Medical expert of the article
New publications
Cardiac stenting: life after surgery, rehabilitation, nutrition and diet
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

One of the methods used in endovascular surgery to expand the lumen of the coronary arteries in case of their atherosclerotic stenosis or occlusion is cardiac stenting, or more precisely, stenting of the heart vessels.
This is myocardial revascularization by installing a special frame inside the coronary arteries – a stent, which is a cylindrical mesh structure made of biocompatible and non-corrosive metals, alloys or polymeric materials. By exerting mechanical pressure on the vascular wall, the stent supports it, restoring the internal diameter of the vessel and hemodynamics. As a result, coronary blood flow is normalized and full trophism of the myocardium is ensured.
Indications for the procedure
The main indications for this endovascular intervention are vascular narrowing due to atheromatous deposits on their inner walls, which are characteristic of atherosclerosis. This leads to insufficient blood supply to the myocardium and oxygen starvation of its cells (ischemia). To solve this problem, cardiac stenting is performed in cases of ischemic heart disease and stable angina, arteriosclerosis of the coronary arteries of the heart, as well as in cases of atherosclerotic lesions of the coronary vessels in systemic vasculitis. However, stenting is performed if drug therapy fails to reduce the intensity of ischemia symptoms and stabilize the condition.
Coronary stenting of the heart vessels – that is, stenting of the coronary arteries – is performed on patients with a high risk of myocardial infarction. An intravascular stent can be implanted urgently: directly during a heart attack (in the first few hours after its onset). And to minimize the likelihood of developing repeated acute ischemia with the threat of cardiogenic shock and to restore the functions of the heart muscle, stenting of the heart after a heart attack is performed.
In addition, stenting is used when a patient who has previously undergone balloon angioplasty of the coronary artery or its bypass grafting experiences a new narrowing of the vessel.
As experts note, in cases of coarctation of the aorta (congenital heart defect), aortic stenting is performed even on infants.
Preparation
In preparation for stenting of the heart vessels, patients with the corresponding diagnoses undergo blood tests: clinical, biochemical, coagulogram; undergo chest X-ray, electrocardiography, and ultrasound of the heart.
To decide whether stenting is necessary, coronary angiography is mandatory: based on the data from this examination, individual anatomical features of the vascular system of the heart are identified, the exact location of the vessel stenosis and its degree are determined.
However, without iodine-containing radiographic contrast agents, coronary angiography of the heart cannot be performed, and this examination can result in complications such as a reaction to the contrast agent (in more than 10% of cases), cardiac arrhythmia and ventricular fibrillation with a fatal outcome (in 0.1% of cases).
It should be noted that coronary angiography is not recommended in febrile conditions, with a history of hypertension, renal failure, diabetes mellitus, hyperthyroidism, sickle cell anemia, myeloma, thrombocytosis or hypokalemia; this procedure is not recommended for the elderly.
In complex cases, intravascular ultrasound (visualizing the vessel wall and providing an idea of the size, quantity and morphology of atherosclerotic plaques) or optical coherence tomography is performed.
Sometimes, most often in emergency situations, coronary angiography of the heart and stenting are performed in the course of one manipulation. Then anticoagulants are administered intravenously before the operation.
Technique coronary stenting
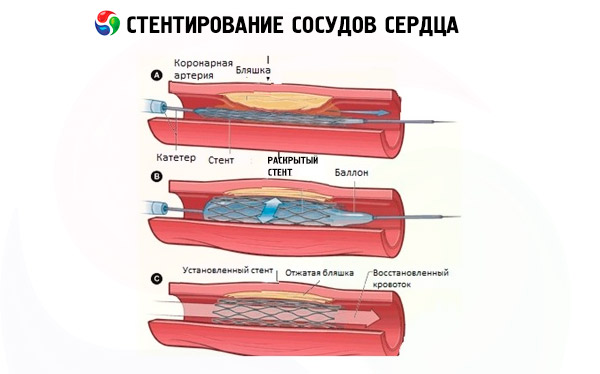
Coronary balloon angioplasty and stenting of heart vessels are percutaneous (percutaneous) coronary interventions for vessel dilation using a balloon catheter, and the installation of a stent in the lumen of the vessel actually occurs after its expansion using balloon angioplasty.
Usually, the technique of performing stenting of the heart vessels - with the main stages of the process - is described in general terms as follows. After general sedation and local anesthesia of a small area of skin, the surgeon punctures it with a simultaneous puncture of the vessel wall. Stenting of the heart vessels can be performed through the arm - transradial access (puncture of the radial artery of the forearm), as well as through the femoral artery in the groin area (transfemoral access). The entire procedure is performed under fluoroscopic visualization by an angiograph with the introduction of a contrast agent into the blood.
A catheter is inserted into the arterial bed through a puncture in the vessel – to the mouth of the coronary vessel in which stenosis has been detected. Then a guidewire is inserted, along which the catheter with the balloon and the stent attached to it is advanced; as soon as the balloon is exactly at the site of the narrowing, it is inflated, causing the vessel walls to expand. At the same time, the stent straightens out and, under the pressure of the balloon, fits tightly to the endothelium, pressing into the vascular walls and forming a strong frame, which becomes an obstacle to the narrowing of the lumen.
After all auxiliary devices have been removed, the puncture site is treated with antiseptics and covered with a pressure bandage. The entire process of coronary stenting of the heart vessels can last from one and a half to three hours.
Contraindications to the procedure
Coronary stenting of heart vessels is contraindicated in the following cases:
- acute cerebrovascular accident (stroke);
- diffuse cardiosclerosis;
- congestive (decompensated) heart failure of various etiologies (coronary insufficiency of metabolic origin);
- the presence of acute infectious diseases, including bacterial endocarditis;
- severe functional failure of the liver, kidneys or lungs;
In cases of local internal bleeding and in patients with blood clotting disorders, stent installation is also contraindicated.
Myocardial revascularization using stenting is not performed:
- if the patient is intolerant to iodine and drugs containing it cause allergies;
- when the lumen of the coronary arteries is narrowed by less than half, and the degree of hemodynamic disturbances is insignificant;
- in the presence of extensive diffuse stenosis in one vessel;
- if small diameter vessels of the heart are narrowed (usually these are intermediate arteries or distal branches of the coronary arteries).
There are risks of stenting of cardiac vessels that are associated with damage to the vascular wall, infection, improper stent implantation, development of a heart attack and cardiac arrest.
Experts emphasize the risk of developing an allergic or anaphylactoid reaction (even to the point of shock) to iodine-containing radiocontrast agents injected into the blood during stenting. This increases the level of sodium and glucose in the blood, causing its hyperosmolarity and thickening, which can provoke vascular thrombosis. In addition, these substances have a toxic effect on the kidneys.
All these factors are taken into account by cardiologists when a patient with coronary circulation disorders is offered stent placement. However, it is necessary to consult with specialists in the field of vascular surgery. Where can I get advice on cardiac stenting? In regional clinical hospitals, many of which (for example, in Kyiv, Dnipro, Lviv, Kharkov, Zaporozhye, Odessa, Cherkassy) have cardiac surgery centers or endovascular surgery departments; in specialized medical centers for vascular and cardiac surgery, the largest of which are the Heart Institute of the Ministry of Health of Ukraine and the National Institute of Cardiovascular Surgery named after N. Amosov.
Consequences after the procedure
Possible complications after the procedure include:
- formation of a hematoma in the area of vessel puncture;
- bleeding after removing the catheter from the artery - in the first 12-15 hours after stent placement (according to some data, observed in 0.2-6% of patients);
- temporary, within the first 48 hours, disturbance of heart rhythm (in more than 80% of cases);
- dissection of the intima (inner lining) of the vessel;
- severe renal failure.
Fatal consequences after the procedure are associated with the development of myocardial infarction (statistics vary in different sources from 0.1 to 3.7% of cases).
One of the key complications of stenting is restenosis, that is, repeated narrowing of the lumen several months after coronary intervention; it is observed in 18-25% of cases, and according to experts from the American Society for Cardiovascular Angiography and Interventions, in more than a third of patients.
This is due to the fact that after the stent is installed - due to its pressure on the vascular wall and the development of an inflammatory reaction - blood platelets can settle and accumulate on the inner surface of the structure, causing the formation of a thrombus - stent thrombosis, and hyperplasia of endothelial cells leads to intimal fibrosis.
As a result, patients experience shortness of breath after stenting of the heart vessels, a feeling of pressure and squeezing behind the sternum. According to clinical statistics, approximately 26% of patients experience tingling and pain in the heart after stenting, which indicates recurrent angina. In such situations, given the high risk of myocardial ischemia, which easily transforms into a heart attack, repeated stenting of the heart vessels or bypass surgery is recommended. What is best for a particular patient is decided by cardiologists after an ultrasound or CT scan of the heart.
What is the difference between bypass surgery and cardiac stenting? Unlike stenting, coronary artery bypass grafting is a full-fledged cardiac surgery under general anesthesia with thoracic access (opening the chest). During the operation, a part of another vessel (extracted from the internal mammary artery or femoral saphenous vein) is taken and an anamostosis is formed from it, bypassing the narrowed section of the coronary vessel.
To avoid thrombus formation and restenosis, stents with various antithrombotic passive coatings (heparin, nanocarbon, silicon carbide, phosphorylcholine) have been developed, as well as eluting stents (drug-eluting stents) with an active coating containing slowly washed-out drugs (groups of immunosuppressants or cytostatics). Clinical studies have shown that the risk of re-stenosis after implantation of such structures is significantly reduced (up to 4.5-7.5%).
To prevent vascular thrombosis, all patients are required to take medications for a long time after stenting of the heart vessels:
- Aspirin (acetylsalicylic acid);
- Clopidogrel, other trade names - Plagril, Lopirel, Thrombonet, Zilt or Plavix after stenting of cardiac vessels;
- Ticagrelor (Brilinta).
Postoperative period
In the early postoperative period, which includes a hospital stay of two to three days (in some medical institutions, a little longer), patients should remain in bed for 10 to 12 hours after stenting of the heart vessels.
By the end of the first day, if the patients feel normal after stenting of the heart vessels, they can walk, but the first two weeks physical activity should be as limited as possible. A sick leave certificate is mandatory after stenting of the heart vessels.
Patients are warned that after stenting of the heart vessels they cannot take a hot shower or bath, lift heavy objects, and smoking is strictly prohibited after stenting of the heart vessels.
It should be borne in mind that the temperature after stenting of the heart vessels may increase slightly due to heparin administered half an hour before the start of the operation (it is used to minimize the risk of blood clots). But a feverish state may also be associated with infection during the insertion of a catheter.
High blood pressure is observed after stenting of coronary vessels, especially in patients with arterial hypertension: after all, installing a stent in a coronary vessel does not solve problems with blood pressure and atherosclerosis. Fluctuations in blood pressure after stenting are also explained by vagal vascular reactions mediated by thyroxine: iodine-containing radiocontrast agents increase the level of this thyroid hormone in the blood, and acetylsalicylic acid (Aspirin) prescribed in large doses reduces it.
Transient decrease in vascular tone and low blood pressure after stenting of cardiac vessels can also be one of the side effects of contrast agents containing iodine. In addition, a negative factor is the impact on the body of X-ray radiation, the average dose of which during the installation of coronary stents ranges from 2 to 15 mSv.
What should not be done after stenting of cardiac vessels?
After stenting of the heart vessels, it is important to follow certain precautions and recommendations from doctors to ensure normal recovery and prevent complications. Here are some important things that are not recommended to do after this procedure:
- Physical activity: Your doctor may recommend limiting your physical activity for the first few days or weeks after stenting. This may include heavy lifting, vigorous exercise, and other types of physical activity. Patients are usually allowed to gradually increase their physical activity after consulting with their doctor.
- Smoking: Smoking is one of the major risk factors for heart disease and should be stopped immediately after stenting. Smoking can increase the risk of blood clots in the stent and other complications.
- Nutrition: After stenting, it is important to maintain a healthy diet and control your cholesterol and blood sugar levels. Your doctor may recommend a diet that limits fats and carbohydrates.
- Medication: Patients are often prescribed medications after stenting, such as anticoagulants, antiplatelet agents, beta blockers, and others. It is important to strictly follow your doctor’s instructions for taking medications and not stop taking them without your doctor’s consent.
- Avoiding stress: Stress can negatively affect the health of the heart. Patients are advised to avoid stressful situations and, if necessary, to consult a stress management specialist.
- Regular medical follow-up: After stenting, it is important to follow your doctor's recommendations and visit him for regular follow-up appointments.
In addition to the above precautions, the following recommendations should also be taken into account after cardiac stenting:
- Caring for the Stent Insertion Site: If the stent was inserted through an artery in your wrist or thigh, it is important to take care of the site. Your doctor may recommend keeping the area clean and dry and avoiding straining or lifting on that side.
- Diet: Diet after stenting should be rich in fruits, vegetables, magnesium, potassium and low in sodium. This helps maintain healthy cardiovascular health.
- Cholesterol levels: If your blood cholesterol levels are high, your doctor may recommend taking medications to lower them and monitoring your diet.
- Blood Pressure Monitoring: Blood pressure levels should also be measured regularly and maintained at optimal levels.
- Weight loss: If the patient is overweight or obese, weight control and dietary advice may be important measures.
- Avoiding Alcohol: Your doctor may recommend that you limit your alcohol intake or avoid it altogether.
- Seek early medical attention: If you experience any new or worsening symptoms such as chest pain, shortness of breath, malaise, or abnormal heart rhythms, seek immediate medical attention.
Remember that recommendations may vary for each patient, and it is important to follow your doctor's individual instructions. If you experience any unusual symptoms, such as chest pain, shortness of breath, dizziness, or weakness, seek immediate medical attention.
Rehabilitation and recovery
How long cardiac rehabilitation and recovery takes after the placement of an intravascular stent depends on many factors.
First of all, you should conscientiously follow all medical recommendations after stenting of the heart vessels.
In particular, moderate physical activity and gymnastics after cardiac stenting should become an integral part of the lifestyle. Experts say that aerobic exercises are best - in the form of regular walks or bike rides, which do not require much effort, but strain most muscles and promote blood circulation. You just need to monitor your pulse and avoid tachycardia.
Those who like to take a steam bath will have to make do with a shower in their bathroom. Ordinary motorists should refrain from driving for two to three months. And if the stent was implanted during an exacerbation of coronary syndrome, a threat of a heart attack or during one, it is unlikely that stress-related work as a driver will be possible after stenting of the heart vessels. It is in such cases that disability may be established after cardiac stenting.
Is a diet necessary after cardiac stenting? Yes, since it is impossible to allow the level of cholesterol in the blood to increase, and lifelong restrictions in the diet should concern the total caloric content (towards its reduction in order to avoid obesity), as well as the consumption of animal fats, table salt and fermented foods. For more information on what you can eat after cardiac stenting, read the publication - Diet for high cholesterol and the article - Diet for atherosclerosis
The ban on smoking was mentioned above, but alcohol after stenting of the heart vessels - only high-quality red wine (dry), and only one glass - is occasionally allowed.
In the first four to five months after cardiac stenting, cardiologists equate sex to intense physical activity, so this must be taken into account so as not to overdo it and cause a heart attack.
In case of a severe attack, when nitroglycerin does not relieve chest pain, how to behave after stenting of the heart vessels? Call an ambulance, preferably a cardiology one!
In addition, daily Clopidogrel (Plavix) reduces platelet aggregation, meaning that any accidental bleeding will be difficult to stop, and this should be taken into account by all patients. Other side effects of this drug include: increased bleeding and bleeding (nose, stomach); cerebral hemorrhage; digestive problems; headaches, joint and muscle pain.
Overall, despite this, heart pain stops in seven out of ten cases, and patients with a coronary stent feel much better.
Lifestyle after cardiac stenting
As experts in the field of endovascular surgery claim, and as evidenced by patient reviews of coronary stenting, life after cardiac stenting changes for the better.
When doctors are asked how long people live after cardiac stenting, they avoid giving a direct answer: even with a perfectly performed endovascular intervention, there are many factors (including immune factors) that, one way or another, affect the state of general and coronary circulation.
But if you lead a healthy lifestyle after cardiac stenting, it will last longer and give you the opportunity to live up to fifteen years.


 [
[