Medical expert of the article
New publications
Habitual miscarriage
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Miscarriage is a spontaneous termination of pregnancy between conception and 37 weeks, counting from the first day of the last menstrual period. Termination of pregnancy between conception and 22 weeks is called spontaneous abortion (miscarriage). Termination of pregnancy between 28 weeks and 37 weeks is called premature birth. According to the WHO nomenclature, the gestation period from 22 weeks to 28 weeks is considered very early premature birth, and in most developed countries, perinatal mortality is calculated from this gestation period. In our country, this gestation period is not considered premature birth or perinatal mortality, but at the same time, care is provided in a maternity hospital, not in a gynecological hospital, and measures are taken to care for a deeply premature newborn. In the event of its death, a pathological examination is carried out, and if the child survives 7 days after birth, this death is considered perinatal mortality.
Spontaneous abortion is considered one of the main types of obstetric pathology. The frequency of spontaneous miscarriages is from 15 to 20% of all desired pregnancies. It is believed that the statistics do not include a large number of very early and subclinical miscarriages.
According to the definition in force in our country, miscarriage is its interruption from the moment of conception to 37 full weeks (259 days from the last menstruation). This large time interval is divided into periods of early miscarriages (up to 12 weeks of pregnancy), late miscarriages (from 12 to 22 weeks); the period of termination of pregnancy in the period from 22 to 27 weeks, from 28 weeks - the period of premature birth. The classification adopted by WHO distinguishes between spontaneous miscarriages - pregnancy loss before 22 weeks and premature birth from 22 to 37 full weeks of pregnancy with a fetal weight of 500 g (22-27 weeks - very early, 28-33 weeks - early premature birth, 34-37 weeks - premature birth). In our country, spontaneous termination of pregnancy between 22 and 27 weeks is not considered premature birth, and the newborn child is not registered in case of death and data on him is not included in the perinatal mortality indicators if he did not survive 7 days after birth. In case of such spontaneous terminations of pregnancy, obstetric hospitals take measures to care for the extremely premature child.
According to the WHO definition, habitual miscarriage is considered to be a woman’s history of 3 or more consecutive spontaneous abortions before 22 weeks of pregnancy.
Epidemiology
Spontaneous pregnancy loss is a surprisingly common occurrence. Although approximately 15% of all clinically diagnosed pregnancies end in spontaneous loss, many more pregnancies fail before they are clinically recognized. Only 30% of all conceptions result in a live birth.[ 4 ],[ 5 ]
In sporadic miscarriage, the action of damaging factors is transient and does not disrupt the woman's reproductive function in the future. For example, an error in the process of gamete formation leads to the emergence of an abnormal egg and/or sperm and, as a consequence, to the formation of a genetically defective non-viable embryo, which can be the cause of a spontaneous miscarriage. In most cases, such a phenomenon is episodic and does not lead to repeated pregnancy losses.
At the same time, in the group of women who have lost their first pregnancy, there is a category of patients (1–2%) who have endogenous factors that prevent the normal development of the embryo/fetus, subsequently leading to repeated terminations of pregnancy, i.e. to the symptom complex of habitual miscarriage. [ 6 ] Habitual miscarriage accounts for 5 to 20% of miscarriages.
It has been established that the risk of pregnancy loss after the first miscarriage is 13–17%, which corresponds to the frequency of sporadic miscarriage in the population, whereas after 2 previous spontaneous abortions the risk of losing a desired pregnancy increases more than 2-fold and is 36–38%.
According to B. Poland et al., in women suffering from primary habitual miscarriage, the probability of a third spontaneous miscarriage is 40–45%.
Considering the increasing risk of losing a desired pregnancy with an increase in the number of miscarriages, most specialists dealing with the problem of miscarriage believe that 2 consecutive miscarriages are enough to classify a married couple as having a habitual miscarriage, with subsequent mandatory examination and a set of measures to prepare for pregnancy.
The influence of maternal age on the risk of early spontaneous miscarriages has been established. Thus, in the age group of 20–29 years, the risk of spontaneous miscarriage is 10%, while at 45 years and older it is 50%. Probably, maternal age is a factor contributing to the increase in the frequency of chromosomal abnormalities in the fetus.
Causes habitual miscarriage
Many researchers believe that spontaneous miscarriages in the first trimester are an instrument of natural selection, since when studying abortions, 60 to 80% of embryos are found with chromosomal abnormalities.
The causes of sporadic spontaneous abortion are extremely diverse and not always clearly defined. They include a number of social factors: bad habits, harmful production factors, unsettled family life, heavy physical labor, stressful situations, etc. Medical factors: genetic breakdowns of the karyotype of parents, embryo, endocrine disorders, malformations of the uterus, infectious diseases, previous abortions, etc.
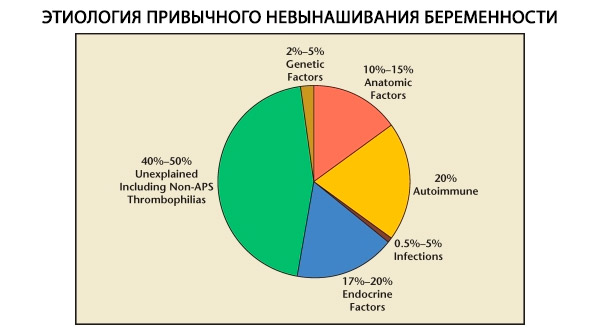
Habitual miscarriage is a polyetiological complication of pregnancy, which is based on dysfunction of the reproductive system. The most common causes of habitual miscarriage are endocrine disorders of the reproductive system, latent forms of adrenal dysfunction, damage to the receptor apparatus of the endometrium, clinically manifested as an incomplete luteal phase (ILP); chronic endometritis with persistence of opportunistic microorganisms and / or viruses; isthmic-cervical insufficiency, malformations of the uterus, intrauterine adhesions, lupus anticoagulant and other autoimmune disorders. Chromosomal pathology for patients with habitual miscarriage is less significant than in sporadic abortions, however, in women with habitual miscarriage, structural karyotype abnormalities occur 10 times more often than in the population and amount to 2.4%.
The causes of sporadic miscarriage and habitual miscarriage may be identical, but a married couple with habitual miscarriage always has a more pronounced pathology of the reproductive system than with sporadic miscarriage. When managing patients with habitual miscarriage, it is necessary to examine the state of the reproductive system of the married couple outside of pregnancy.
Read also: Habitual miscarriage - Causes
Diagnostics habitual miscarriage
Diagnostic evaluation should include maternal and paternal karyotypes, assessment of uterine anatomy, and evaluation for thyroid dysfunction, APS, and selected thrombophilias. Some women may require testing for insulin resistance, ovarian reserve, antithyroid antibodies, and prolactin abnormalities.
What tests are needed?
Who to contact?
Treatment habitual miscarriage
Treatment of threatened miscarriage in patients with habitual miscarriage (symptomatic therapy)
In the early stages of pregnancy, when pulling, aching pains in the lower abdomen and lower back occur in women with habitual miscarriage, along with pathogenetic therapy, treatment aimed at normalizing the tone of the uterus should be carried out. Up to 12 weeks of pregnancy, therapy includes:
- semi-bed rest;
- physical and sexual peace;
- antispasmodic drugs:
- drotaverine hydrochloride at a dose of 40 mg 2-3 times a day intramuscularly or 40 mg 3 times a day orally;
- papaverine hydrochloride at a dose of 20–40 mg 2 times a day rectally or 40 mg 2–3 times a day orally;
- magnesium preparation - 1 tablet contains magnesium lactate 500 mg (including magnesium 48 mg) in combination with pyridoxine 125 mg; average daily dose is 4 tablets - 1 tablet in the morning and afternoon and 2 tablets in the evening. The duration of treatment is determined individually depending on the symptoms of threatened miscarriage.
In the presence of partial detachment of the chorion or placenta (up to 20 weeks of pregnancy), along with antispasmodic therapy, hemostatic therapy is carried out with calcium preparations at a dose of 1000 mg/day, sodium ethamsylate at a dose of 250 mg 3 times a day orally or, in case of severe bleeding, 250 mg 3 times a day intramuscularly.
In case of heavy bleeding, tranexamic acid is used intravenously by drip at 5–10 ml/day in 200 ml of 0.9% sodium chloride solution for hemostatic purposes, followed by switching to tablets at a dose of 250 mg 3 times a day until the bleeding stops.
In the case of retrochorial and retroplacental hematomas at the organization stage, a complex preparation is used, containing bromelain 45 mg, papain 60 mg, pantheatin 100 mg, chymotrypsin 1 mg, trypsin 24 mg, alpha-amylase 10 mg, lipase 10 mg, ascorbic acid + rutoside 50 mg, 3 tablets 3 times a day 30 minutes before meals, a course of 14 days.
If pronounced tonic contractions of the uterus occur at 16–20 weeks of pregnancy, if antispasmodic drugs are ineffective, indomethacin is used rectally or orally at a dose of no more than 200 mg/day, for a course of no more than 1000 mg: 1st day - 200 mg (50 mg 4 times a day in tablets or 1 suppository 2 times a day), 2–3rd day 50 mg 3 times a day, 4–6th day 50 mg 2 times a day, 7–8th day - 50 mg at night.
Prevention
Women with a history of 2 or more miscarriages or premature births should be advised to undergo an examination before the next pregnancy to determine the causes, correct the disorders, and prevent further complications. Prevention methods depend on the causes underlying the habitual miscarriage.
Forecast
The prognosis will depend on the underlying cause of pregnancy loss and the number of previous losses. With identification of the cause, correction of abnormalities outside of pregnancy, and monitoring during pregnancy, the birth of viable children in couples with habitual miscarriage reaches 95–97%. Patients and doctors can be encouraged by the overall good prognosis, since even after 4 consecutive losses, the patient’s probability of carrying the next pregnancy to term is more than 60–65%.


 [
[