually does not exceed one week) for no more than a month (depending on the reason for the operation, its complexity and the patient's condition).
As a rule, a course of antibiotics, subcutaneous injections of aloe extract (1 ml per day for two weeks), and the use of Longidazay vaginal suppositories (one suppository every three days) are prescribed.
Physiotherapy after tube removal includes electrophoresis sessions with iodine and zinc (standard course – 20 procedures). Moderate physical activity (quiet walking) is mandatory – to prevent adhesions from forming.
Care for stitches after laparoscopic surgery consists of preventing their infection, so the doctor's recommendations after removal of the fallopian tube: observe hygiene rules, but refuse baths and take a shower (covering the stitches from water). Doctors also advise wearing compression underwear for at least a month after the operation.
Also, sexual activity should be stopped for a month after the removal of the tube, and then (if one tube is removed) birth control pills should be taken for about six months (after the first full menstruation).
No special diet is required after tube removal, but constipation and bloating (flatulence) should be avoided. In this regard, it is necessary to temporarily exclude the consumption of carbonated drinks, legumes, cabbage, cereal dishes, red meat, fresh yeast bread and pastries, sweet fruits, and whole milk.
 [ 11 ]
[ 11 ]

