Medical expert of the article
New publications
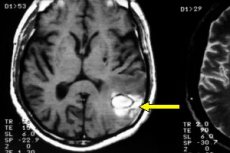
Cavernoma of the brain
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Abnormal brain vessel masses belong to cerebrovascular diseases, and one of them is cerebral cavernoma.
There are several alternative names for this cavernous cluster of abnormal blood vessels, which is a cavernoma (from Latin caverna - cave, cavity): cavernous angioma (i.e. Vascular tumor), cavernous hemangioma (tumor from blood vessels), venous malformation or cerebral cavernous malformation (from Latin malus - bad and formatio - formation). [1]
Epidemiology
It is believed that 0.4-0.8% of the population have cerebral cavernoma, and this pathology accounts for 8-15% of all vascular malformations of the brain and spinal cord. Symptomatic malformations account for at least 40-45% of cases, they are diagnosed at the age of 40-60 years, but in 25% of cases a cavernoma is detected in a child or adolescent. [2]
Almost half of cavernous malformations are detected accidentally: during brain scans when visiting a doctor with neurological complaints. [3]
Causes of the cavernomas of the brain
What are the causes of this type of cerebral vascular formation? Its etiology is associated with intrauterine disruption of the formation of the endothelium lining the inner surface of blood vessels, which is caused by specific mutations or deletions of certain genes.
The so-called familial forms of cavernoma account for 30-50% of all cases, and associated genes that encode proteins that interact at the endothelial cell junction include: CCM1 (KRIT1); CCM2 (MGC4607); CCM3 (PDCD10). For example, mutations in the CCM3 gene, which can be inherited in an autosomal dominant pattern, are thought to be predetermined in the formation of cavernomas in the brain and spinal cord, manifested in childhood by multiple cerebral hemorrhages.
Multiple cavernomas occur in 15-20% of cases, diagnosed as multiple cavernomatosis - with onset of symptoms at an earlier age with an increased risk of bleeding.
However, cavernomas can also develop sporadically (de novo appearance) - without clearly defined causes. In some cases, they are associated with ionizing radiation, for example, in childhood radiation therapy of the brain. [4]
Specialists also take into account the fact that in a significant proportion of patients the appearance of cerebral cavernoma occurs in the presence of such a congenital malformation as venous developmental anomaly (DVA) - venous angioma of the brain, since all sporadic cavernous masses form near the abnormal vein. [5]
The size of a cerebral cavernoma can vary from a few millimeters to several centimeters. Most often it is localized in the supratentorial region (in the brain), can be found in the white matter or adjacent to the cerebral cortex, and in 20% of cases the anomaly is found in the infratentorial region - in the cerebellum and the zone of the posterior cranial fossa. The same vascular malformation can form in the spinal cord - a cavernoma of the spinal cord.
See also - cavernous angioma
Pathogenesis
Researchers continue to elucidate the pathogenesis - molecular mechanisms of cerebral vascular malformations.
Although a cavernoma can enlarge, it is not a cancerous tumor but a benign vascular mass-a type of venous malformation without hyperplasia of endotheliocytes (endothelial cells).
Histologically, cavernomas are round/oval capsule-free formations consisting of irregularly dilated thin-walled capillary-like vessels with cavities lined by endothelium (with no fibers in the intercellular matrix).
In these tumor-like masses, which look like a small raspberry or mulberry, there is no brain tissue or intense arterial blood flow. However, thrombosis, deposition of hemosiderin, a breakdown product of blood hemoglobin, and replacement of nerve cells by glial cells (reactive gliosis) may be observed in the adjacent brain parenchyma.
Different theories of the pathogenesis of cerebral cavernous malformation are considered - taking into account the peculiarities of the structure and functions of brain capillaries in the blood-brain barrier; with possible stenosis of basal and collecting veins due to developmental venous anomaly (DVA); increased pressure in the cerebral capillary bed; microbleeding into the surrounding tissues; and proliferation of endotheliocytes and fibroblasts originating from the germinal mesenchyme. [6]
Symptoms of the cavernomas of the brain
As a rule, in small cavernomas, symptoms are absent for a long time or throughout life, but when the size of the malformation increases, the nature of the symptomatology and its intensity depend on the localization of the vascular formation. These include headaches, dizziness, weakness in the limbs, balance problems, sensory disorders (paresthesias), etc.
Experts associate partial seizures and epileptic seizures with microbleeding in cavernomas at the surface of the hemispheres or lobes of the brain. And only brainstem and spinal cord cavernomas do not cause such seizures. But among the symptoms of cavernous malformation of the brainstem are noted: ataxia (impaired coordination of movements), impaired muscle tone, unilateral facial nerve paralysis, double vision.
A cavernoma in the medulla oblongata, the lowest part of the brain stem, can cause spasms of the diaphragm that resemble continuous hiccups, and in some cases dysphagia (trouble swallowing).
A cavernoma of the pontine bridge, which is a section of the brain stem, can interfere to some extent with the transmission of nerve impulses between the cerebellar cortex and the cerebellum and disrupt the functioning of the nuclei of several cranial nerves. Because of this, the clinical picture of such a cavernoma may include: vestibular problems and difficulties in standing and moving, rhythm and proportionality of movements, and hearing problems.
A wide range of symptoms has a frontal lobe cavernoma: from seizures, impaired voluntary and purposeful movements (with the inability to coordinate them), problems with speech, writing and abstract thinking to deeper cognitive disorders and pronounced inertia, as well as up to catatonic immobility.
In addition to seizures, right frontal lobe cavernoma may be accompanied by migraine headaches, pseudodepressive/pseudopsychopathic syndrome. In right-handed people, left frontal lobe cavernoma can cause a state of apathy, articulation-related speech disorders, memory impairment and problems with logical thinking.
A right temporal lobe cavernoma can manifest itself with epileptic seizures, speech disorders, memory loss and hallucinations. If the patient has a left-sided temporal lobe cavernoma, in addition to epileptic seizures, he or she has difficulty recognizing and identifying sounds.
Among the symptoms that can be manifested by a parietal lobe cavernoma are sensory disturbances of the upper extremities, astereognosis and decreased ability to orient in space; apraxia (difficulty in performing purposeful actions) develops; memory and concentration of attention decrease.
A large cerebellar cavernoma has a negative impact on cerebellar function, manifested as vestibulo-atactic syndrome, and affects the ability to perform stereotyped and purposeful movements. In addition, cerebral cavernous malformation of this localization may lead to dizziness or nausea, tinnitus or hearing impairment.
In cases where the cavernoma is localized in the spinal cord, numbness, weakness, problems with movement and sensitivity in the extremities (numbness or burning), paralysis and loss of bowel and bladder control may develop. [7]
Complications and consequences
The most serious complication of this cerebral malformation is intracranial hemorrhage of the cavernoma - into the brain membranes or subarachnoid hemorrhage - with a clinical picture as in hemorrhagic stroke. And it usually leads to an increase in the size of the cavernoma and worsening of symptoms, but there is also a high risk of death.
The most common sequelae of temporal lobe cavernoma of the brain include neuropsychiatric disorders such as epileptogenic encephalopathy and temporal lobe epilepsy.
Diagnostics of the cavernomas of the brain
It is impossible to diagnose a cerebral cavernoma based on the patient's symptoms. Imaging, i.e. Instrumental diagnostics is necessary: CT and ultrasound encephalography, high-resolution magnetic resonance imaging - MRI of the brain, angiography of the brain and spinal cord.
Genetic testing may be performed to determine the etiology of the disease.
Differential diagnosis
Differential diagnoses include: cerebral arterial aneurysm and amyloid angiopathy; cerebral vasculitis; glioma, medulloblastoma and other cerebral malignancies; primary hemorrhagic tumors (ependymoma, glioblastoma) and hemorrhagic metastases to the brain; hippel-Lindau disease.
Who to contact?
Treatment of the cavernomas of the brain
It should be understood that the treatment of cavernomas by medication is aimed at alleviating the existing symptoms, since there are no pharmacological means for "resorption" of cerebral vascular malformation.
Therefore, various medications are prescribed to treat headaches, and anticonvulsants - antiepileptic drugs - help control seizure attacks.
However, not all patients have epileptic seizures that are treatable - due to resistance to pharmacologic drugs.
Most cavernomas are treated conservatively by observing the patient's condition and monitoring clinical symptoms, periodically visualizing the vascular mass.
Surgical treatment is performed if seizures cannot be controlled, there has been a cavernoma hemorrhage and there is a risk of recurrence. Many neurosurgeons consider it necessary to remove a de novo cavernoma as well as growing malformations.
In such cases, taking into account the size and location of the cavernoma, it is surgically resected. And when the localization of the mass makes neurosurgical intervention difficult or dangerous, stereotactic radiosurgery is used, where precisely dosed gamma radiation - the so-called gamma knife - is directed directly at the cavernoma. [8], [9]
More information in the material - angioma of the brain
Prevention
There are currently no measures to prevent the development of this cerebrovascular disease.
Forecast
The prognosis regarding the outcome of the disease depends on the size of the cerebral malformation, the presence of symptoms and complications, and the rate and extent of its enlargement.
Is it accepted in the army with a cavernoma of the brain or spinal cord? If this malformation is detected, then even in the absence of symptoms, the passage of military service in the presence of such pathology raises doubts of medics.

