Medical expert of the article
New publications
Reactive meningitis
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
By etiology, inflammation of the soft and arachnoid membranes of the brain (leptomeninges) – meningitis – can be bacterial, viral, parasitic or fungal. Or it can be non-infectious or reactive meningitis.
Epidemiology
According to statistics, non-infectious meningitis is observed in 1.4-2% of cases of systemic lupus erythematosus, in 10% of cases of sarcoidosis, and in 5-15% of cases of oncological blood diseases.
Causes reactive meningitis
The main causes of reactive meningitis are non-infectious autoimmune diseases, cancer, head injuries or brain surgery, the use of a number of pharmacological drugs and the administration of certain vaccines. [ 1 ], [ 2 ]
The risk factors for its development are similar.
Meningitis of this type can develop:
- in systemic lupus erythematosus (SLE); [ 3 ], [ 4 ]
- in Behcet's disease (systemic vasculitis); [ 5 ]
- in patients with idiopathic thrombocytopenic purpura;
- in cases of sarcoidosis, and can be diagnosed as neurosarcoidosis in the form of chronic meningitis; [ 6 ], [ 7 ]
- for melanoma, breast and gastrointestinal cancer, lung adenocarcinoma, T-cell lymphoma (non-Hodgkin's), acute lymphoblastic leukemia in children. [ 8 ]
The development of drug-induced aseptic meningitis can be caused by the use of non-steroidal anti-inflammatory drugs (NSAIDs); the fluoroquinolone antibiotic Ciprofloxacin, the anti-tuberculosis antibiotic Isoniazid and sulfonamides; the anticonvulsants Carbamazepine (Finlepsin) and Lamotrigine (Lamotrin); the immunosuppressant Azathioprine; drugs for the treatment of gastric ulcer (Ranitidine, Ranigast, Zantac, etc.) or gout (Allopurinol); some epidural anesthetics; antitumor drugs (Methotrexate, Pemetrexed, Cytarabine), as well as monoclonal antibodies (Infliximab, Adalimumab, Cetuximab). [ 9 ]
Pathogenesis
Patients with systemic lupus erythematosus are more prone to developing infections both due to immune problems and due to immunosuppressant therapy. At the same time, according to research results, in 50% of cases pathogenic bacteria are not detected in the cerebrospinal fluid (even in the presence of lymphocytic or neutrophilic pleocytosis) by microbiological methods, therefore meningitis is defined as aseptic.
Most often, in SLE, the pathogenesis of reactive meningitis without detection of infectious etiology is explained by non-inflammatory thickening of the endothelium of the vascular walls of the capillaries of the brain membrane in response to the action of autoantibodies circulating in the cerebrospinal fluid, which is defined as immune-mediated vasculopathy. In addition, it is assumed that the lupus anticoagulant (a prothrombotic antibody that binds to the phospholipids of the cell membranes of blood platelets) can cause occlusion of small vessels with the development of chronic tissue hypoxia.
Also, the mechanism of damage to the soft meninges in lupus is seen in the effect on the vascular plexus of antigen-antibody complexes penetrating the blood-brain barrier. And some experts believe that the whole thing is about non-steroidal anti-inflammatory drugs and immune-suppressing drugs taken for a long time for this autoimmune pathology.
In the presence of the previously mentioned oncological diseases, non-infectious meningitis is a consequence of the spread of cancer cells into the meninges, and it can be defined as neoplastic meningitis, meningeal or leptomeningeal carcinomatosis.
In cases of drug-induced reactive meningitis, the mechanism of alteration of the meninges may be associated with both reactions of increased autoimmune sensitivity to the active substances of pharmacological drugs and with their side effects.
Symptoms reactive meningitis
The first signs of reactive meningitis may include severe headaches and fever.
In general, its symptoms are typical of meningitis and include: stiffness of the neck muscles, nausea and vomiting, increased sensitivity of the eyes to light (photophobia) and changes in mental status in the form of confusion.
Reactive meningitis in a newborn may manifest itself only with non-specific symptoms (increased irritability or drowsiness).
In addition to headache, common manifestations of neoplastic meningitis may include hydrocephalus, swallowing problems, and cranial nerve palsy.
Drug-induced reactive meningitis usually shows neurological disturbances such as numbness, paresthesia, seizures.
Complications and consequences
This type of meningitis can lead to serious complications (such as deafness or hydrocephalus), as well as long-term consequences such as epilepsy or cognitive impairment.
Diagnostics reactive meningitis
Diagnosis of reactive or non-infectious meningitis is carried out comprehensively and is based on clinical symptoms, laboratory tests and hardware visualization.
Tests include cytological and general analysis of cerebrospinal fluid (CSF), as well as bacterial culture or PCR analysis of blood.
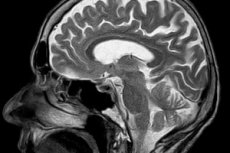
Instrumental diagnostics uses magnetic resonance imaging (MRI) of the brain.
Differential diagnosis
Differential diagnosis should exclude bacterial and other types of infectious meningitis, as well as meningism.
Treatment reactive meningitis
Treatment options may vary depending on the specific cause of meningitis.
In cases of non-infectious (reactive) meningitis, treatment is aimed at the underlying disease, meaning its options vary.
The use of drugs that cause an increased response with alteration of the meninges is discontinued.
Supportive therapy is also given to reduce the intensity of symptoms.
In addition, in severe cases of patients - before receiving the results of the cerebrospinal fluid analysis - antibacterial drugs and corticosteroids are urgently used as a preventive measure. They are cancelled if the cerebrospinal fluid is sterile, that is, after excluding infectious causes.
For patients with leptomeningeal carcinomatosis, a combination of radiation therapy and chemotherapy (with the introduction of an anticancer drug into the cerebrospinal fluid via lumbar puncture) is indicated.
Prevention
Currently, prevention of the development of reactive meningitis can only concern the prescription and use of drugs that may be involved in its occurrence, as well as monitoring the condition of patients in whose treatment such drugs are used.
Forecast
The prognosis for noninfectious meningitis depends on the underlying disease. For example, most patients with neoplastic reactive meningitis survive for one to one and a half months without treatment, dying of progressive neurological dysfunction; with treatment, survival is three to six months.

