Medical expert of the article
New publications
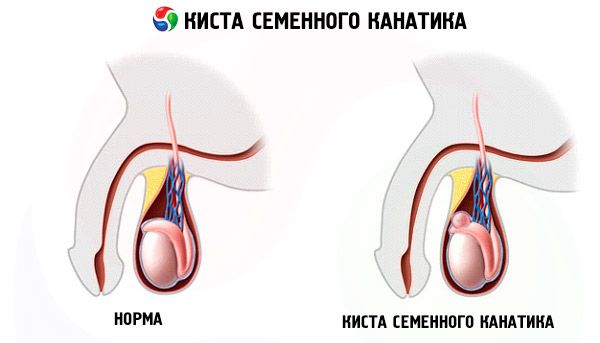
A cyst of the spermatic cord
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Causes spermatic cord cysts
There are the following reasons for the formation of cysts:
- Acquired - the cyst appears as a result of inflammation or damage to the organs of the scrotum. In this case, the inflamed or injured ducts stop working and close, as a result of which the outflow of produced spermatozoa is interrupted. Then the secretion begins to accumulate, thereby stretching the wall of the cord, forming a cyst where spermatozoa (new or destroyed old ones) accumulate;
- Congenital – the pathology develops due to a disturbance in embryonic development. It appears due to the fact that a special vaginal process located in the peritoneum (this is a section of the mucous membrane inside the peritoneum that performs the function of conducting the vas deferens with the testicles into the scrotum at the final stage of pregnancy) does not partially close. Because of this, non-communicating cavities appear along the path of the vas deferens with the epididymis. They are filled inside only with translucent fluid, and spermatozoa are not contained in them.
Risk factors
Symptoms spermatic cord cysts
A cyst of the vas deferens grows rather slowly and does not cause any disturbances in the reproductive function or sexual activity of a person. Mostly, patients complain about the appearance of an unknown additional neoplasm in the scrotum - it is easily palpated, but also does not hurt and does not manifest itself in any way.
Occasionally, if the cyst becomes too large or grows too quickly, the patient may experience symptoms such as severe discomfort while walking or sitting, as well as an unpleasant squeezing sensation inside the scrotum.
Spermatic cord cyst in a child
Sometimes a spermatic cord cyst disappears on its own in children under 1 year of age. Therefore, boys with this disease are observed by a urologist-andrologist or surgeon until 1-2 years of age. If necessary, surgery is performed on children from 1 year of age, approximately in the period of 1.5-2 years.
For children aged 2 years and over, surgery is prescribed soon after the problem is diagnosed. If the cyst is acute, which may result in strangulation of the inguinal hernia, treatment is performed according to urgent indications.
Where does it hurt?
Complications and consequences
A cyst generally does not pose a threat to health, but in any case, if it is present, you should consult a urologist, because it can be a sign of more serious pathologies.
For example, a cyst can be a precursor to a disease such as a tumor of the seminal ducts or testicle. It should be noted that the cyst itself cannot cause infertility, although if it grows too quickly, it can press on the surrounding tissues and healthy ducts, which can disrupt the reproductive function. Most often, this occurs in the case of bilateral development of the disease.
Complications can arise as a result of surgery, and not only those typical for such procedures (inflammation in the wound, bleeding, severe pain syndrome), but sometimes also specific ones.
An incorrectly performed operation can provoke a recurrence of the cyst or the development of a severe scarring process. Damage to the vas deferens or the vessels that feed the testicle can also cause infertility.
Diagnostics spermatic cord cysts
The cyst is first diagnosed by palpation - by detecting a dense elastic neoplasm of a round shape in the tail or head of the epididymis, as well as the spermatic cord. It feels like a third testicle.
 [ 27 ]
[ 27 ]
Tests
The following tests are required:
- Smear;
- Blood and urine for general analysis, as well as blood for bacteriological analysis;
- Analysis for hepatitis, HIV and other venereal diseases.
 [ 28 ], [ 29 ], [ 30 ], [ 31 ]
[ 28 ], [ 29 ], [ 30 ], [ 31 ]
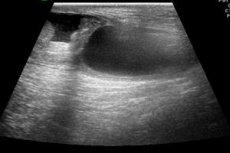
Instrumental diagnostics
To confirm the diagnosis, the following instrumental diagnostic procedures are used:
- Diaphanoscopy (transillumination is performed using transmitted rays). The procedure shows a small (often maximum 2-2.5 cm) cyst. It is transparent, contains light yellow liquid. Unlike other tissues, such a cyst is completely translucent;
- Examination of the scrotum using ultrasound. This method has almost completely replaced diaphanoscopy in our time, because it is considered a more accurate procedure that provides more information. This method identifies the exact location of the cyst, as well as the size of the formation. On ultrasound, it looks uniform, has clear and even contours both outside and inside. Although ultrasound does not make it possible to detect the presence or absence of sperm in such formations, this method is considered completely suitable for confirming the diagnosis;
- Occasionally, if cancer is suspected, an MRI or CT scan may be performed.
What do need to examine?
How to examine?
Who to contact?
Treatment spermatic cord cysts
This type of disease requires treatment only when it causes frequent and very noticeable pain, and the scrotum increases greatly in size, thereby interfering with sitting and any movements. Most urologists prefer to wait if the cyst is small. Surgery should be resorted to only if the cyst begins to clearly change the shape of the surrounding tissues.
Surgical treatment
The operation is performed under local anesthesia, and 1 day of hospitalization is enough to perform the procedure. After 10 days, the patient can fully return to normal life.
How the procedure is performed: a small incision is made through which the walls of the formation are carefully excised. At the same time, it is necessary to prevent severe trauma to the adnexal tissues in order to preserve reproductive function.
Next, the appendage is carefully sutured. Without this action, scars may appear in the postoperative period, which can disrupt the process of maturation and movement of the reproductive cells. To prevent this from happening, modern urologists use microsurgical instruments and also use optical magnification. This suture is usually so small that it does not leave a scar.
After the procedure, apply cold to the operated area for 2 hours.
Prevention
There is no specific prevention of cysts, as they can develop not only as a result of unfavorable external influences, but also be congenital. In order to protect yourself from the possible appearance of a cyst, a man should maintain a correct life rhythm, avoid prolonged stress, and have sex regularly.
Forecast
The spermatic cord cyst has a favorable prognosis. After the operation, the noticeable cosmetic defect disappears and the impaired reproductive function is restored. For 1 month after the procedure, you should refrain from physical activity. After this, you need to protect the scrotum from possible damage.

