Medical expert of the article
New publications
Intracranial hematoma
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
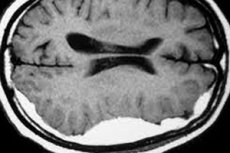
An intracranial or intracranial hematoma is a tissue-restricted, extravascular accumulation of blood that has leaked and then clotted between the brain membranes or into the brain tissue. This condition is considered potentially life-threatening.
Epidemiology
According to statistics, in craniocerebral traumas, hematomas between the dura mater and cerebral web are formed in 25% of cases, and intracerebral hematoma occurs in about 35 people per 100,000 population. In severe traumatic injuries, acute intracranial hematoma occurs, on average, in 20% of victims.
An epidural hematoma is identified in approximately 1-3% of closed head injury cases in children.
Causes of the intracranial hematoma
Traumatic intracranial hematomas are the most common, and brain injury (traumatic brain injury), including skull bone fractures and hemorrhagic cerebral contusion with blood vessel damage, are the most common causes of this condition.
For the most part, intracranial hematomas in children are also a consequence of traumatic brain injury. But they can occur spontaneously in the presence of hemorrhagic diathesis, in willebrand's disease, and intracranial neoplasms. In newborns, epidural hematoma may result from delivery by forceps or vacuum extraction. [1]
In addition, the etiology of intracranial hematoma may be related to a previous (remote in time) intracerebral hemorrhage in vascular lesions of the brain. [2]
Risk factors
Risk factors are considered to be age - elderly and children, chronically elevated blood pressure and constant intake of anticoagulants (acetylsalicylic acid preparations, etc.).
Also, the risk of hematoma (particularly subdural hematoma) is higher with:
- Cranial and brain surgeries (e.g., craniotomies);
- Arterial cerebral vascular aneurysm;
- Arteriovenous malformations cerebral vessels;
- Abnormalities of blood platelets involved in blood clotting - thrombocytopathies;
- Coagulopathy in the form of disseminated intravascular coagulation (DIC );
- Cortical vascular damage due to cerebral amyloid angiopathy;
- Idiopathic thrombocytopenic purpura;
- Acute lymphoblastic and sickle cell anemia.
Pathogenesis
Specialists explain the pathogenesis of intracranial hematoma formation by violation of the integrity of the walls of blood vessels (arteries, veins, capillaries), as well as convexital vessels (vessels of the convex surface of the large hemispheres) of the brain in the area of the frontal, temporal, parietal and occipital lobes) and blood leakage into the surrounding tissues.
In this case, at the first stage of the pathological process, blood clotting (coagulation) begins outside the vessel, caused by aggregation (adhesion) of platelets with the formation of a clot, which consists of erythrocytes, platelets and serum. At the next stage, phagocytosis of erythrocytes by macrophages and glial cells occurs, which leads to the release of hemoglobin of blood, which combines with oxygen molecules present in tissues and undergoes degradation with the formation of oxygenated hemoglobin (oxyhemoglobin) and by-products of its cleavage. In particular, free heme (the non-protein part of the hemoglobin molecule), which is embedded in cell membranes and has a cytotoxic effect on them in the form of oxidative damage.
In addition, intracellular deoxyhemoglobin (hemoglobin without bound oxygen) is formed at the edges of the hematoma and transformed into intracellular methemoglobin, which is unable to bind and transport oxygen. As a result, vasogenic extracellular edema of the surrounding brain tissue develops due to increased permeability of the blood-brain barrier. [3]
Symptoms of the intracranial hematoma
Most patients with epidural hematoma have increased drowsiness from the moment of injury, and one third of them lose consciousness. If the person remains conscious, the first signs arising from increased intracranial pressure and associated edema of brain tissue are manifested by progressive headache, nausea, vomiting, dilated and differently sized pupils, seizures (generalized convulsive paroxysms).
It should be borne in mind that in almost half of the cases there may be a short-term improvement followed by a sharp deterioration - a lucid interval in intracranial hematoma formed between the outer surface of the dura mater and the skull. The duration of this interval varies depending on the severity of the injury.
Against the background of loss of consciousness after traumatic injury, it is difficult to structure the clinical picture of subdural hematoma, because patients usually quickly fall into cerebral coma (which in almost half of cases ends lethally).
Most epidural and intracerebral hematomas and many subdural hematomas develop quickly and cause symptoms within a short period of time. Large hematomas press on the brain and can cause swelling and displacement of brain tissue - brain herniation - resulting in confusion and loss of consciousness, loss or increase in reflexes, unilateral or bilateral paralysis of the body, difficulty breathing and slow heart rate.
In addition, dizziness and loss of balance; difficulty with speech, concentration, and memory problems (especially with chronic hematoma in the elderly) have been reported with subdural hematoma. [4]
Forms
There are different types or kinds of intracranial hematomas such as: epidural (or extradural), subdural, and intracerebral (or intraparenchymal).
An epidural hematoma is usually associated with trauma, when a blood vessel is damaged and blood pools between the inner surface of the skull vault and the outer surface of the dura mater encephali. In 90% of cases, epidural hematoma is associated with a skull bone fracture, when blood is drawn either from the dura mater vessels (usually arterial) ruptured by the broken bone or from damaged intracranial venous sinuses.
The localization of a subdural hematoma is the subdural space that lies between the dura mater of the brain and the arachnoidea encephali - the arachnoid (spider) membrane. subdural hematoma can be acute (signs and symptoms usually appear immediately after the injury), subacute (symptomatology appears a few days after the injury) and chronic (with signs that may appear after a longer period of time). An enlarged hematoma causes compression of brain tissue and results in loss of consciousness.
When blood accumulates in the brain tissue itself, an intracerebral hematoma is diagnosed, and in 10% of severe closed traumatic brain injuries it is the primary cerebral lesion with the most frequent localization in the basal ganglia of the frontal and temporal lobes of the large hemispheres or in the cerebellum. In these hematomas, tissue damage is accompanied by edema, refractory intracranial hypertension and impaired function of neurons of the corresponding localization. [5]
Complications and consequences
Complications and sequelae of intracranial hematomas include:
- Cerebral edema;
- Brain compression;
- Elevated intracranial pressure;
- Hypoxia and cerebral ischemia.
Hematoma of the mesencephalon (midbrain) is complicated by acute ophthalmoplegia - uni- or bilateral.
Chronic subdural hematoma can be complicated by superficial cerebral hemosiderosis (deposition of heme-derived hemosiderin and other iron metabolites on areas of the brain) with sensorineural hearing loss, cerebellar ataxia (movement coordination disorders), and articulation problems.
The consequences of intracranial hematoma after a traumatic brain injury include not only significant neurologic problems, but also the threat of death due to compression and/or oxygen deprivation of the brain.
In birth trauma, intracranial hematomas in newborn infants can also lead to the death of the child. For example, in cases of massive subdural or intraparenchymal hematomas due to rupture of vessels in the region of the sickle-shaped venous sinus of the large brain or in the cerebellar peduncle in cases of compression on the fetal parietal bones during natural childbirth. Surviving infants may subsequently show signs of focal neurological deficits, in particular, epileptic seizures, convulsions (tonic or clonic), hearing impairment, speech impairment, etc., as well as other symptoms. [6]
Also read - brain hematoma and its consequences
Diagnostics of the intracranial hematoma
Diagnosis of intracranial hematoma is primarily diagnosis of brain injury.
To detect intracranial hematoma, instrumental diagnostics is performed, which, using computerized axial tomography (CT) or magnetic resonance imaging (MRI) of the brain, makes it possible to visualize reliable signs of intracranial hematoma - an extravascular accumulation of coagulated blood - and accurately determine its localization and size. For example, on CT, an acute subdural hematoma usually appears as a homogeneous, high-density sickle-shaped mass parallel to the inner surface of the skull.
CT angiography of cerebral vessels or digital subtractive angiography is also used.
Blood tests are necessary: general clinical and coagulogram.
To rule out intraventricular hemorrhage (bleeding in the ventricles of the brain), a analysis of the liquor is required. A hemorrhage will be indicated by a red color of cerebrospinal fluid, and a possible result of a spinal tap for intracranial hematoma: dark cherry or brown colored liquor.
In addition, differential diagnosis should exclude intracerebral hemorrhage - intracerebral hemorrhage, caused by hemorrhagic stroke or rupture of cerebral arteriovenous malformations; subarachnoid hemorrhage; hemorrhagic tumor; cerebral amyloid angiopathy with parenchymatous hemorrhages. [7]
Who to contact?
Treatment of the intracranial hematoma
Initial treatment consists of treating the brain injury with anti-edema and antiemetic medications and monitoring intracranial pressure. [8], [9]
Small hematomas that do not cause symptoms resolve on their own and do not require intensive treatment, but severe cases are treated surgically. Thus, most epidural hematomas and acute subdural hematomas require surgical intervention. [10]
The type of surgery depends on the type of hematoma. Options include:
- Surgical drainage (through a trepanation hole with subsequent placement of drainage in the subdural space);
- Skull trepanation (opening of part of the skull) - to remove large hematomas after severe traumatic injuries.
Prevention
Prevention of intracranial hematomas comes down to following safety rules and using protective gear in any situation that could lead to a brain injury.
Forecast
Intracranial hematoma can be life-threatening, and its prognosis is determined by both the degree of associated brain damage and the speed of its removal. Acute subdural hematoma is considered the most dangerous, as it results in significant cerebral damage and persistent neurologic sequelae.

