Medical expert of the article
New publications
Facial nerve palsy
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Epidemiology
Facial nerve paralysis occurs relatively often. This may be due to its anatomical features: the nerve passes through narrowed openings in the bones of the facial part of the skull. This causes its compression and subsequent paralysis.
Most often, one branch of the facial nerve is affected, but 2% of patients are diagnosed with bilateral paralysis.
Every year, there are 25 cases of the disease per 100 thousand people in the world, and both men and women suffer equally.
The highest percentage of morbidity is observed in the off-season – from autumn to winter, as well as in the winter period.
According to prognostic data, the work of facial muscles is fully restored in most cases. This occurs within 3-6 months. In 5% of patients, innervation is not restored, and in 10%, repeated nerve damage is possible after a certain period of time.
Causes facial nerve palsy
Experts cannot yet name the exact cause of facial nerve paralysis, but the disease is often caused by infectious viral pathologies:
- herpes infection;
- chickenpox and shingles virus;
- adenovirus infections, acute respiratory viral infections, influenza;
- Epstein-Barr virus infection (mononucleosis);
- damage by cytomegalovirus;
- defeat by the Coxsackie virus;
- rubella.
In addition, hypothermia, alcohol abuse, hypertension, head injuries (face, ear), tumor processes in the brain, dental diseases, diabetes, atherosclerotic changes in blood vessels, severe stress, otitis or sinusitis can be a trigger for the development of facial nerve paralysis.
Risk factors
Most often, facial nerve paralysis occurs in the following cases:
- during pregnancy or in the postpartum period;
- during viral epidemics;
- in old age, especially if the immune system is weak.
Cases of a familial type of the disease have been described, which suggests the presence of a genetic predisposition to the development of facial nerve paralysis.
Pathogenesis
The facial nerve is the 7th paired cranial nerve, which controls the facial muscles responsible for speech production, facial expressions and chewing. Paralysis of this nerve can occur as a result of an inflammatory process, which leads to spasm of the arterial vessels with stagnation of blood flow in the capillary network. The capillaries become permeable, the tissues around them swell, and compression of the venous and lymphatic vessels occurs. This provokes a violation of blood and lymph flow.
As a result of all the above processes, the nutrition of the facial nerve, which is very sensitive to oxygen starvation, deteriorates. The nerve trunk increases in size, and the transmission of nerve impulses along it deteriorates. When the brain sends a command to the muscles for a certain action, they do not receive it and do not react. This explains the characteristic manifestations of the disease - inactivity of some facial muscles.
 [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
[ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ]
Symptoms facial nerve palsy
In any case, facial nerve paralysis begins acutely, with a sharp deterioration in the condition.
However, the first signs can be detected at the initial stage of paralysis, 1-2 days before visual manifestations. These may be the following symptoms:
- pain behind the auricle, radiating to the occipital region or facial area;
- pain in the eye on the affected side.
The first signs are associated with increasing swelling of the nerve column and its gradual compression.
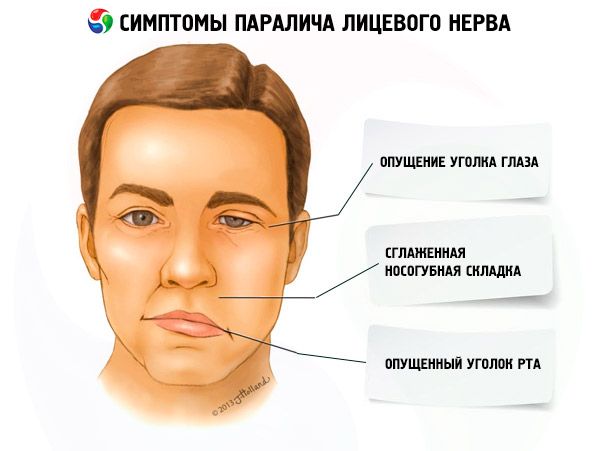
The following symptoms are more pronounced:
- facial symmetry is disrupted;
- the affected side attracts attention with its lack of emotionality and facial expressions;
- on the affected side, one can observe a drooping corner of the mouth, a smoothed nasolabial fold, and the absence of frontal folds;
- the violation of facial symmetry intensifies during the patient’s attempts to speak, smile, or cry;
- the upper eyelid on the affected side does not close completely, and the eye looks upward;
- liquid food and drinks cannot be retained in the mouth and spill out of the affected side of the oral cavity; chewing and swallowing functions are not impaired;
- while chewing, the patient, not feeling his own cheek, may bite it from the inside;
- the mucous membrane dries out, salivation often decreases (sometimes the opposite happens);
- speech function is impaired due to inactivity of certain areas of the lips and oral cavity;
- the eye on the affected side is half-open or completely open, the blinking function is impaired, the mucous membrane dries out (less often the opposite happens - profuse lacrimation);
- there is a disturbance of taste sensations on the affected side of the tongue;
- Hearing on the affected side increases, sounds are perceived louder than usual.
By assessing the clinical symptoms of the disease, the doctor can determine which part of the facial nerve is damaged. Depending on this, the following types of facial nerve paralysis are distinguished:
- Damage to the cerebral cortex responsible for the function of the facial nerve manifests itself in paralysis of the facial muscles of the lower part of the face, nerve and muscle twitching. At the same time, symmetry is visually restored during a smile.
- Damage to the facial nerve nucleus is accompanied by nystagmus, inability to wrinkle the skin on the forehead, numbness of the skin on the affected side, muscle twitching in the palatine and pharyngeal area. Sometimes, one-sided coordination disorder of the entire body is observed.
- Damage to the facial nerve inside the cranium and the inner part of the temporal bone is characterized by paralysis of facial expressions, salivary glands. Signs such as thirst, changes in auditory function, drying of the ocular mucosa can be noticed.
Forms
- Congenital facial paralysis is associated with abnormal development of the brain during fetal development. This type of paralysis is characterized by a one- or two-sided mask-like facial expression on the affected side, a drooping corner of the mouth, and an open and moist eye slit. The skin on the cheek is smooth, and during exhalation the affected cheek seems to swell (the "sail" sign). The most severe form of congenital facial paralysis is Moebius syndrome.
- Peripheral facial nerve paralysis is the result of a disorder of the motor function of the nerve trunk. The pathology is accompanied by asymmetry, complete immobility of the muscles of the affected part of the face. The affected eye of the patient often does not close, except in cases of damage to the orbicularis muscle, when symmetrical closing of the eyes is possible.
- Central facial paralysis is the result of pathological changes in the cerebral cortex. The causes may be diseases affecting the cortico-nuclear pathways adjacent to the facial nerve. The most common localization of central paralysis is the lower part of the face. The disease manifests itself in involuntary muscle movements - a kind of tic, as well as convulsive attacks.
Complications and consequences
The restoration of nerve fibers after facial nerve paralysis occurs gradually, significantly slowing down during periods of stress, intoxication and hypothermia. This creates some difficulties in treatment: for example, many patients simply lose patience and hope and refuse further rehabilitation. If the paralysis is not cured, very unpleasant complications may arise.
- Muscle atrophy is the thinning and weakness of muscles due to long-term dysfunction and tissue trophism. This process is considered irreversible: atrophied muscles do not recover.
- Mimic contractures – loss of elasticity of muscles on the affected side, muscle spasms, spastic shortening of muscle fibers. Visually, the affected side of the face seems to be stretched, the eye squints.
- Facial muscle tics, spasmodic twitching are a disruption of impulse conduction along the nerve. This condition is also called hemispasm or blepharospasm.
- Associated movements – synkinesis – occur as a result of disruption of biocurrent isolation in the nerve trunk. As a result, excitation spreads to other innervation areas. An example of associated movements: while chewing food, the patient starts to cry, or the edge of the lips rises when squinting.
- Inflammation of the conjunctiva or cornea of the eye occurs because the patient cannot completely close the eye for a long period of time, which leads to its drying out.
Diagnostics facial nerve palsy
The diagnosis of facial nerve paralysis is established by a neurologist. This usually happens during the first examination of the patient, but in some cases additional studies may be required. Most often, diagnostics are used to clarify the causes of paralysis.
- First of all, the patient is prescribed tests - for example, a general blood test will indicate the presence of inflammation. Signs of an inflammatory process will be: increased ESR, leukocytosis, decreased lymphocyte count.
- Instrumental diagnostics may include the following procedures:
- MRI is a type of examination using a magnetic field and obtaining layered images. Thanks to magnetic resonance imaging, it is possible to identify tumor processes, vascular disorders, inflammatory changes in the meninges, and cerebral infarction.
- CT is a type of X-ray examination that can also detect such probable causes of the disease as tumors, post-stroke conditions, disturbances in perinuclear blood flow, and consequences of mechanical damage to the brain.
- The electroneurography method helps to determine the speed of nerve impulse passage. The results of this study help in determining the inflammatory process, damage to the nerve branch, muscle atrophy.
- The electromyography method is usually combined with the neurography procedure, determining the quality of intramuscular impulses. This allows detecting muscle atrophy and contractures.
Differential diagnosis
Differential diagnostics can be performed with stroke, Ramsay-Hunt syndrome, inflammatory processes in the middle ear or mastoid process, Lyme disease, temporal bone fractures, damage to the nerve trunk by carcinomatosis or leukemia, chronic meningitis, tumor processes, osteomyelitis, multiple sclerosis, and Guillain-Barré syndrome.
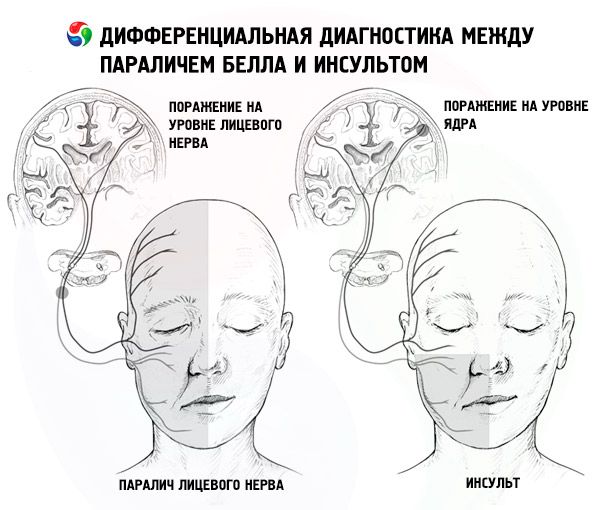
The difference between central and peripheral facial nerve paralysis
Some difficulties sometimes arise in differentiating between central and peripheral facial nerve paralysis.
First of all, attention is paid to the condition of the frontal row of muscles responsible for facial expressions. If they function without changes, and other facial muscles are motionless, then central localization of paralysis is assumed.
In this situation, we can talk about a variant with hemorrhage into the internal capsule: the process occurs with partial paralysis of the lower part of the nerve and a simultaneous one-sided feeling of weakness in the limbs. The sense of taste, the secretion of tears and saliva are normal.
From practice, it is quite difficult to distinguish between central and peripheral facial nerve paralysis, even for an experienced doctor. Therefore, the maximum possible amount of information about the patient and his disease should be used for diagnostics.

Who to contact?
Treatment facial nerve palsy
Medicines are prescribed immediately after the patient seeks medical help. It is with complex drug therapy that the main treatment of facial nerve paralysis begins.
Diuretics |
|||
Directions for use |
Side effects |
Special instructions |
|
Furosemide |
Take 40 mg orally in the morning. |
Nausea, diarrhea, skin reactions, decreased blood pressure, dizziness, dry mouth. |
Long-term use of the drug is not recommended. |
Veroshpiron |
Take 50-100 mg in the morning. |
Dyspepsia, lethargy, headache, drowsiness. |
The drug is incompatible with alcohol. |
Anti-inflammatory drugs |
|||
Directions for use |
Side effects |
Special instructions |
|
Nimesulide |
Orally 100 mg in the morning and at night with water. |
Headaches, apathy, dyspepsia, heartburn. |
Should not be used for long periods of time. |
Nurofen |
Take orally 0.2-0.8 g up to 4 times a day. |
Nausea, flatulence. |
It is recommended to wash down the drug with milk. |
Glucocorticoids |
|||
Directions for use |
Side effects |
Special instructions |
|
Prednisolone |
The average dosage is 5-60 mg per day. The drug is taken once a day, in the morning. |
Muscle weakness, indigestion, peptic ulcer, dizziness, high blood pressure. |
The drug is not prescribed for systemic fungal infections. |
Dexamethasone |
At the onset of the disease, 4-20 mg of the drug is administered intramuscularly up to 4 times a day. |
Nausea, cramps, headache, weight gain, allergies, flushing. |
The drug is discontinued gradually due to the risk of withdrawal syndrome. |
Antiviral drugs |
|||
Directions for use |
Side effects |
Special instructions |
|
Zovirax |
Take 200 mg 5 times a day for 5 days. |
Digestive disorders, headache, feeling of fatigue, allergic rash. |
During treatment with Zovirax, you should drink plenty of fluids. |
Acyclovir |
Take 200 mg 5 times a day for 5 days. |
Stomach pain, headache, drowsiness, allergies. |
The drug should not be taken for a long time. |
Antispasmodics |
|||
Directions for use |
Side effects |
Special instructions |
|
Spasmol |
Take 1-2 tablets up to 3 times a day. |
Increased heart rate, decreased blood pressure, dizziness, allergies. |
Not recommended for use in glaucoma and prostate hyperplasia. |
Drotaverine |
Take 40 to 80 mg three times a day. |
Low blood pressure, headache, nausea, allergies. |
The drug is not prescribed for severe liver and kidney diseases. |
Neurotropic drugs |
|||
Directions for use |
Side effects |
Special instructions |
|
Carbamazepine |
Take 100-400 mg orally up to 3 times a day. The dosage is increased gradually. |
Tremors in the limbs, depression, anxiety, allergies, digestive disorders. |
The drug is incompatible with alcohol. |
Diphenin |
Take on average 200-500 mg per day. |
Muscle weakness, dizziness, bowel disorder, nervousness. |
During treatment, the body's need for vitamin D may increase. |
Vitamin products |
|||
Directions for use |
Side effects |
Special instructions |
|
Pyridoxine |
It is administered intramuscularly in an amount of 50 to 150 mg per day. |
Sometimes – allergies, increased secretion of hydrochloric acid in the stomach. |
Requires caution in case of gastric ulcer and duodenal ulcer. |
Thiamine |
Administer intramuscularly once a day at 25-50 mg. Duration of therapy is 10-30 days. |
Allergies, sweating, increased heart rate. |
Injections may be painful. |
Cholinesterase inhibitors |
|||
Directions for use |
Side effects |
Special instructions |
|
Prozerin |
Take orally 10-15 mg up to 3 times a day. |
Nausea, headache, arrhythmia, shortness of breath. |
It is advisable to refrain from driving during treatment. |
Galantamine |
Take orally, in quantities from 8 to 32 mg in three doses, washed down with water. |
Fluctuations in blood pressure, swelling, thirst, dyspepsia, muscle spasms, urinary disorders. |
The drug is not prescribed for pathologies of the urinary system. |
Medicines are prescribed only by a doctor. Most often, treatment is carried out in a hospital, since it is very difficult to effectively treat facial nerve paralysis at home. In addition, this can lead to various negative consequences.
Physiotherapy treatment
Physiotherapy is used as an auxiliary but mandatory therapeutic method for facial nerve paralysis. The following physiotherapeutic procedures may be prescribed:
- UHF is heating of tissues using an electric field, which leads to improvement of trophic processes, removal of edema and inflammation. The duration of one UHF session is about 10 minutes. The treatment course usually consists of about 10 sessions, which are held every day or 3-4 times a week.
- UFO of the affected part of the face can be applied starting from about the 6th day from the onset of the disease. Ultraviolet activates the synthesis of hormones, improves the immune system, which has a positive effect on recovery. The treatment course can consist of 7-15 sessions.
- UHF therapy is the use of electromagnetic decimeter waves to activate metabolic processes in the affected facial tissues. The procedure lasts about 10 minutes. The course can be short (3-5 procedures) or standard (10-15 procedures).
- Electrophoresis with dibazol, vitamins, proserin is the effect of certain doses of electric current, with the help of which the drug manages to penetrate into the affected tissues. The duration of one electrophoresis session is about 20 minutes. The duration of treatment is from 10 to 20 sessions.
- Diadynamic currents help restore muscle function by causing their spastic contraction. At the same time, swelling is removed and nerve fibers are restored. Treatment is usually long-term: 10 to 30 procedures may be needed for recovery.
- Paraffin or ozokerite applications accelerate the regeneration process and promote faster recovery. The application is applied for 30-40 minutes. About 15 procedures may be required to restore innervation in case of facial nerve paralysis.
After each physiotherapy session, it is important to protect your face from drafts and cold, as a sharp change in temperature can aggravate the inflammatory process.
Massage treatments for facial nerve paralysis
Massage for facial nerve paralysis is considered very effective, but it is performed bypassing the acute period of the disease. The first massage sessions are prescribed no earlier than a week after the onset of the disease. What is therapeutic massage for facial nerve paralysis?
- The massage procedure begins with warming up and kneading the neck muscles, using slow bends and rotations of the neck;
- then massage the occipital region, thereby increasing lymph flow;
- massage the scalp;
- move on to massage of the face and temples;
- important: massage movements should be light and shallow, so as not to provoke muscle spasms;
- it is good to use stroking and relaxing movements;
- stroking is carried out along the lymphatic vessels;
- the face is massaged from the central line to the periphery;
- avoid massaging the areas where lymph nodes are located;
- massage the inside of the cheek using your thumb;
- At the end of the procedure, the neck muscles are massaged again.
The massage procedure should last no more than 15 minutes. The total duration of the course is until the patient is completely cured.
Special gymnastics
Gymnastics for facial nerve paralysis consists of a set of exercises to warm up the cervical spine and shoulder area. The patient is seated in front of a mirror so that he can see his reflection. This guarantees the quality of the exercises performed.
During the exercise, the face should be relaxed. Do 5 repetitions of each of the following exercises:
- the patient raises and lowers his eyebrows;
- frowns;
- looks down as much as possible while closing his eyes;
- squints;
- moves eyeballs in a circle;
- smiles with pursed lips;
- raises and lowers the upper lip, showing the upper row of teeth;
- lowers and raises the lower lip, demonstrating the lower row of teeth;
- smiles with his mouth open;
- presses his chin to his chest and snorts;
- moves nostrils;
- tries to puff out his cheeks, alternately and simultaneously;
- takes in air and blows it out, pursing his lips into a “tube”;
- tries to whistle;
- sucks in cheeks;
- lowers and raises the corners of the lips;
- lifts the lower lip onto the upper, then places the upper lip onto the lower;
- makes movements with the tongue while keeping the lips closed and open.
If any exercise does not work, it is recommended to relax and make stroking movements with your fingertips on the affected part of the face.
Typically, the suggested series of exercises is repeated up to 3 times a day.
Homeopathic Remedies for Facial Nerve Paralysis
Homeopathy also offers a number of remedies that can help speed up recovery from facial paralysis. Homeopathic remedies should not be the mainstay of therapy, but they can enhance the effects of other treatments. Below is more information on the remedies that homeopaths offer to help relieve facial paralysis.
- Traumeel C is an injection drug in ampoules. Usually 1-2 ampoules are prescribed 1 to 3 times a week as intramuscular injections. The duration of therapy is at least 1 month. Combined use with Traumeel ointment and tablets is possible.
The drug rarely causes allergies, but redness and slight swelling may occur at the injection site. In such a situation, a doctor's consultation is recommended.
- Nervoheel is a homeopathic medicine that improves the functioning of the nervous system, promotes functional renewal of nerve fibers, eliminates the effects of stress and fatigue. The medicine is taken 1 tablet three times a day, dissolving under the tongue half an hour before meals. Treatment continues for about 3 weeks. Features of the use of the medicine: during the first week of taking Nervoheel, a temporary deterioration in the condition is possible, which is considered a normal variant.
- Girel is a drug used for facial nerve paralysis, which is a consequence of viral infectious diseases. Girel is taken 1 tablet three times a day, dissolving under the tongue. The duration of administration is calculated by the doctor.
- Valerianaheel is a sedative that can be used for neuroses, neuropathies, and neurasthenia. Taking this drug can serve as an excellent preventative measure against facial nerve paralysis relapses. The drug is prescribed 15 drops with ½ glass of clean water, three times a day half an hour before meals. Continue taking for 20-30 days.
Surgical treatment
The doctor may resort to surgical intervention if drug treatment does not have the expected effect within 9 months. Before this period, it is not worth prescribing surgery, since the drugs can still have a positive effect. If more than 1 year passes, then surgical treatment is no longer meaningful, since by this time atrophic changes in muscle tissue have already occurred, which cannot be restored.
In most cases, surgical intervention is used for nerve ischemia, which develops as a result of chronic otitis or after head injuries. Surgery is also appropriate for mechanical rupture of a nerve branch.
To summarize, the following situations with facial nerve paralysis can be identified in which the help of a surgeon may be required:
- traumatic rupture of the nerve trunk;
- ineffectiveness of the drug treatment administered over a period of approximately 9 months;
- tumor processes.
How is the operation performed?
- When the facial nerve is compressed, the intervention is carried out as follows:
- an incision is made behind the ear;
- the place where the nerve exits the stylomastoid foramen is highlighted;
- the outer wall of the hole is expanded using special devices;
- stitches are applied.
General anesthesia is used for the operation.
- To suture a nerve trunk damaged by rupture, the following surgical manipulations are performed:
- an incision is made behind the ear;
- under the skin, the ends of the torn nerve trunk are found, which are cleaned for better fusion;
- the ends are sewn together immediately or first passed along another, shorter path;
- In some cases, a nerve transplant from another part of the body, such as a lower limb, may be necessary.
The operation is quite complicated, but the rehabilitation period is usually short.
Folk remedies
- It is useful to apply compresses from puree based on elderberries. Berries are steamed and ground, spread on the surface of a clean cloth and applied as a compress to the affected part of the face for half an hour. The procedure is carried out twice a day.
- A good effect is expected from regular consumption of dates with milk, which are eaten three times a day, 6 pieces at a time. Duration of treatment is 1 month.
- Fill your mouth with warm water with a few drops of valerian tincture added. Keep the medicine in your mouth for 3-4 minutes without swallowing.
- Take mumijo in the morning, afternoon and at night, 0.2 g, for 10 days. Repeat the intake after another 10 days. Usually three such courses are enough for a cure.
In addition, you can also use herbal treatment according to the following recipes.
- Take 100 g of sage herb, pour 1 glass of hot water and leave overnight. Drink 1 teaspoon between meals, washing it down with milk.
- Prepare an equal mixture of valerian rhizome, oregano, yarrow and mistletoe. Prepare an infusion at the rate of 1 tbsp. of the mixture per glass of water. Drink the medicine 100 ml three times a day 20 minutes before meals.
- Prepare an equal mixture of mint, lemon balm, oregano, thyme, mistletoe, motherwort. Pour 1 tbsp of the mixture with 200 ml of boiling water, leave for an hour and take 100 ml twice a day between meals.
- Take 1 tbsp. of betony herb, pour 200 ml of boiling water and leave for 2 hours. Drink the medicine 60 ml up to 4 times a day.
Prevention
To prevent repeated relapses of facial nerve paralysis, special prevention methods can be used. To do this, it is enough to use the following useful tips:
- do not allow your face and head to become excessively cold, dress according to the weather, avoid drafts;
- do not ignore treatment for colds and viral diseases, take appropriate medications in time at the first signs of illness;
- take care of your nervous system, don’t get nervous, avoid unpleasant conversations and scandals;
- rest properly: it is advisable to spend time in nature, swim, and engage in active sports;
- eat right, avoid strict diets, eat enough plant foods;
- Take a course of multivitamin preparations with B vitamins twice a year, which are essential for the normal functioning of nerve cells and fiber conductivity;
- maintain your immunity, toughen up, take air baths;
- Massage your face periodically, morning and night, using light stroking movements.
Forecast
Most cases of facial nerve paralysis heal spontaneously within 1.5-2 months. In elderly patients, such statistics have a less favorable prognosis: paralysis can persist in 40-60% of cases.
The outcome of the disease can be predicted by taking into account the degree of nerve damage: the more severe this damage is, the longer the recovery will be. In severe cases, if the patient seeks medical help late, the signs of the disease may persist for a long time, or for life.
Peripheral facial nerve paralysis usually has a more favorable course, in contrast to central damage.

