Medical expert of the article
New publications
Idiopathic thrombotic thrombocytopenic purpura in adults
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
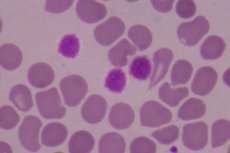
Idiopathic (immune) thrombocytopenic purpura is a hemorrhagic disorder caused by thrombocytopenia not associated with a systemic disease. It is usually chronic in adults but is often acute and transient in children. The spleen is normal in size. Diagnosis requires exclusion of other diseases by selective tests. Treatment includes glucocorticoids, splenectomy, and, for life-threatening bleeding, platelet transfusions and intravenous immunoglobulin.
Causes idiopathic thrombotic thrombocytopenic purpura.
Symptoms idiopathic thrombotic thrombocytopenic purpura.
Symptoms include petechiae and mucosal bleeding. The spleen is of normal size unless it enlarges due to a viral infection. Idiopathic thrombocytopenic purpura is suspected in patients with unexplained thrombocytopenia. Peripheral blood parameters are within normal limits, except for a decrease in the platelet count. Bone marrow examination is performed if, in addition to thrombocytopenia, abnormalities are detected in the peripheral blood smear or changes in the levels of other cellular elements. Bone marrow examination does not reveal any abnormalities or there is an increase in the number of megakaryocytes against the background of normal bone marrow. Since there are no specific diagnostic criteria, the diagnosis requires exclusion of other thrombocytopenic diseases based on clinical and laboratory data. Because HIV-associated thrombocytopenia may be indistinguishable from idiopathic thrombocytopenic purpura, HIV testing is performed in patients with risk factors for HIV infection.
What tests are needed?
Who to contact?
Treatment idiopathic thrombotic thrombocytopenic purpura.
Initial therapy is oral glucocorticoids (eg, prednisolone 1 mg/kg daily). In patients who respond to therapy, the platelet count rises to normal within 2 to 6 weeks. The glucocorticoid dose is then tapered. However, most patients do not respond adequately or relapse after glucocorticoid tapering is initiated. Splenectomy achieves remission in about two-thirds of such patients. Because patients refractory to glucocorticoids and splenectomy may not respond to further treatment and because the natural history of idiopathic thrombocytopenic purpura is often benign, additional therapy is not indicated unless the platelet count falls below 10,000/μL or active bleeding occurs; in this case, more intensive immunosuppressive therapy (cyclophosphamide, azathioprine, rituximab) is prescribed.
In children, only symptomatic treatment is usually used, since most children usually experience spontaneous recovery of thrombocytopenia within a few days or weeks. Even after months or years of thrombocytopenia, children may achieve spontaneous remission. If mucosal bleeding occurs, glucocorticoids or intravenous immunoglobulin are given. Data on the use of glucocorticoids or intravenous immunoglobulin in initial treatment are controversial, since they may increase platelet counts but may not improve clinical outcome. Splenectomy is rarely used in children. However, if thrombocytopenia is severe and symptoms persist for more than 6 months, splenectomy may be effective.
In children and adults with life-threatening bleeding, intravenous immunoglobulin 1 g/(kg x day) for 1 or 2 days is prescribed to quickly block phagocytosis. Typically, the platelet count rises on the second to fourth day, but only for 2-4 weeks. High doses of methylprednisolone (1 g/day intravenously for 3 days) are a cheaper and easier to use treatment method than using intravenous immunoglobulin, but this method is also effective. In patients with idiopathic thrombocytopenic purpura and the presence of life-threatening bleeding, platelet mass is used. However, platelet mass is not used for prophylactic purposes.
Oral glucocorticoids or intravenous immunoglobulin are used when a temporary increase in platelet levels is needed during dental extractions, childbirth, surgery, or other invasive procedures.
More information of the treatment


 [
[