Medical expert of the article
New publications
Chronic alcoholic hepatitis
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Alcoholic hepatitis is an inflammatory process. It occurs against the background of heavy alcohol consumption. As a result, the organ is affected by toxins. The chronic form of the disease occurs 5-7 years after the onset of the inflammatory process. The scale can be serious, it all depends on the quality of the alcohol consumed and its quantity.
ICD-10 code
For convenience, a special international classification of the disease was created. Thanks to it, the diagnosis can be understood anywhere in the world. Simply put, this coding is used everywhere. Hepatitis is a disease of the digestive system.
K00-K93 Diseases of the digestive system.. K00-K14 Diseases of the oral cavity, salivary glands and jaws. K20-K31 Diseases of the esophagus, stomach and duodenum. K35-K38 Diseases of the appendix. K40-K46 Hernias. K50-K52 Non-infectious enteritis and colitis.
K55-K63 Other diseases of the intestine. K65-K67 Diseases of the peritoneum
K80-K87 Diseases of the gallbladder, biliary tract and pancreas. K90-K93 Other diseases of the digestive system
K70-K77 Liver diseases.
- K70 Alcoholic liver disease (Alcoholic liver disease, Liver cirrhosis).
- K70.0 Alcoholic fatty liver disease.
- K70.1 Alcoholic hepatitis.
- K70.2 Alcoholic fibrosis and sclerosis of the liver.
- K70.3 Alcoholic cirrhosis of the liver.
- K70.4 Alcoholic liver failure (liver failure).
- K70.9 Alcoholic liver disease, unspecified
- K71 Toxic liver injury.
- K72 Liver failure, not elsewhere classified (Liver failure).
- K73 Chronic hepatitis, not elsewhere classified (Hepatitis, chronic).
- K74 Fibrosis and cirrhosis of the liver (Cirrhosis of the liver).
- K75 Other inflammatory diseases of the liver.
- K76 Other liver diseases.
- K77 Liver disorders in diseases classified elsewhere
Causes of chronic alcoholic hepatitis
The name speaks for itself. The main reason for liver problems is heavy alcohol consumption. Regular consumption of alcoholic beverages in increased quantities will sooner or later affect the liver. Alcohol contributes to the disruption of oxidative processes in cellular structures. It has a toxic effect and disables the organ. Ultimately, cirrhosis of the liver may develop, requiring liver transplantation.
The minimum amount of alcohol that can cause inflammation is 20-30 grams regularly. This figure applies to the female population. For men, it is slightly higher and is 60-70 grams per day. As can be seen from these statistics, a very small amount of alcohol is enough to get serious problems. There are simply no other reasons that contribute to the development of inflammation. Alcohol is to blame for everything. Therefore, its consumption should be reduced to a minimum.
Pathogenesis
The toxic effect of ethanol leads to addiction. Ethanol has a special effect on the concentration of acetaldehyde and acetate in the blood. The oxidative process increases the level of NAD*H / NAD+. These indicators play an important role in the formation of fatty liver dystrophy. As soon as the concentration of the first indicator increases, there is an increase in the synthesis of glycero-3-phosphate. As a result, fatty acids begin to actively accumulate in the liver.
Acetaldehyde has a hepatotoxic effect. It manifests itself mainly due to the intensification of lipid peroxidation processes. Ultimately, the functions of cell membranes are disrupted. In combination with proteins, acetaldehyde leads to a change in the structure of hepatocyte microtubules. As a result, alcoholic hyalgin is formed. Intracellular transport is disrupted, and hepatocyte dystrophy occurs.
Increased formation of acetaldehyde leads to a decrease in the activity of mitochondrial enzymes. As a consequence, the synthesis of cytokines is significantly enhanced. Cellular immunity is significantly impaired. Ultimately, the liver is exposed to strong negative effects. An inflammatory process begins, functionality is undermined. As a result, alcoholic hepatitis develops, flowing into a chronic form.
There are different points of view regarding the terminology of this type of alcoholic liver damage. L. G. Vinogradova (1990) provides the following definition: "chronic alcoholic hepatitis" is a term used to designate relapses of acute alcoholic hepatitis that occur against the background of an incompletely completed previous attack of acute alcoholic hepatitis and lead to a specific liver damage with features of chronic hepatitis.
Histological examination reveals two forms of chronic alcoholic hepatitis: chronic persistent and chronic active. Morphologically, chronic persistent alcoholic hepatitis combines the characteristic features of alcoholic hepatitis with moderate pericellular and subsinusoidal fibrosis in the third zone of the acinar liver lobule, expansion of the portal ducts, portal fibrosis, and minor portal infiltration. The clinical picture includes decreased appetite, mild pain in the liver, belching, general weakness, slight enlargement of the liver, and a mild increase in the activity of γ-glutamyl transpeptidase in the blood serum.
Chronic alcoholic active hepatitis histologically combines the signs of alcoholic hepatitis with active fibrosis and hyaline necrosis in the liver lobules, bridging and multilobular necrosis are possible with high activity of the pathological process. Clinical manifestations are characterized by severe weakness, lack of appetite, pain in the liver, jaundice, enlarged, dense and painful liver, significant changes in liver function tests, in particular, high activity in the blood serum of y-glutamyl transpeptidase, aminotransferases, an increase in the content of immunoglobulin A in the blood.
Chronic alcoholic hepatitis can progress to liver cirrhosis even in conditions of abstinence from alcohol due to the addition of autoimmune mechanisms - sensitization of T-lymphocytes to alcoholic hyaline.
Chronic alcoholic hepatitis is a liver disease. Naturally, caused by heavy alcohol consumption. This disease needs to be eliminated, because in most cases it develops into liver cirrhosis. During the intake of alcoholic beverages, acetaldehyde is formed in the liver. It is this that severely affects liver cells. It can trigger a number of chemical reactions in the body and thus lead to organ damage.
Symptoms of chronic alcoholic hepatitis
The clinical manifestation of this disease is limited to scanty symptoms. Thus, the organ may slightly increase in size, and painful sensations appear. Severe pain and loss of appetite are possible. Over time, the symptoms are supplemented by nausea and vomiting. There are no physical data.
Often, there is a disturbance in the rhythm of sleep and wakefulness. A person experiences a decrease in libido, an increase in body temperature. A number of other signs can be identified. Thus, nails become white, spider veins appear, palmar erythema and ascites often develop. These changes are characteristic directly of the chronic form of the disease. The symptoms described in the first paragraph appear at the initial stage.
Chronic course is characterized by the severity of symptoms, as well as their diversity. They may well manifest simultaneously. If treatment is not started in time, a fatal outcome is possible. This occurs due to the rapid development of liver cirrhosis. Severe liver damage requires liver transplantation. The risk factor is present in people with low weight, jaundice and increased liver density. Alcoholic hepatitis together with these factors is fraught with aggravating consequences.
First signs
The danger is that the disease can be asymptomatic for a long time. Signs appear at severe stages. You can suspect something is wrong by liver dysfunction. A person begins to feel weak, he experiences increased fatigue, his appetite worsens, his body weight decreases sharply. These are the first signs that you should pay attention to. As a rule, pain syndrome does not particularly manifest itself at this stage. Therefore, a person most often thinks that his condition is associated with decreased immunity and other diseases. He is in no hurry to visit a doctor.
Over time, the pain syndrome begins to manifest itself. To a greater extent, it resembles discomfort and a feeling of heaviness in the right hypochondrium. Again, this situation does not particularly bother a person. After all, it is easy to think that low-quality products were consumed. Alcoholics, as a rule, do not understand that all troubles arise against the background of uncontrolled alcohol consumption. Gradually, nausea, vomiting and a bitter taste in the mouth are added to all the symptoms. There may be belching with bitterness. This symptom is associated with the use of alcohol and fatty foods.
Jaundice may also manifest itself. A yellowish tint of the sclera and the membrane of the oral cavity appears. As the disease progresses, yellowness of the skin occurs. Sometimes itching and an enlarged liver are added to this.
Where does it hurt?
What's bothering you?
Consequences
If the treatment was started on time, there can be no consequences. In most cases, everything ends successfully. If all recommendations are followed and alcoholic beverages are excluded, there can be no consequences. Otherwise, cirrhosis and liver fibrosis may develop.
Fibrosis is a reversible stage of the process. It can be eliminated with proper treatment. Cirrhosis cannot be cured, in this case, it is possible to get rid of the problem by organ transplantation.
If the treatment is started on time, and the transplantation has given a positive result, then the prognosis will be favorable. But, in no case should you drink alcoholic beverages. Otherwise, there is a risk of repeated inflammation. Therefore, you should always follow all the recommendations given and not deviate from them. Otherwise, a fatal outcome is possible. Whether or not there will be consequences depends directly on the patient in most cases.
 [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
[ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
Complications
It is necessary to understand that this inflammatory process has disappointing complications. The fact is that in most cases hepatitis develops into liver cirrhosis. It is impossible to cope with the problem at the drug level. Only transplantation is necessary here. Cirrhosis is equated to a malignant tumor in its severity.
Another complication may be ascites. It is also caused by hepatitis. The main sign of the problem is a strong protrusion of the abdomen. This is due to the fact that there is a large amount of free fluid in the human abdominal cavity. The type of ascites is completely determined by the amount of this fluid. With a small form, it can be 3 liters, average - more than 3 liters. With a high form, the amount of fluid varies up to 20-30 liters. A person is not able to move normally, there are some difficulties.
It should be understood that ascites is an alarming signal. It indicates that the organ is unable to filter blood. This moment cannot be missed. Otherwise, the patient will live no more than 5 years.
Diagnosis of chronic alcoholic hepatitis
The first step is to collect a history of the disease and complaints. It is important to determine how long ago the symptoms began. Important information is the amount of alcohol consumed and its frequency. It is important to collect a life history. Does the patient have any chronic processes in the body, are there any hereditary diseases. The presence of bad habits, tumors and contact with toxic substances are also taken into account.
Then a physical examination is carried out. During the examination, the skin tone, the size of the abdomen, and the presence of spider veins on the body are taken into account. When palpating, the person feels pain in the abdomen. Thus, it is possible to palpate the enlarged organ. It is important to assess the patient's mental state.
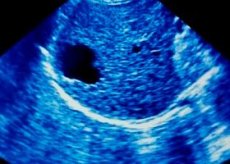
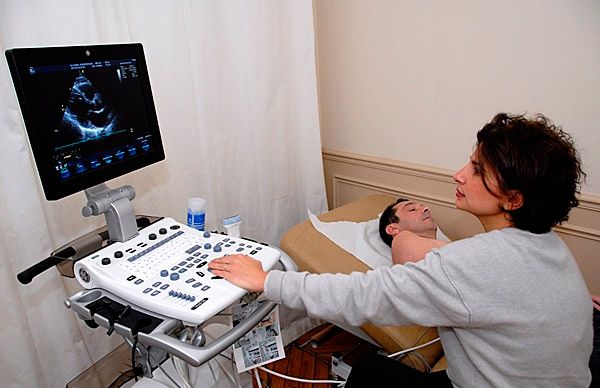
If necessary, an ultrasound is performed. The full picture consists of laboratory tests, instrumental and differential diagnostics. Detailed information will be provided below.
Tests
Laboratory tests play an important role. They include a general blood test. Thanks to it, the level of red blood cells and hemoglobin can be determined. It is easy to detect leukocytosis.
In addition to the general analysis, a biochemical blood test is taken. It allows you to evaluate the functionality of the liver and pancreas. Biochemical markers. They are used to check blood clotting indicators, the work of gamma-glutamyl transpeptidase. Aliproprotein A1 is monitored. It can be used to determine the condition of the liver. If proline and oxyproline are significantly increased in the blood, then, most likely, liver fibrosis is present. This condition is characterized by the growth of scar tissue.
A coagulogram is also widely used. It is an analysis of the coagulability of blood systems. A lipidogram is a study of fat-like substances in the blood. Long-term alcohol use can be determined by laboratory signs. A person has significantly increased activity of gamma-glutamyl transpeptidase, immunoglobulins, aspartate aminotransferase.
To get a complete picture, markers are determined. These are specific indicators that allow you to determine the presence of inflammatory processes in the liver that were caused by special viruses. A general urine test is also taken. It allows you to determine the general condition of the kidneys and urinary system. A coprogram is also performed, in other words, a stool analysis for the presence of undigested food fragments and fat.
Instrumental diagnostics
This research method is diverse. Thus, most often they resort to the help of ultrasound. This will allow to assess the condition of the abdominal organs and notice any changes in them.
Esophagogastroduodenoscopy is widely used. It is a diagnostic procedure during which a specialist can assess the condition of the esophagus as a whole. This allows pathologies to be identified. The stomach and duodenum are subject to examination. The study is carried out using a special instrument - an endoscope.
In addition, a puncture biopsy is performed. For this, a damaged piece of liver is taken and carefully examined. This allows the structure of the organ to be assessed and the correct diagnosis to be made.
Spiral computed tomography is widely used. This method involves obtaining X-ray images at different depths. The study allows you to get an accurate image of the affected area. Magnetic resonance imaging has a similar effect. This method is built on the chain of interaction of the human body with liquid. It allows you to get a clear image of the organ being examined.
Elastography. This method allows you to examine liver tissue. Everything is done with a special device that allows you to determine the presence of liver fibrosis. During the procedure, special compression of the tissue being examined is carried out. As a result, it is possible to see changes. Most often, the procedure is used as an alternative to biopsy.
Retrograde cholangiography. This method is based on the introduction of contrast. It is usually introduced into the Vater's papilla. The procedure allows to determine the deterioration of bile outflow. Cholangiography is performed on people with pronounced cholestasis syndrome.
Differential diagnostics
This type of diagnostics includes laboratory tests. Initially, a person needs to take a general blood test, as well as a biochemical blood test. The level of leukocytes, hemoglobin and erythrocytes can determine the presence of deviations and inflammation. Particular attention is paid to blood clotting.
In addition to this procedure, a biopsy is performed. It allows you to take a sample of the affected tissue and examine it. This method is the most reliable, but it only works in combination with blood tests.
To determine the condition of the urinary system, a urine test is taken. It is important to determine the presence of markers. In addition, a stool test is performed to determine the presence of coarse dietary fiber or undigested food fragments. It is impossible to get a complete picture using instrumental or diagnostic methods alone. All studies must be carried out together.
What do need to examine?
Who to contact?
Treatment of chronic alcoholic hepatitis
First of all, a person needs to give up drinking any alcoholic beverages. Naturally, this is an unbearable burden for an alcoholic. Therefore, it will have to be controlled. Because sooner or later all this will flow into cirrhosis of the liver. This is a very serious lesion, which most often ends in death.
It is worth visiting a psychologist and a narcologist. This will help you get rid of the addiction and understand the severity of the whole process. After all, in most cases, a person is unable to cope with the problem on their own. All patients must strictly adhere to diet No. 5. Its purpose is to reduce the load on the diseased organ. That is why fatty, fried and spicy dishes are considered prohibited foods. You should give up salted foods, canned goods, sweets and strong teas. Preference is given to food that contains a lot of fiber, vitamins and minerals.
Naturally, it is impossible to do without medications. However, in this case, you need to be especially careful. Because medications should have a positive effect on the organ and not injure it. Most often, hepatoprotectors are prescribed. This is a group of drugs that can regenerate liver cells and protect it from negative effects. It is mainly recommended to use Ursosan, Essentiale N, Heptral and Rezalut Pro. The course of treatment does not exceed one month. Detailed information about medications will be provided below.
It is important to fill the person's diet with vitamins and minerals. Herbal teas, including those based on echinacea and mint, will be useful. If a person is bothered by an overexcited and stressed state, it is worth drinking a sedative. Valerian can act as such, but only in tablets! Tincture should not be consumed under any circumstances! 2 tablets 3 times a day are enough. In case of severe liver damage, when cirrhosis is observed, it is worth resorting to organ transplantation. Otherwise, the person will not survive.
Medicines
As medicinal preparations, it is recommended to use those whose action is aimed at protecting the liver, as well as regenerating its cells. Therefore, patients are most often recommended to use Ursosan, Essentiale N, Heptral and Rezalut Pro.
Ursosan. The dosage of the drug is prescribed by the attending physician. In particularly severe cases, 14 mg per kilogram of weight is used. The duration of therapy can be from one month to six months. In some cases, 2 years. Contraindications: hypersensitivity, pregnancy, impaired liver and kidney function. Side effects: pain in the liver, nausea, vomiting, allergic reactions.
Essentiale N. The dosage is 2 capsules 3 times a day. The duration of therapy depends on the person's condition. Contraindications: hypersensitivity. Side effects: intestinal upset may occur very rarely.
Geptral. The drug can be used both in the form of tablets and injections. With prolonged therapy, the daily dose should not exceed 4 tablets. If the drug is administered, 400-800 mg is sufficient. The duration of treatment is determined by the doctor. Contraindications: hypersensitivity. Side effects: heartburn, nausea, sleep disorders, allergic reactions.
Rezalut Pro. The drug is used 2 capsules, 3 times a day before meals. The duration of treatment depends entirely on the course of the disease. Contraindications: hypersensitivity, antiphospholipid syndrome. Side effects: diarrhea, allergic reactions.
Folk remedies
Traditional medicine has a lot of useful recipes. Many herbs, fruits, plants and roots can be used for treatment. However, some of them can be toxic. Therefore, independent use can lead to a lot of unpleasant consequences. Before starting treatment, it is worth consulting a specialist.
Recipe 1. Blueberries. The beneficial properties of this berry have been known for a long time. Its leaves contain special enzymes that help fight hepatitis. Many healers recommend using blueberry decoctions. You can use fruit drinks, juices, or just eat the berry. Even jam will have a positive effect. The leaves themselves have special power. They can block viruses and protect the organ.
Recipe 2. Pumpkin. It is useful for minerals and vitamins. Its pulp can be used both for treatment and simply for nutrition. It is worth noting that it is not recommended to use it for more than 3 months. Traditional healers recommend eating it fresh, about half a kilogram per day. You can cook porridge, stew it, and also eat it in the form of candied fruit. Raw pumpkin is especially useful with sour cream. You can drink pumpkin juice. Pumpkin treatment is useful for cirrhosis of the liver.
 [ 23 ], [ 24 ], [ 25 ], [ 26 ]
[ 23 ], [ 24 ], [ 25 ], [ 26 ]
Herbal treatment
Medicinal herbs have a positive effect on many organs and systems. But it is important to understand which of them can be used and which ones to avoid.
Recipe 1. Dandelion grass. It can be used to eliminate many diseases. Especially those associated with liver failure. When treating hepatitis, dandelion grass should be consumed fresh. Salads are quite suitable. You can eat jam from them. Dandelion has a choleretic effect. A decoction of it should be consumed before each meal, half a glass. It is prepared simply, take dandelion leaves and pour boiling water over them. Then let the remedy brew and cool. To combat hepatitis, use the root of the plant. It should be crushed and evaporated for an hour. Then use a tablespoon before meals.
Recipe 2. You need to take St. John's wort, calendula flowers, and chicory. Mix all this and take only 2 tablespoons of the mixture. Then pour them with two glasses of cold water. Infuse everything overnight, boil for 5 minutes in the morning and strain. You can drink the remedy regardless of food intake. The course of treatment is 2 months.
Recipe 3. Take horsetail, yarrow and rose hips. It is important that everything is in equal proportions. After that, mix everything and take only one tablespoon. Pour a glass of boiling water over the mixture and leave for 2-3 hours. The resulting remedy can be consumed 3 times a day 30 minutes before meals. The duration of treatment is 2 weeks. If necessary, the course is repeated after a month.
Homeopathy
Homeopathic remedies have always been in demand. However, they are not suitable for everyone. Thus, there are both positive and negative opinions about them. Among homeopathic remedies, only a few are able to help. Thus, the following remedies have gained particular popularity: Hepel and Galstena. They have a positive effect, but only if used under the supervision of an experienced homeopath. The main action of the remedies is aimed at regenerating liver cells and creating a protective barrier around it. Therapy with the drugs is long-term. It is worth noting that monopreparations have always been distinguished by a special tropism for liver cells. Among them, it is worth noting May celandine and milk thistle. These two drugs are able to eliminate most of the symptoms that occur with liver damage. In addition, they support it.
The negative opinion is that not all people resort to homeopathy. More precisely, it is not able to help everyone. The fact is that homeopathic remedies do not undergo any clinical trials, so it is difficult to say whether there will be a positive effect.
Surgical treatment
Surgical treatment means liver transplantation. This operation is not only complicated, but also expensive. Such intervention is appropriate only if a person has liver cirrhosis or the last stage of liver failure.
A quality transplant can only be performed in German clinics. As mentioned above, the procedure is really expensive. The complexity of this operation lies not only in the price, but also in finding a donor, because finding a person with good physical and mental abilities is not always so easy. Some people stand in line for a new organ for years and do not always wait for it.
The operation itself is complicated. The recovery period is very long. It is necessary to monitor the condition of the person and the organ. After all, it takes a long time to take root and this is not always possible. Naturally, it is best not to resort to such an operation. No one gives a 100% positive result. To avoid such a need, you should simply exclude alcohol consumption and promptly treat pathological and inflammatory processes in the body.
More information of the treatment
Drugs
Prevention
Prevention of alcoholic hepatitis is the only way to avoid this problem. After all, the treatment is not only long-term, but also complicated. Moreover, during the recovery period, many difficulties may arise. First of all, you should exclude the consumption of ethanol-containing drinks. In this case, we mean alcoholic drinks of any percentage. The daily dose of consumption for a woman should not exceed 20 grams, and for a man 40 grams. If these figures are significantly higher, the likelihood of developing alcoholic hepatitis also increases.
The only way to avoid this problem is to completely give up alcohol. If a person drinks it periodically, it is difficult to draw conclusions about his health. The development of alcoholic hepatitis depends entirely on the amount drunk, the person's lifestyle and the nature of his diet. Naturally, a special place is given to the condition of the liver. It may not be in the best shape from the start, and alcohol will only worsen the situation.
Forecast
The prognosis depends entirely on the liver condition and the stage of the disease. The best prognosis is observed in the presence of alcoholic fatty degeneration. This condition is characterized by the presence of fat droplets inside the liver cells. This occurs under the influence of alcohol. It is not so difficult to eliminate this problem. Therefore, the prognosis is usually favorable.
A negative course is observed in liver cirrhosis. The problem in this case can only be eliminated by means of transplantation. Medicines are unlikely to have the necessary effect. In cirrhosis, the prognosis is unfavorable.
A positive course is possible only if a person completely refuses to drink alcohol and begins timely treatment of inflammatory processes in the body. Young age and normal body weight also affect the favorable prognosis. Finally, the disease proceeds much more favorably in men than in women.

