Medical expert of the article
New publications
Sialadenitis: causes, symptoms, treatment
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
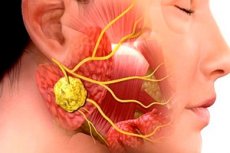
Inflammatory pathologies in surgical dentistry are very common. Even the use of antibiotic therapy does not reduce the incidence of maxillofacial inflammations and their complications. This situation is due to late visits to doctors, frequent self-medication of patients, etc. One of the typical infectious and inflammatory diseases of this kind is sialadenitis, or sialoadenitis - inflammation of the salivary gland, often provoked by viruses or bacteria. The pathology is accompanied by a number of characteristic clinical signs, and the diagnosis is established based on the results of bacteriological and cytological studies, as well as instrumental diagnostics.
Epidemiology
The exact prevalence of submandibular sialadenitis is unclear. Submandibular sialadenitis accounts for about 10% of all cases of sialadenitis. It accounts for 0.001 to 0.002% of all hospitalizations. There are no age or sex differences.[ 1 ]
Bacterial and viral sialadenitis mainly affects elderly and senile people.
Epidemic mumps affects mainly children, less often adults (women - more often). Today, epidemic mumps occurs as a sporadic disease, which is due to early vaccination of children.
A purulent form of sialadenitis is often recorded, which is due to the late seeking of medical help by patients.
Causes sialadenitis
The development of sialadenitis is caused by viral or microbial lesions of the salivary glands. The microbial inflammatory process can be provoked by bacteria present in the oral cavity or released from various infectious foci in the body. Sources of infection are often adjacent phlegmon, acute respiratory diseases (tonsillitis, pneumonia, bronchitis), maxillofacial and dental pathologies.
The disease may appear as a result of injuries and surgeries in the maxillofacial area, the entry of foreign bodies into the salivary canal (fish bones, food particles, hairs, etc.), and canal stone formation.
Viral sialadenitis is most often caused by cytomegaloviruses, influenza viruses, adenoviruses, paramyxoviruses, Coxsackie viruses, herpes simplex viruses, etc. Fungal sialadenitis, syphilitic, and tuberculous also occur.
The spread of infection can occur through the canal opening, through blood or lymphatic fluid.
Risk factors
Risk factors for the development of sialadenitis include:
- weakened immune system, recent illnesses;
- congestion in the salivary ducts;
- salivary disorders caused by infectious and inflammatory pathologies;
- surgical operations;
- tuberculosis; [ 2 ]
- syphilis;
- maxillofacial injuries.
The risk group includes the elderly, people suffering from eating disorders, pathological dry mouth, as well as those undergoing radiation therapy, or regularly using antibiotic therapy without good indications, postoperative conditions, [ 3 ] intubation, and the use of anticholinergics. [ 4 ]
Additional (indirect) predisposing factors may include:
- poor oral hygiene;
- unhealthy lifestyle, presence of a number of bad habits;
- ignoring visits to doctors, self-medication.
Pathogenesis
The salivary glands are divided into paired large and unpaired small. Large glands include the parotid, submandibular, and sublingual. Small glands include the labial, buccal, lingual, palatine, and oral floor glands. Each of these glands has parenchyma, interstitium, and a duct system.
The causative agent of epidemic parotitis, one of the variants of acute sialadenitis, is a filterable virus. A person becomes infected by direct transmission from a sick person, the transmission route is airborne (but infection through objects used by the sick person is not excluded).
Bacterial sialadenitis can develop with any severe pathologies. The infection spreads through the stomatogenic route, as well as through the blood and lymphatic fluid. The microflora is usually of a mixed type: streptococcal, pneumococcal, staphylococcal, etc., which enters through the excretory glandular duct.
In patients with lymphogenous divergence of infection, the lymphoid network of the parotid gland is often affected: this process is a consequence of nasopharyngeal or mandibular inflammation, pathologies of the teeth or tongue.
The etiology and pathogenesis of chronic sialadenitis are unclear and poorly understood. Doctors assume that the development of the disease is associated with general pathologies in the body - in particular, with hypertension, atherosclerosis, deforming spondylosis, and diseases of the digestive tract.
Symptoms sialadenitis
Acute sialadenitis can proceed with different intensity. In mild cases, the clinical picture is poorly expressed, without an increase in body temperature and without pain in the parotid glands, which only swell slightly. In moderate cases, there is general malaise, pain in the head and muscles, chills, dry mouth mucous membranes, pain and swelling of the parotid gland. Salivation is slightly reduced. Symptoms last for about 4 days, after which gradual relief occurs. In severe cases of acute sialadenitis, the parotid gland greatly enlarges, the submandibular and sublingual glands may be involved in the process. Salivation increases, the temperature reaches high values (up to 40 ° C), and purulent-necrotic complications may develop. Under favorable circumstances, the temperature begins to decrease after about a week, and signs of an inflammatory reaction gradually subside. However, the risk of abscess formation remains, as does the risk of developing meningitis, encephalitis, paralysis of the cranial and spinal nerves, etc.
Viral sialadenitis of the parotid glands manifests itself as pain when opening the mouth and when trying to turn the head to the side. Swelling of the buccal, mandibular, submandibular zone and upper part of the neck is noted. Palpation reveals a painful compaction with a smooth surface, not extending beyond the boundaries of the parotid gland. The spread of pathology to surrounding tissues occurs with the development of a purulent process.
When the submandibular gland is affected, patients complain of pain when swallowing. The swelling extends to the sublingual and submandibular area, chin and upper neck. When the sublingual glands are affected, pain appears when moving the tongue, and the sublingual folds increase. Involvement of minor salivary glands occurs with multiple pathologies.
The first signs of chronic sialadenitis may go unnoticed and are detected by chance. Patients notice discomfort in the parotid gland (or two glands), less often - occipital pain. Visually, a soft swelling is determined in the affected area, without obvious pain. There are no changes in the skin, the oral cavity opens painlessly, the mucous tissues are without pathologies, salivation is not impaired (it may decrease during a relapse). At an advanced stage of chronic sialadenitis, patients experience general weakness, fatigue, hearing loss, and sometimes dryness of the mucous membranes of the oral cavity. Swelling in the area of the affected glands is constant, without pain.
Interstitial sialadenitis is characterized by seasonal exacerbations (in the cold season), during which painful seals form and body temperature rises.
Sialadenitis in children
Sialadenitis can develop in childhood, even in newborn babies. However, the etiology of the disease in infants has not yet been determined. It is known that inflammation of the mammary gland in the mother contributes to the development of the disease. Sialadenitis in newborns is differentiated from osteomyelitis of the condylar process of the mandible, indicating the development of septicopyemia.
In general, the main causes of sialadenitis in children are considered to be epidemic parotitis and cytomegalovirus. In addition, it is important to know about the possible development of Herzenberg's false parotitis, which does not refer to sialadenitis and is an inflammation of the lymph nodes localized near the parotid salivary gland. The clinical picture of the diseases is very similar.
Tuberculous and syphilitic etiology of the disease is not typical for children. The clinical picture is characterized by more serious intoxication than in adults, as well as a higher percentage of development of purulent or purulent-necrotic tissue melting.
Stages
Sialadenitis develops through three corresponding stages: initial, clinically expressed and late.
The initial stage is not accompanied by pronounced clinical symptoms. However, swelling increases, lymphatic congestion is observed in the affected area, connective tissue loosens, and blood vessels dilate. Terminal glandular segments are preserved, but mucin and mucopolysaccharides, inflammatory markers, accumulate in them. Interlobar ducts become wider, collagen fibers become denser.
The second stage is characterized by the following picture:
- atrophy of the terminal glandular segments occurs;
- infiltrates are formed based on plasma structures, lymphocytes and histiocytes in the connective tissue base;
- the mouths are surrounded by fibrous tissue;
- inside the canals, there is an accumulation of desquamated epithelium and lymphocytes.
The third stage is accompanied by almost complete atrophy of the glandular parenchyma, its replacement by connective tissue, proliferation of the blood supply network, expansion of the intralobar ducts (or narrowing caused by compression by connective tissue and fibrous structures).
Forms
The classification of the disease is quite extensive. Thus, according to the course of the inflammatory reaction, acute and chronic sialadenitis are distinguished.
Acute sialadenitis of the parotid gland occurs as an epidemic parotitis, or the well-known "mumps". In general, the parotid glands are most often affected, less often - the submandibular and sublingual salivary glands. The acute process is easier to treat than the chronic one.
Depending on the condition of the parenchyma, the following types of chronic disease are distinguished:
- chronic parenchymatous sialadenitis - accompanied by damage to only the glandular stroma (as in patients with mumps);
- chronic interstitial sialadenitis – in addition to the stroma, is accompanied by damage to the glandular parenchyma (as in patients with cytomegalovirus sialadenitis).
- Chronic sclerosing sialadenitis (Küttner's tumor) is an IgG4-associated sclerosing disease and has distinct histopathological features such as dense lymphoplasmacytic infiltrate, sclerosis, and obliterative phlebitis.[ 5 ]
Interstitial sialadenitis is also called chronic productive sialadenitis, chronic sclerosing mumps, Kuttner's inflammatory tumor, chronic atrophic sialadenitis, fibroproductive sialadenitis, symptomatic sialopathy, hormonal sialosis. The etiology of the disease is poorly understood.
Influenza sialadenitis develops during flu epidemics, which are observed mainly in winter. Patients show signs of acute sialadenitis of one or more salivary glands. The parotid gland is most often affected, the inflammation increases quickly and spreads to the paired gland.
Depending on the location of the lesion, a distinction is made between:
- mumps sialadenitis of the parotid glands;
- submaxillitis - a lesion of the submandibular gland;
- sublingual sialadenitis of the sublingual gland.
According to the inflammatory characteristics, sialadenitis of the salivary gland can be:
- serous;
- hemorrhagic;
- purulent;
- connective tissue;
- granulomatous;
- fibroplastic;
- destructive;
- undeformed;
- cirrhotic.
Depending on the etiology, the following are distinguished:
- traumatic inflammatory process;
- toxic;
- autoimmune;
- allergic;
- obstructive (with blockage or cicatricial contraction).
Calculous sialadenitis is a type of obstructive pathology caused by blockage of the duct by a salivary gland stone.
If the inflammatory disease progresses, then purulent-necrotic or gangrenous sialadenitis develops. In this case, a picture of severe phlegmon with pronounced edema, infiltration, hyperemia, fluctuation, etc. is noted.
Ductal sialadenitis (or sialodochit) is a consequence of congenital defects of the salivary glands (strictures and ectasias) in combination with weak immunity and hyposalivation, stagnation of saliva inside the ducts.
Complications and consequences
Acute sialadenitis may be complicated by damage to the oculomotor, optic, abducens, facial, vestibulocochlear nerves, as well as mastitis, pancreatitis, nephritis. Orchitis often develops in boys and men.
If acute sialadenitis occurs against the background of general pathologies, it may be complicated by the divergence of the pathological process into the peripharyngeal space, into the tissues surrounding the carotid artery and the internal jugular vein. In some patients, purulent contents break through into the external auditory canal. Rarely, damage to the walls of large vessels is observed, which entails bleeding. Venous thrombosis and blockage of the sinuses of the meninges are also possible.
A late complication of advanced purulent sialadenitis is the formation of fistulas and parotid hyperhidrosis.
If bacterial sialadenitis is left untreated, massive swelling of the neck tissue may develop, which can lead to respiratory obstruction, septicemia, cranial osteomyelitis, and trigeminal neuritis.
Diagnostics sialadenitis
General clinical diagnostic methods include questioning the patient, examining him, and palpating him. Additionally, laboratory testing of blood and urine is prescribed. If we are talking about a child, then it is necessary to check with the parents whether he has previously suffered from mumps, whether he has had contact with sick people.
If chronic sialadenitis is suspected, the annual frequency of relapses, the size of the gland at different periods of the inflammatory process are specified. Attention is paid to the condition of the skin over the affected area, the volume and nature of the salivary fluid, the condition of the excretory salivary ducts.
The following is mandatory:
- assessment of secretory function;
- cytology, microbiology, immunology of salivary secretions;
- contrast sialography;
- computed tomography;
- radiosialography;
- ultrasound;
- puncture biopsy.
Many pediatric patients are indicated for electroencephalography, which is necessary to assess disorders of brain bioactivity.
Mandatory instrumental diagnostics include sialometry, which involves using a polyethylene catheter, which after preliminary bougienage is inserted into the salivary duct. The manipulation is performed on an empty stomach, and the procedure itself lasts about 20 minutes. It provides information on the volume of salivary production and the physical characteristics of the secretion. [ 6 ]
Contrast sialography is performed at the stage of remission of the disease, as it can provoke a relapse. Radiocontrast solutions are introduced into the salivary gland using a syringe and a polyethylene catheter.
Special instrumental diagnostics are represented by the following procedures:
- cytology of salivary secretion smears;
- Electroradiography with contrast;
- salivary gland scanning method;
- puncture with biopsy and subsequent histology.
Ultrasound is most often performed in the form of sialosonography - a study that allows you to examine the full picture of the glandular structure. The doctor has the ability to detect sclerotic tissue disorders, blockages, tumor processes, stones, determine their number and size.
In bacterial sialadenitis, non-specific changes are detected during ultrasound. At an early stage of development, an increase in echogenicity and expansion of the duct are noted, and the presence of anechoic foci indicates possible abscess formation. [ 7 ]
Magnetic resonance imaging and computed tomography allow us to exclude the presence of stones in the ducts and to clarify the depth of the pathological process.
Laboratory tests include a general blood and urine test, as well as salivary fluid. The blood may show a high level of leukocytes, which is one of the signs of an inflammatory process. In a biochemical blood test, sugar levels are important, and in a urine test, the salt composition. Leukocytes, pus, and bacterial flora can often be detected in salivary secretion. It is also necessary to examine the physicochemical characteristics of the secretion.
Differential diagnosis
First of all, it is important to determine the root cause of the pathological condition, to find out whether the disease is of atherogenic, infectious, neoplastic, autoimmune, metabolic nature. Rheumatological and autoimmune pathology should be excluded.
Interstitial sialadenitis is differentiated from chronic parenchymatous sialadenitis, sialodochit, tumor processes, epidemic parotitis. For diagnostics, an assessment of typical symptoms, cytological and sialographic picture in accordance with the diseases is used.
In general, sialadenitis should be distinguished from salivary stone disease, salivary gland cysts, and tumor processes. Diagnosis is based on clinical symptoms, sialometry data, cytological examination of salivary secretions, radiography and sialography, puncture and excisional biopsy.
It is important for patients to understand that sialadenitis or sialoadenitis are two equivalent concepts that are completely interchangeable.
In some cases, the clinical features of the disease and laboratory parameters may require a broader diagnostic search: in such a situation, a salivary gland biopsy is recommended to establish an accurate diagnosis.
Who to contact?
Treatment sialadenitis
A patient with acute sialadenitis is prescribed treatment aimed at inhibiting the inflammatory reaction and normalizing salivation. Bed rest is prescribed for the duration of the fever. Warming compresses and ointment dressings are applied to the areas of compaction as indicated, and physiotherapy procedures are performed (light therapy, heat therapy - Sollux lamp, UHF, UV irradiation). High-quality oral care is provided, using rinses and irrigations.
In viral sialadenitis, irrigation with interferon 5 times a day (in case of early practice - on the 1-2 day) has a good effect. If the salivary function decreases, then 0.5 ml of antibiotic solutions of 50,000-100,000 ED penicillin and streptomycin with 1 ml of 0.5% novocaine are administered intraductally. In addition, a blockade with novocaine and penicillin or streptomycin is performed. If purulent inflammation progresses, foci of tissue melting are detected, then surgery is prescribed.
Pilocarpine for sialadenitis is taken orally, up to four times a day, 6 drops of a 1% solution. Such treatment is appropriate for serous inflammation. A good effect is noted when applying compresses with dimethyl sulfoxide, dimexide, which provides an analgesic, anti-inflammatory, anti-edematous and bactericidal effect. The compress is placed on the inflammation zone for about half an hour a day. The course of treatment consists of ten procedures, or until relief occurs.
In case of gangrenous sialadenitis and severe course of the disease, surgical treatment is prescribed, which consists of opening the glandular capsule: intervention on the parotid gland is carried out using the Kovtunovich technique.
In chronic sialadenitis, treatment is aimed primarily at increasing immunity, optimizing salivary function, preventing relapse, improving tissue trophism, eliminating congestion, and inhibiting sclerotic and degenerative processes.
The following medications are included in complex therapy:
- sodium nucleinate 0.2 g three times a day for two weeks (for chronic sialadenitis, such courses should be carried out up to three times a year);
- potassium iodide 10%, 1 tbsp. three times a day for 8-12 weeks (the patient’s body’s iodine sensitivity should be taken into account).
During treatment with sodium nucleinate, minor side effects may occur in the form of epigastric pain and dyspepsia. Such phenomena completely disappear upon completion of the drug intake.
Potassium iodide is contraindicated in case of hypersensitivity to iodine, pregnancy, pyoderma.
A novocaine blockade is performed once every 3 days, in a course of 10 blockades. Intramuscular injections of Pyrogenal are given (a course of 25 injections, once every three days), subcutaneous injections of 0.5% Galantamine (a course of 30 injections of 1 ml).
Patients with duct stenosis are prescribed proteolytic enzyme preparations (Chymotrypsin, Trypsin), as well as injection of Ribonuclease at 10 mg intramuscularly in combination with electrophoresis of deoxyribonuclease (up to 10 procedures for 20 minutes).
Galvanization for chronic sialadenitis is indicated in the form of daily procedures for 4 weeks, in combination with radiotherapy.
Surgical treatment is practiced infrequently, only in the case of lack of effect from drug therapy, as well as in case of regular relapses of the inflammatory disease (more than ten times a year), accompanied by a purulent process, pronounced functional disorders, strictures and atresia. According to indications, the method of flow bougienage, total plastic surgery of the mouth, glandular resection with preservation of branches of the facial nerve, blocking of the parotid canal are used.
Antibiotics
Antibiotic therapy is appropriate for bacterial sialadenitis and depends on the severity of the infectious process. [ 8 ]
The drugs of choice are often protected penicillin antibiotics and cephalosporins that inhibit the activity of β-lactamases:
Amoxiclav |
The drug amoxicillin and clavulanic acid is prescribed to adults orally in a daily dosage of 1500 mg (divided into two doses). Side effects in the form of nausea or diarrhea are mild and pass quickly. To prevent these reactions, the drug is recommended to be taken with food. |
Sulbactomax |
A preparation of sulbactam and ceftriaxone for intramuscular injections. Daily dosage is 1-2 g, administered every 24 hours. The duration of therapy is determined by the doctor. Possible side effects are more typical for long-term use. This includes candidiasis, mycosis, secondary fungal infections, enterocolitis, and dyspepsia. |
Piperacillin-Tazobactam |
A combined antibacterial drug that is administered to patients as intravenous infusions every 8 hours at 4.5 g. The daily dose can be changed by the doctor depending on the severity of the infection. Possible side effects: diarrhea, nausea, vomiting, skin rashes. |
If gram-negative microorganisms are detected, fluoroquinolone drugs are prescribed. In complex cases, combination therapy is used - for example, Carbapenem, Metronidazole and Vancomycin.
Physiotherapy treatment
At the initial stage of the inflammatory process with elevated body temperature, physiotherapy is not used. The patient is recommended to drink alkaline mineral waters (such as Borjomi) against the background of drug treatment. From about 3-4 days, it is possible to use UHF therapy in a non-thermal dose, electrophoresis of anti-inflammatory drugs.
Further, to treat acute sialadenitis, the doctor may prescribe:
- Ultraviolet irradiation of the affected area begins with two biodoses, then increases by 1 biodose, bringing it to 6 biodoses. The procedures are performed every two days.
- Fluctuation of the infiltrate zone is carried out in sessions of 8-10 minutes. The course of therapy includes 10 sessions.
- After eliminating the signs of acute inflammation, in order to accelerate the resorption of the infiltrate, the following is used:
- Infrared irradiation in 20-minute sessions, in a course of 10-12 sessions.
- Ultrasound therapy with an intensity of 0.05-0.2 W/cm², duration up to 5 minutes, course of 10 sessions.
- Electrophoresis of 3% potassium iodide, lasting 20 minutes, in a course of 10-12 sessions.
To relieve pain, it is recommended to undergo laser therapy lasting 2-3 minutes, in a course of 8 to 10 sessions.
Salivary gland massage for sialadenitis
Intraoral (intrabuccal) massage improves blood and lymph flow, stimulates bioactive points, and improves the function of the salivary gland. The procedure is carried out in several stages, including general warming up of soft tissues, work with the salivary glands and muscles, and impact on the exit points of the cranial nerves.
Massage movements such as stroking, point pressure, and myoextensive kneading are used. The procedure is performed with clean hands; sterile surgical gloves can be used.
The salivary glands are massaged with gentle movements, starting from the periphery to the area of the excretory ducts.
After the session, the patient should rinse the mouth with an antiseptic solution.
Massage is performed not only to improve trophism in the gland tissues, but also to assess the amount of saliva, its color, consistency, and taste characteristics.
Herbal treatment
Traditional methods of treatment are allowed to be used only at an early stage of sialadenitis development, or only for the prevention of this disease. To alleviate symptoms, doctors recommend drinking plenty of fluids during drug therapy, including infusions and decoctions of herbs that have anti-inflammatory activity.
- Mint tea stimulates the secretion of saliva, relieves pain, refreshes, and eliminates unpleasant taste in the mouth.
- Chamomile infusion has anti-inflammatory and decongestant effects.
- Raspberry leaf tea accelerates wound healing and has an anti-inflammatory effect.
For daily mouth rinses, you can use infusions of the following herbal mixtures:
- raspberry leaves, immortelle flowers, field horsetail;
- peppermint leaves, plantain shoots, elder flowers;
- chamomile flowers, eucalyptus and sage leaves.
Rinsing with pine water gives a good effect. To prepare the remedy, boil 0.5 liters of water, add 2 tablespoons (with a slide) of pine needles (spruce or pine), cover with a lid, leave until completely cool, filter. Use for rinsing 2-3 times a day, or after each meal.
You should not self-medicate if the disease manifests itself with severe pain, stone formation, or suppuration.
Surgical treatment
In some cases, medication alone will not be enough to eliminate sialadenitis. In such situations, surgical intervention may be required.
In case of obstruction of the salivary gland excretory duct, surgical intervention is necessary. Under local anesthesia, the doctor removes the cause of the blockage and performs antiseptic treatment. In the postoperative period, antibacterial and symptomatic therapy is prescribed, and if necessary, additional bougienage of the excretory duct is performed with its subsequent rinsing.
Chronic sialadenitis is characterized by frequent recurrence, which over time can lead to complete or partial sclerosis of the gland tissue and the formation of connective tissue structures. If this happens, the affected gland is removed.
In case of sialadenitis, it is preferable to perform endoscopic minimally invasive procedures. Today, surgeons have special elastic endoscopes, with which they can penetrate the smallest glandular channels. During endoscopy, the doctor can fully examine the duct, take biomaterial for examination, fragment and remove the cause of obstruction.
In case of sialolithiasis, removal of the salivary gland stone is necessary using interventional sialendoscopy or direct surgical removal. [ 9 ], [ 10 ]
Several types of minimally invasive treatments have been proposed for the treatment of salivary gland stones, including interventional sialendoscopy (iSGE), extracorporeal shock wave lithotripsy (ESWL) [ 11 ], and combined endoscopic surgical procedures. [ 12 ] The choice of the right treatment should include criteria such as the affected gland, the number and size of stones, the location, and the relationship to the duct. The least damaging method is always the preferred treatment method. [ 13 ]
Postoperative complications such as pain, scarring, and nerve damage are common. Patients who underwent surgery experienced disorders such as xerostomia (up to 31%), taste changes (16.3%), hematomas (up to 14%), facial nerve damage (8%), and lingual nerve damage (12%). [ 14 ], [ 15 ], [ 16 ], [ 17 ]
Prevention
Preventive measures to prevent the development of sialadenitis are not specific. The essence of prevention is a complete, high-quality and balanced diet, a healthy and active lifestyle, and the eradication of bad habits. Compliance with such simple but important rules reduces the likelihood of many pathologies.
The occurrence of sialadenitis can be directly related to other diseases of the oral cavity and ENT organs. Violation of the ratio of microflora in the mouth, the entry of pathogenic microorganisms with the blood or lymph flow can provoke the development of an inflammatory process. Almost any chronic infectious and inflammatory focus can be considered as a predisposition to the occurrence of sialadenitis. Moreover, any infectious diseases negatively affect the immune defense of the body as a whole. Therefore, to prevent many diseases, it is important to maintain immunity in every possible way, promptly treat all diseases (including chronic ones), exclude hypothermia and stress, and in the winter-spring period take additional multivitamin preparations recommended by the attending physician.
Other mandatory preventive measures:
- regular hygiene procedures, high-quality cleaning of the oral cavity and teeth;
- avoiding the consumption of coarse foods that can damage the oral mucosa;
- quitting smoking;
- strengthening the immune system;
- the correct selection of a toothbrush and oral care products.
If any problems do occur, such as dry mouth mucosa, swelling, pain in the salivary glands, you should see a doctor without delay. Timely medical care will help prevent the development of inflammation and prevent adverse effects.
Forecast
Acute sialadenitis ends in recovery in the overwhelming majority of patients. However, fatal cases have also been described: this can happen if a purulent-necrotic process develops in the gland, as well as if the pathology spreads to the nervous system.
The prognosis for chronic disease is relatively favorable. In this situation, the concept of "conditional" recovery is used: it is applied if the patient's remission period lasts more than three years.
Patients are observed for several years, prevention of exacerbations is carried out, which usually occur 1-2 times a year, more often in cold weather. As a result of correctly prescribed therapy, long-term remission may occur. In some cases, the formation of a salivary stone in the glandular canal is noted.
Provided that the immune system is in a normal state, oral hygiene is observed, concomitant pathologies are treated and existing infectious foci are eliminated, sialadenitis completely disappears within 14 days.

