Medical expert of the article
New publications
Melanoma in children
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Melanoma in children is a malignant skin tumor that grows very aggressively and metastasizes quickly. This pathology is related to childhood oncological diseases, the treatment of which is difficult. Fortunately, melanoma in children is very rare, so knowledge of the symptoms and main manifestations of the disease is very important for timely treatment.
Epidemiology
The epidemiology of melanoma is not very developed, since melanoma among all oncological pathologies of childhood accounts for less than one percent. But since this disease is not so widespread, its diagnosis is not always timely. In the age structure, melanoma in children under ten years old accounts for 5% of the total incidence of oncological diseases, and in children over ten years old, this figure is 15%. That is, melanoma is more common in children of prepubertal and pubertal periods.
Causes melanomas in a child
The reasons underlying the development of any oncological pathology cannot yet be determined precisely. Therefore, it is very difficult to talk about the obvious cause of melanoma in children. To find out what factors can influence the formation of melanoma in a child, it is necessary to understand the pathogenesis of this disease.
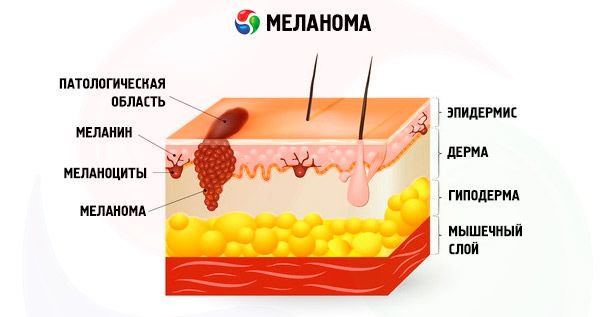
A child's skin consists of the epidermis, the skin itself or dermis and subcutaneous tissue. Each person's dermis contains melanin, a pigment that is responsible for skin color. If a person has little of this pigment, then his skin is light and not prone to tanning, and if there is a lot of melanin in the dermis, then the person may be dark-skinned. It is also necessary to say about pigment nevi or, as people say, moles. These are formations on the skin that are benign and consist of a cluster of several melanocyte cells. Under normal conditions, they do not change or grow. Melanoma is a skin tumor in which these melanocyte cells degenerate and become malignant. And the moment when such a degeneration occurs should be diagnosed in time.
 [ 10 ]
[ 10 ]
Risk factors
Taking into account all the reasons, it is possible to identify risk factors for the development of melanoma in children, given their young body and ability to correct various mutations. The main risk factors are as follows:
- Children with albinism are more susceptible to melanoma because their skin is not protected from the effects of ultraviolet radiation;
- a history of skin cancer or melanoma in the family, even in remote cases;
- mothers with harmful work factors during pregnancy with this child (paints, varnishes, chemical shops);
- Severe intrauterine infections or viral lesions may later cause mutation.
These are far from all the reasons for the development of melanoma, since it is impossible to determine them precisely, but these are the main ones, and it is necessary to take into account and prevent complications associated with this.
Pathogenesis
The pathogenesis of any oncological pathology is that a cell is affected by a mutagen. A mutagen is a factor (cause) that affects cell division. Under normal conditions, a cell at a certain point in time divides by mitosis, resulting in the formation of two new cells, and the old cell dies. If a cell is affected by a mutagen, then mitosis is disrupted and uncontrolled division occurs, in this case, melanocytes, and the old cell does not die. Such uncontrolled growth occurs very quickly, which leads to an increase in the number of melanocytes, and they interfere with the growth and reproduction of skin cells. Therefore, an excessive number of such malignant cells leads to dysfunction and rapid growth into the deep layers of the dermis.
Given this mechanism of melanoma formation, there can be many reasons, i.e. mutagens. The most powerful mutagens are viruses, which are capable of inducing changes in the cell nucleus and disrupting the normal division process. Chemical compounds that affect the skin can also be the cause. Given the direct effect on the skin itself, the main cause of melanoma development can be considered ultraviolet radiation. Since under the influence of rays, melanin is formed in the melanocytes themselves, this type of radiation can cause malignant growth of these cells. And we are not talking about excess radiation, but simply about its presence. Genetic predisposition is very important in the development of melanoma, because if there are certain genes, even the “lightest” antigen can trigger a reaction of abnormal division.
Symptoms melanomas in a child
The first signs of melanoma are always visible, since this is a malignant formation of external localization. And this pathology is diagnosed by parents quite widely, since they pay attention to the child during bathing or simply caring about health. Therefore, if you know exactly what to pay attention to, the symptoms of melanoma can be seen.
At birth, there are usually no moles. They begin to appear after some time and grow together with the child, but to a small size. At the same time, moles should be of the same color, usually brown, with smooth contours, without growths and various inclusions. With such signs, we are talking about a normal nevus or birthmark. Signs of melanoma can be a sudden onset of nevus growth, a change in its color and coloring, if it is paler in the center and lighter around. There may also be redness, itching, pain around the mole. If the edges and contours become uneven, pathological inclusions appear, or the child scratches the nevus area, then this is also a symptom of a possible malignant tumor. Therefore, it is important for the mother to remember that if the birthmark was the same all the child's life, and suddenly at least something in the characteristics of this mole changed, then only one sign can be a symptom of melanoma. With any such change, you need to see a doctor.
Skin melanoma in children can manifest itself in a different way. There are different types of melanoma, including non-pigmented melanoma, which is not associated with symptoms of changes in the nature of nevi. Therefore, such melanomas are more difficult to diagnose. In this case, the first clinical sign may be an increase in regional lymph nodes. The lymphoid system of a person, and especially a child, is very well developed and tries to limit and remove all unnecessary toxins and substances from the body. So with melanoma, the lymph nodes try to remove all malignant cells, and they accumulate there. So the main and only first symptom may be an increase in such lymph nodes. Then the child may complain of a lump in the groin or under the arm, pain.
Amelanotic melanoma in a child does not manifest itself on the skin in any way, but there is only an invasion into the deep layers of the skin, which can cause an imperceptible compaction. Depending on the immersion of melanoma into the depths of the dermis, different stages of melanoma in children are distinguished, which is important for assessing the prognosis and choosing a treatment method.
Stages
The stages of melanoma depend on which layers are involved in the process.
- Stage 1 is when malignant cells of altered melanocytes do not spread beyond the epidermis and do not penetrate the basement membrane; this is considered the most prognostically favorable stage;
- Stage 2 – the process spreads to the basement membrane of the epidermis;
- Stage 3 – spread to the papillary layer of the dermis, without invasion of the reticular layer;
- Stage 4 – tumor cells spread to the entire layer of the dermis;
- Stage 5 – the disease widely invades the subcutaneous fat tissue with regional and distant metastases.
Such staging can only be carried out after a thorough histological examination, and this subsequently allows us to establish the stage of the disease itself and determine the treatment.
The initial stage of melanoma in children is considered the most acceptable for a good treatment outcome. This is due to the fact that in this case there are no regional and distant metastases and removal of the primary tumor can lead to a complete recovery.
Complications and consequences
The consequences of untimely diagnosis of melanoma are very serious, because this disease is very prone to metastasis. Therefore, the most common complications can be metastases to the liver, which disrupts blood circulation. Therefore, there can be thrombosis of the hepatic vein, necrosis of liver cells. Among the remote consequences of melanoma and the treatment carried out, there can be a delay in the child's growth, a violation of the process of blood cell formation. The most serious complications can develop against the background of chemotherapy, which is manifested by anemia, a decrease in the number of leukocytes, infectious diseases, fungal lesions of the mucous membranes.
Diagnostics melanomas in a child
Early diagnosis of melanoma is equivalent to a full recovery, so it is very important that if a mother notices any changes in a birthmark, she should immediately consult a pediatric dermatologist.
For correct diagnosis, before examination, it is necessary to find out how such a nevus behaved throughout the child's life and from what moment it began to bother. It is necessary to ask the child's reaction to sunbathing and whether there are any changes in the nevi. It is also necessary to clarify the family history, whether there is skin cancer, melanoma, or any other oncopathology in the family, because there may be a genetic predisposition to mutation of the mitotic cell division gene.
When examining, you need to pay attention not only to what is bothering the mother at the moment, but to the condition of the child's entire skin. If the child is white and not prone to tanning, then you should pay attention to this, then the nevi will be clearly visible. You also need to pay attention to all other pigment spots for the purpose of differential diagnosis.
The tests that are performed for melanoma in a child are specific histological studies. Given that melanoma has a high risk of rapid metastasis, a puncture biopsy is strictly prohibited if melanoma is suspected. Therefore, an excisional biopsy is performed, that is, a smear-imprint of the skin is taken and examined under a microscope. Histological examination makes it possible to accurately diagnose melanoma. The appearance of cells with atypical nuclei, a violation of the mitosis process, and a violation of the structure of the skin tissue itself indicate that such a diagnosis is in favor. In parallel, various chemical reactions of staining such cells with different dyes are carried out, which allows us to distinguish between skin cancer and melanoma.
Instrumental diagnostics of melanoma is limited to differential diagnosis in complex cases, until the biopsy results are available. Dermatoscopy can be performed - this is a skin examination with a special device that magnifies several dozen times and allows you to see more serious changes in the skin and its appendages. This way you can see parasites or fungi that can cause lichen, which can be similar, for example, to non-pigmented melanoma.
If a child is diagnosed with melanoma, it is very important to conduct a comprehensive examination – computed tomography – to determine the stage. This method allows you to determine the damage to regional lymph nodes and determine the condition of the internal organs where melanoma can metastasize – for example, the lungs or liver.
Thus, if there is histological confirmation, then the diagnosis of melanoma leaves no doubt, and it is only important to determine the stage.
What do need to examine?
How to examine?
Differential diagnosis
Differential diagnostics of melanoma in children should be carried out with lymphadenopathy of infectious genesis, if the child has enlarged lymph nodes as a symptom of melanoma. If lymphadenopathy is infectious, then such nodes are moderately enlarged, symmetrical, can be painful and not fused with the surrounding tissues. Under the influence of antibacterial or other etiologic therapy, such nodes go away very quickly. If the cause is melanoma, then they are enlarged on one side, in accordance with its localization, and are huge in size, not fused with tissues.
Amelanotic melanoma should be carefully differentiated from lichen. Such melanoma may be accompanied by only a slight thickening of the skin, without visible external changes. Lichen is also accompanied by thickening, elevation above the skin with a slight rim of redness. In this case, it is necessary to conduct a dermatoscopy, and it is possible to see parasites or signs characteristic of lichen.
Melanoma is extremely rare in newborns, but often there are small hemangiomas that the mother does not pay attention to and does not treat. Then, over time, when the child grows, such hemangiomas also grow. They can be brown in color, with unclear contours, which is very similar to melanoma. Therefore, it is also necessary to clearly distinguish between these two pathologies, specifying the time of onset of symptoms and conducting additional studies.
Who to contact?
Treatment melanomas in a child
A special feature of melanoma treatment is that this malignant tumor is very poorly responsive to chemotherapeutic agents and radiation therapy. The main approach to treating melanoma in a child is the following: the initial stages of melanoma (first and second) are treated surgically, since at this stage the spread of the tumor allows it to be removed within healthy tissues. The higher the stage of the disease, the more methods are used - at the third and fourth stages, preference is given to a combined and comprehensive method.
For conservative therapy, medications are used according to the stage and treatment protocol. For this purpose, several cytostatics with different mechanisms of action are used at once. Such therapy is very aggressive towards both healthy tissues and cells of the child, given that this is a growing organism. Therefore, against the background of cytostatic therapy, many drugs are used to protect and maintain the function of the child's internal organs - antiemetics, probiotics, vitamins, parenteral nutrition drugs, antihistamines, antibiotics and antivirals. The main cytostatics used in the treatment of melanoma in children are Doxorubicin, Vincristine, Asparginase, Dacarbazine, Prospidin.
- Doxorubicin is an antitumor agent used in combination drug therapy for melanoma. The drug acts by inhibiting the synthesis of nucleic acids in malignant cells, which reduces their activity and division rate. Therefore, the drug reduces the number of malignant cells and leads to remission. To achieve the effect, long-term treatment with repeated use of drugs is required to completely remove malignant cells and block their proliferation. The dosage of the drug is always calculated individually for each treatment cycle. The main principle of dosage for children is the calculation of the drug per square meter of the child's skin area. This is determined by special tables that correspond to the age and weight of the child in relation to the body surface. The method of administration of the drug is intravenous with a clear dosage throughout the day by setting an infusion pump. The side effects of all antitumor drugs are very pronounced, since in addition to malignant cells, they also affect the cells of the body. Therefore, there is a decrease in the activity of reproduction of the epithelium of the intestine, stomach, blood cells, and the protective function of leukocytes.
- Vincristine is a drug used in the treatment of malignant neoplasms. The main active ingredient of the drug is a plant alkaloid, which acts by disrupting the mitotic division of malignant cells due to the destruction of the tubulin protein. This drug is used in combination therapy with an individual dosage for each child per square meter of body area. The method of application is intravenous only, preventing contact with the skin or outside the vein. Side effects are very common, the main ones are inflammation and ulceration of the oral mucosa and tongue, gastritis, intestinal digestion disorders, frequent inflammatory diseases of the pharynx, bronchi, anemia.
- L-asparaginase is a drug that is also used to treat malignant tumors in pediatric oncology. The drug works by reducing the amount of asparagine, which is needed by malignant cells to reproduce. With a deficiency of this amino acid, their mitotic activity decreases and the child goes into remission. The method of administration and dosage of the drug is the same as all antitumor agents. Side effects are frequent sore throats during treatment with the drug, paresthesia, abdominal pain, impaired motility, fungal complications, decreased general immunity and frequent viral and bacterial diseases.
- Dacarbazine is a drug for the treatment of skin and soft tissue tumors, which is used in pediatric oncology. The drug acts by inhibiting cell growth and reducing the activity of DNA synthesis. The method of administration of the drug is intravenous with an individual dosage for each child per body area. Side effects of the drug are expressed in the form of hepatitis, liver cell necrosis, toxic effects on the kidneys, a decrease in the level of all cellular structures of the blood and an effect on the growth of the child.
It should be clearly stated that for the treatment of melanoma, as well as any other tumor, combinations of at least four antitumor agents are used. Due to the different mechanisms of action of the drugs, the maximum effect of reducing the number of malignant cells is achieved. But such treatment is prescribed only by a pediatric oncologist, with mandatory long-term treatment in a hospital. In Ukraine, treatment of children with cancer, including children with melanoma, is free until the age of 18.
The use of antibiotics and antifungal agents against the background of such cytostatic therapy is considered mandatory, since the child develops a state of deep immunosuppression. A combination of drugs or monotherapy with broad-spectrum antibiotics is used. Sometimes interferon drugs are used to treat and prevent viral infections.
- Josamycin is an antibacterial agent from the macrolide group. Among the known drugs, it has the maximum activity due to its structure. The drug acts on cellular and intracellular forms of bacteria, so it can be used against the background of cytostatic therapy to prevent the development of diseases of the lungs, and the gastrointestinal system, and external skin infections. The method of administration depends on age and can be in the form of a suspension or tablets. It is prescribed to children over 3 years old and the dosage is 10 mg / kg / day on the first day, from the 2nd to the 7-10th day - 5 mg / kg / day 1 time per day. A mandatory condition is the use of probiotics against the background of such therapy and treatment for at least ten days. Side effects of josamycin are paresthesia, impaired skin sensitivity, numbness of the arms and legs, tremor, impaired bile outflow, as well as dyspepsia. Precautions - do not use in cholestasis or gallstone disease.
- Fluconazole is an antifungal agent used to treat complications associated with antitumor therapy in the form of fungal inflammation of the oral cavity, genitals, skin, and internal organs. When symptoms of fungal complications appear, it is recommended to immediately start with a dosage of 6 milligrams per kilogram of the child's body weight, and then on the fifth day, the dose can be halved. Method of administration: the drug is taken orally in tablet form. Side effects may include decreased appetite, impaired liver function, changes in heart rhythm, increased temperature, and decreased neutrophil levels.
Children undergoing chemotherapy receive vitamins in the form of injections, since they are very important for the normal development of healthy cells.
Physiotherapy treatment is not used in the acute period; it is possible to use different methods already at the stage of complete recovery only on the doctor’s recommendations.
Surgical treatment of melanoma in a child is used at the first stage of the disease, when the stage of melanoma invasion is the first or second. Then surgical intervention can ensure a complete recovery of the child. The scope of the operation is determined after a thorough examination and determination of the condition of the lymph nodes. If the lymph nodes are intact, then the scope of the operation is limited only to excision of the melanoma within healthy tissues. The operation for children is performed under general anesthesia. In this case, it is necessary to spare the skin itself, and remove the melanoma deeper into the subcutaneous tissue. The surgical material is necessarily sent for histological examination to determine the degree of invasion and the nature of the melanoma.
If the lymph nodes are affected, then surgical intervention is performed with excision of the melanoma and removal of regional lymph nodes with subcutaneous tissue.
Radiation therapy for melanoma is often used in combination therapy at stages three and four. It can be used before or after a planned surgical intervention, along with chemotherapy. Close-focus X-ray therapy or gamma therapy is most often used for treatment. Irradiation is administered locally and, if necessary, to the lymph nodes.
Folk treatment of melanoma in children
Folk treatment and the use of homeopathic medicines cannot cure melanoma or any other malignant formation. But folk methods are used against the background of drug therapy for a better effect and prevention of the development of infectious and other complications. For this purpose, herbs and folk methods are used that increase overall immunity.
- As a rule, children undergoing chemotherapy have a poor appetite, which further reduces the child's immunity and increases the risk of infectious complications. Therefore, in order to increase immunity and improve appetite, the following mixture is recommended. You need to take equal amounts of ginger root and orange zest and grate. After the gruel is mixed, you need to add five tablespoons of honey per 200 grams of such gruel and mix everything. After this, you need to add three grated walnuts and let it stand for four to five days. You need to take a teaspoon twice a day.
- Treatment of melanoma with aconite is known for its effect on malignant cells and a decrease in their proliferation. To do this, take fifty grams of aconite herb and pour hot water over it, leave for two hours. Take for twenty days, starting with one drop once a day and increasing the dose by one drop every day. Then, after the twentieth day of treatment, you need to reduce the dose of the medicine according to the same scheme. So the course of treatment is forty days.
- To prevent fungal infections during treatment for melanoma, it is recommended to rinse the child's mouth with a calendula solution after each meal.
Treatment of melanoma with herbs has not been proven, but this method is widely used because such herbal infusions help normalize digestion, appetite, and some of them normalize the processes of cell division.
- An infusion of herbs is good for children with melanoma to improve digestion and appetite. For the infusion, you need to take 20 grams of coriander, 20 grams of elecampane and twice as many leaves of stinging nettle. This solution needs to be boiled for half an hour and taken a tablespoon three times a day after meals.
- The effectiveness of white birch bark in the treatment of melanoma is proven due to its high content of antioxidants and tannins. To prepare the infusion, you need to boil the birch bark over low heat for two hours, then dilute the resulting decoction with warm boiled water in half and take a teaspoon up to five times a day.
- Elderberry, meadowsweet and centaury take one hundred grams of each plant and pour hot water over it. When the solution cools down, add honey and drink instead of tea.
Homeopathy in the treatment of melanoma can be used when remission is achieved. Preparations can be used to improve the immune status and normalize the general condition, prolong the period of remission. Concomitant immunotherapy helps the body cope with melanoma most effectively. The main homeopathic preparations in the treatment of melanoma that have an effect are the following:
- Arsenicum album is a homeopathic remedy used in the complex therapy of melanoma in children, which is located on the face and is accompanied by a sharp loss of body weight. The dosage in case of taking drops is one drop per ten kilograms of the child's body weight once a day. Side effects are possible in the form of hyperemia of the skin of the hands and feet, as well as a feeling of heat. Precautions - do not use in combination with drugs of bee origin.
- Acidum fluoricum is an inorganic homeopathic preparation based on phosphoric acid. The effectiveness of the drug has been proven by many studies, especially in the treatment of melanoma in older children and adolescents. The method of administration of the drug depends on the form. The dosage in case of taking drops is one drop per year of the child's life, and in case of taking capsules - two capsules three times a day. Side effects - burning tongue, sore throat or stomach, which goes away if you drink milk. Precautions - do not use if you have gastritis.
- Nosodes are a homeopathic remedy of natural origin. The method of administration of the medicine is enteral. The granules should be chewed until completely dissolved, it is not recommended to swallow them whole. The dosage is two granules twice a day. Side effects may occur in case of combination with iodine preparations - then there may be allergic reactions. Precautions - the drug cannot be used in case of severe diarrhea in a child.
- Silicea and sepia - a combination of these drugs in appropriate dilutions allows for effective treatment, especially with severe asthenia of the child and enlarged lymph nodes. The method of using drugs for children in the form of homeopathic drops and the dosage is four drops twice a day half an hour after meals at the same time. The course of treatment is three months. Side effects may be dizziness, so you need to take the medicine after meals.
Traditional methods of treatment are varied, but they cannot be used as priority methods of treatment.
Prevention
Prevention of melanoma development in children is very important today, since the culture of the process of tanning of small children has changed a little. Parents go on vacation with small children before they are one year old. But children under three years old are strictly prohibited from simple tanning in the sun, especially during active hours of ultraviolet radiation. It is necessary to hide children and not leave them to tan deliberately, since their thin skin is not protected and is not able to synthesize melanin so well. Therefore, the main measure of melanoma prevention in children is to avoid such active sun. If your child has many moles, then you need to carefully monitor them constantly and record any changes, because this can be the main symptom of the disease. All other preventive measures are also non-specific and consist of avoiding other possible harmful factors, especially during pregnancy.
Forecast
The prognosis for survival in children with melanoma is not very favorable, as the five-year survival rate is from forty to fifty percent. Remission with timely treatment occurs in 40% of patients.
Melanoma in children is a very rare disease, which is good given the high malignancy of this type of pathology. But it is also very difficult for a doctor to detect this pathology in time, until parents themselves pay attention to the health of their child. Therefore, if there are any changes in birthmarks in children that were not there before, you must definitely consult a doctor.

