Medical expert of the article
New publications
Neuropathy of the median nerve of the hand.
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
One of the most frequently diagnosed diseases of the peripheral nerves is neuropathy of the median nerve, one of the three main motor-sensory nerves of the hands, providing movement and sensation from the shoulder to the fingertips.
Without taking into account pathogenetic factors, many continue to call it neuritis, and ICD-10, based on the anatomical and topographic features of the disease, classifies it as a mononeuropathies of the upper extremities with the code G56.0-G56.1.
Epidemiology
The exact statistics of this pathology are unknown. Most epidemiological studies focus on carpal tunnel syndrome, which is the most common syndrome of peripheral compression of the median nerve with a disease frequency of 3.4% of all neuropathies: 5.8% in women and 0.6% in men.
European neurologists note that this syndrome is diagnosed in 14-26% of patients with diabetes; about 2% of cases are recorded during pregnancy, in almost 10% of professional drivers, in a quarter of painters, in 65% of people who constantly work with vibrating tools, and in 72% of workers engaged in manual processing of fish or poultry.
But pronator teres syndrome is found in almost two thirds of milkmaids.
Causes median nerve neuropathy
In most cases, the causes of median nerve neuropathy are compression of some part of the nerve trunk, which in neurology is defined as compression neuropathy of the median nerve, neurocompression or tunnel syndrome. Compression can be a consequence of injuries: fractures in the area of the humeral head or clavicle, dislocations and strong blows to the shoulder, forearm, elbow or wrist joints. If the blood vessels and capillaries of the endoneurium adjacent to the nerve are subject to compression, then compression-ischemic neuropathy of the median nerve is diagnosed.
In neurology, other types of medial nerve neuropathy are also distinguished, in particular, degenerative-dystrophic, associated with arthrosis, deforming osteoarthrosis or osteitis of the shoulder, elbow or wrist joints.
In the presence of chronic infectious inflammations of the joints of the upper extremities - arthritis, osteoarthritis of the wrist, rheumatoid or gouty arthritis, articular rheumatism - neuropathy of the median nerve can also occur. Here, as a trigger for pathology, we should also include inflammatory processes localized in the synovial bag of the joints, in the tendons and ligaments (with stenosing tendovaginitis or tenosynovitis).
In addition, damage to the median nerve can be caused by neoplasms of the bones of the shoulder and forearm (osteomas, bone exostoses or osteochondromas); tumors of the nerve trunk and/or its branches (in the form of neurinoma, schwannoma or neurofibroma), as well as anatomical anomalies.
Thus, if a person has a rare anatomical formation in the lower third of the humeral bone (approximately 5-7 cm above the middle epicondyle) - the spinous supracondylar process (apophysis), then together with the ligament of Struther and the humerus it can form an additional opening. It can be so narrow that the median nerve and brachial artery passing through it can be compressed, leading to compression-ischemic neuropathy of the median nerve, which in this case is called supracondylar apophysis syndrome or supracondylar process syndrome.
Risk factors
Experts consider the following to be absolute risk factors for the development of neuropathy of this nerve: constant tension of the wrist or elbow joints, prolonged actions with a bent or straightened wrist, which are typical for some professions. The importance of heredity and a history of diabetes mellitus, severe hypothyroidism - myxedema, amyloidosis, myeloma, vasculitis, and deficiency of B vitamins are also noted.
According to the results of some foreign studies, factors associated with this type of peripheral mononeuropathy include pregnancy, increased body mass index (obesity), and in men – varicose veins in the shoulder and forearm.
The risk of developing median nerve neuritis exists with antitumor chemotherapy, long-term use of sulfonamides, insulin, dimethylbiguanide (antidiabetic agent), drugs with glycolyl urea and barbituric acid derivatives, the thyroid hormone thyroxine, etc.
Pathogenesis
The long branch of the brachial plexus, which emerges from the brachial ganglion (plexus brachials) in the armpit, forms the median nerve (nervus medianus), which runs parallel to the humerus downwards: through the elbow joint along the ulna and radius of the forearm, through the carpal canal of the wrist joint into the hand and fingers.
Neuropathy develops in cases of compression of the middle trunk of the supraclavicular part of the brachial plexus, its external bundle (in the area where the upper nerve leg exits the brachial ganglion) or in the place where the internal nerve leg departs from the internal secondary bundle. And its pathogenesis consists in blocking the conduction of nerve impulses and disrupting the innervation of muscles, which leads to limited movement (paresis) of the radial flexor of the wrist (musculus flexor carpi radialis) and the round pronator (musculus pronator teres) in the forearm area - the muscle that provides turns and rotational movements. The stronger and longer the pressure on the median nerve, the more pronounced the nerve dysfunction.

The study of the pathophysiology of chronic compression neuropathies has shown not only segmental, but often extensive demyelination of the axons of the median nerve in the compression zone, pronounced edema of the surrounding tissues, an increase in the density of fibroblasts in the tissues of the protective sheaths of the nerve (perineurium, epineurium), vascular hypertrophy in the endoneurium and an increase in the volume of endoneurial fluid, which increases compression.
An increase in the expression of smooth muscle relaxant prostaglandin E2 (PgE2); vascular endothelial growth factor (VEGF) in synovial tissues; matrix metalloproteinase II (MMP II) in small arteries; and transforming growth factor (TGF-β) in fibroblasts of the synovial membranes of joint cavities and ligaments was also revealed.
Symptoms median nerve neuropathy
The main diagnostic definitions for compression mononeuropathies are: supracondylar apophysis syndrome, pronator teres syndrome, and carpal tunnel syndrome or carpal tunnel syndrome.
In the first case – with supracondylar apophysis syndrome (which was already discussed above) – compression of the median nerve manifests itself with symptoms of a motor and sensory nature: pain in the lower third of the shoulder (on the inside), numbness and tingling (paresthesia), decreased sensitivity (hypesthesia) and weakening of the muscles of the hand and fingers (paresis). The frequency of this syndrome is 0.7-2.5% (according to other data – 0.5-1%).
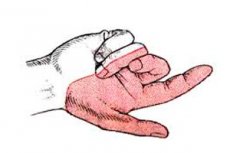
In the second case, symptoms of median nerve neuropathy appear after its compression when passing through the structures of the forearm muscles (pronator teres and flexor digitorum). The first signs of pronator teres syndrome include pain in the forearm (radiating to the shoulder) and hand; then there is hypoesthesia and paresthesia of the palm and the back of the terminal phalanges of the first, second, third and half of the fourth fingers; limited rotation and rotational movements (pronation) of the forearm and hand muscles, flexion of the hand and fingers. In advanced cases, the thenar muscle (elevation of the thumb) innervated by the median nerve partially atrophies.
In carpal tunnel syndrome, the trunk of the median nerve is compressed in a narrow bone-fibrous tunnel of the wrist (carpal canal), through which the nerve extends into the hand along with several tendons. This pathology is characterized by the same paresthesia (which does not go away even at night); pain (even intolerable - causalgic) in the forearm, hand, first three fingers and partly the index finger; decreased muscle motor skills of the hand and fingers.
The soft tissues in the area of the pinched nerve swell at the first stage, and the skin turns red and becomes hot to the touch. Then the skin of the hands and fingers turns pale or acquires a bluish tint, becomes dry, and the stratum corneum of the epithelium begins to peel off. Gradually, there is a loss of tactile sensitivity with the development of astereognosia.
In this case, the symptoms that manifest neuropathy of the right median nerve are identical to the signs that occur when the compression is localized on the left hand, that is, there is neuropathy of the left median nerve. For more details, see - Symptoms of damage to the median nerve and its branches
Complications and consequences
The most unpleasant consequences and complications of neuropathic syndromes of the medial nerve of the upper extremities are atrophy and paralysis of peripheral muscles due to disruption of their innervation.
In this case, motor limitations concern rotational movements of the hand and its flexion (including the little finger, ring and middle fingers) and clenching into a fist. Also, due to atrophy of the muscles of the thumb and little finger, the configuration of the hand changes, hindering fine motor skills.
Atrophic processes have a particularly negative effect on the condition of muscles if compression or inflammation of the nervus medianus has led to extensive demyelination of its axons - with the impossibility of restoring the conduction of nerve impulses. Then fibrous degeneration of muscle fibers begins, which becomes irreversible after 10-12 months.
Diagnostics median nerve neuropathy
Diagnosis of median nerve neuropathy begins with obtaining the patient's medical history, examining the limb and assessing the degree of nerve damage based on the presence of tendon reflexes, which are checked using special mechanical tests (flexion-extension of the joints of the hand and fingers).
To determine the cause of the disease, blood tests may be needed: general and biochemical, glucose levels, thyroid hormones, CRP content, autoantibodies (IgM, IgG, IgA), etc.
Instrumental diagnostics using electromyography (EMG) and electroneurography (ENG) make it possible to evaluate the electrical activity of the muscles of the shoulder, forearm and hand and the degree of conductivity of nerve impulses by the median nerve and its branches. Radiography and myelography with a contrast agent, ultrasound of vessels, ultrasound, CT or MRI of bones, joints and muscles of the upper limbs are also used.
Differential diagnosis
Differential diagnostics aims to distinguish median nerve mononeuropathy from ulnar or radial nerve neuropathy, brachial plexus lesion (plexitis), radicular dysfunctions in radiculopathy, scalenus syndrome, inflammation of the ligament (tenosynovitis) of the thumb, stenosing tendovaginitis of the flexor muscles of the fingers, polyneuritis in systemic lupus erythematosus, Raynaud's syndrome, sensitive Jacksonian epilepsy and other pathologies, the clinical picture of which has similar symptoms.
Who to contact?
Treatment median nerve neuropathy
Complex treatment of median nerve neuropathy should begin with minimizing compression and pain relief, for which the arm is given a physiological position and fixed with a splint or orthosis. Severe pain is relieved by perineural or paraneural novocaine blockade. While the limb is immobilized, the patient is given sick leave for median nerve neuropathy.
It should be borne in mind that treatment of the resulting neuropathy does not cancel the treatment of the diseases that caused it.
To reduce pain, medications in tablet form may be prescribed: Gabapentin (other trade names – Gabagama, Gabalept, Gabantin, Lamitril, Neurontin); Maxigan or Dexalgin (Dexallin), etc.
To relieve inflammation and swelling, paraneural injections of corticosteroids (hydrocortisone) are used.
Ipidacrine (Amiridin, Neuromidin) is used to stimulate the conduction of nerve impulses. It is taken orally at 10-20 mg twice a day (for a month); it is administered parenterally (subcutaneously or intramuscularly - 1 ml of 0.5-1.5% solution once a day). The drug is contraindicated in epilepsy, cardiac arrhythmia, bronchial asthma, exacerbation of gastric ulcer, pregnancy and breastfeeding; it is not used in children. Side effects include headache, allergic skin reactions, hyperhidrosis, nausea, increased heart rate, the occurrence of bronchial spasm and convulsions.
Pentoxifylline (Vazonit, Trental) improves blood circulation in small vessels and tissue blood supply. Standard dosage is 2-4 tablets up to three times a day. Possible side effects include dizziness, headache, nausea, diarrhea, increased heart rate, decreased blood pressure. Contraindications include bleeding and retinal hemorrhages, liver and/or kidney failure, gastrointestinal ulcers, pregnancy.
To increase the content of high-energy compounds (macroegs) in muscle tissues, alpha-lipoic acid preparations are used - Alpha-lipon (Espa-lipon): first, intravenous drip administration - 0.6-0.9 g per day, after two to three weeks, tablets are taken - 0.2 g three times a day. Side effects may include the appearance of urticaria, dizziness, increased sweating, pain in the abdominal cavity, and intestinal dysfunction.
For neuropathy associated with diabetes, Carbamazepine (Carbalex, Finlepsin) is prescribed. And all patients need to take vitamins C, B1, B6, B12.
Physiotherapeutic treatment of neuropathies is very effective, therefore, sessions of physiotherapy procedures are necessarily prescribed using ultraphonophoresis (with novocaine and GCS) and electrophoresis (with Dibazol or Proserin); UHF, pulsed alternating current (darsonvalization) and low-frequency magnetic field (magnetotherapy); conventional therapeutic massage and point (reflexotherapy); electrical stimulation of muscles with impaired innervation; balneo- and peloidotherapy.
After the acute pain syndrome has been relieved, approximately one week after arm immobilization, all patients are prescribed exercise therapy for median nerve neuropathy – to strengthen the muscles of the shoulder, forearm, hand and fingers and increase the range of their flexion and pronation.
Folk remedies
Among the means recommended for folk treatment of this pathology, pain-relieving compresses with blue clay, turpentine, a mixture of camphor alcohol with salt, and calendula alcohol tincture are offered. The effectiveness of such treatment, as well as herbal treatment (ingesting decoctions of elecampane or burdock roots), has not been assessed. But it is known for sure that it is useful to take evening primrose oil, as it contains a lot of fatty alpha-lipoic acid.
Surgical treatment
If all attempts to cure compression-ischemic neuropathy of the median nerve with conservative methods are unsuccessful, and motor-sensory disturbances do not go away after one to one and a half months, surgical treatment is performed.
Moreover, if neuropathy occurs after an injury due to the intersection of the nervus medianus, the operation to restore its integrity, that is, suturing or plastic surgery, is performed earlier - in order to avoid persistent limitation of the range of motion of the hand (contractures).
In carpal tunnel syndrome, surgical decompression of the median nerve (cutting the carpal ligament) or its release (neurolysis) with removal of compressive fibrous tissue is performed. The intervention can be performed by open access or endoscopically.
Contraindications to surgery for carpal tunnel syndrome are advanced age, duration of symptoms longer than 10 months, constant paresthesia, and stenosing tendovaginitis of the flexor muscle.
But supracondylar process syndrome is subject to surgical treatment only: for the purpose of decompression, an operation is performed to remove this bone growth.
Prevention
There is no specially developed method for preventing neuropathies.
Peripheral nerve diseases, including median nerve neuropathy, are in many cases unavoidable. What is possible? Try not to injure your limbs, treat joint inflammations in a timely manner, take B vitamins, and avoid gaining extra pounds…
And if your work involves prolonged stress on the elbow or wrist joints, you need to take short breaks and perform simple but effective exercises for the joints of the hands: they are described in detail (with illustrations) in the material - Carpal Tunnel Syndrome
Forecast


 [
[